Содержание
- 3. These measurements indicate if the circulatory, pulmonary, neurological, and endocrine body systems are functioning normally. Because
- 5. 1 A nurse caring for a patient is responsible for measuring vital signs. Nurses analyze vital
- 6. 5 Control or minimize environmental factors that affect vital signs. For example, assessing the patient’s temperature
- 8. Its main job is to pump blood to different body parts so that oxygen and other
- 9. The pulse can be felt anywhere an artery close to your skin such as: Your wrist
- 11. For trained athletes and people who are physically active, a heart rate lower than 60 beats
- 13. In order to palpate for a radial pulse, follow these steps: 1. Turn your one hand
- 15. In adults, the normal respiratory rate range from 10 to 20 breaths per minute while it
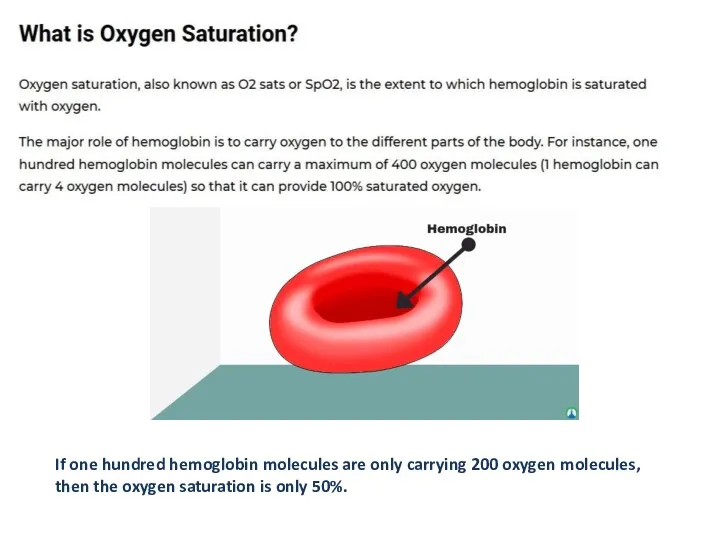
- 17. If one hundred hemoglobin molecules are only carrying 200 oxygen molecules, then the oxygen saturation is
- 18. In healthy adults and children, normal oxygen saturation ranges from 95% to 100%. For people with
- 21. For instance, the blood pressure reading is 120/80 mmHg. 120 is the systolic reading while 80
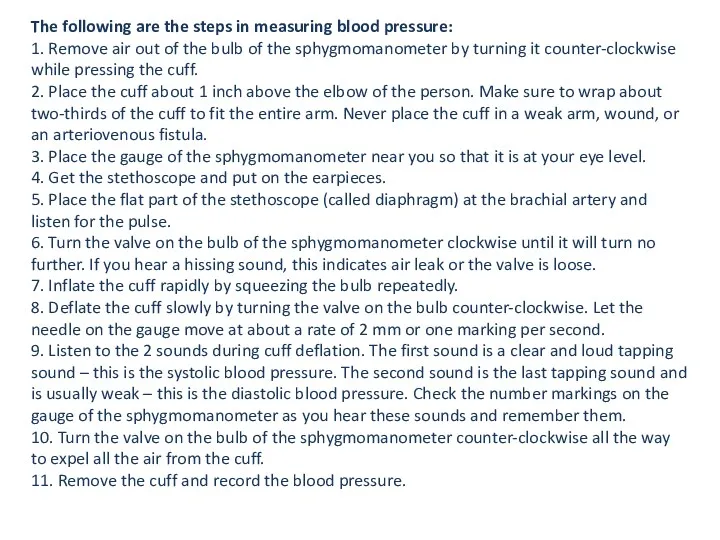
- 22. The following are the steps in measuring blood pressure: 1. Remove air out of the bulb
- 23. The average body temperature is 36.5 to 37.5 degrees Celsius or 98.6 degrees Fahrenheit. Certain factors
- 29. Скачать презентацию
These measurements indicate if the circulatory, pulmonary, neurological, and endocrine body
Because of their importance as indicators of the body’s physiological status and response to physical, environmental, and psychological stressors, they are referred to as vital signs.
Vital signs reveal sudden changes in a patient’s condition, as well as changes that occur progressively over time.
Any difference between a patient’s normal baseline measurement and present vital
signs may indicate the need for nursing therapies and necessary medical interventions.
You will frequently perform assessment of a patient’s level of comfort and pain with vital sign measurements.
1 A nurse caring for a patient is responsible for measuring
1 A nurse caring for a patient is responsible for measuring
signs. Nurses analyze vital signs to interpret their significance
and make decisions about appropriate interventions.
2 Equipment must be clean, functional, properly calibrated,
and appropriate for the patient’s size, age, condition, and
characteristics.
3 A nurse knows a patient’s usual range of vital signs. His or her
usual values may differ from the acceptable range for that age
or physical state. They serve as a baseline for comparison with
later findings; thus you detect changes in condition over time.
4 A nurse knows a patient’s medical history, therapies, and prescribed
medications. Some illnesses or treatments cause predictable
vital sign changes. Most medications affect at least one of
the vital signs.
5 Control or minimize environmental factors that affect vital
signs. For example,
5 Control or minimize environmental factors that affect vital
signs. For example,
warm, humid room may yield a value that is not a true indicator
of the patient’s condition.
6 Use an organized, systematic (step-by-step) approach when
taking vital signs ensures accuracy of findings.
7 Based on the patient’s condition, collaborate with the health
care provider to decide the minimum frequency of vital sign
assessment for each patient. Following surgery or treatment
intervention, measure vital signs more frequently to detect complications.
In a clinic or outpatient setting take vital signs before the health care provider examines the patient and after any invasive procedures. As a patient’s physical condition worsens, it is important to monitor the vital signs as often as every 5 to
15 minutes.
You are responsible for judging whether more frequent assessments are necessary.
Its main job is to pump blood to different body parts
Its main job is to pump blood to different body parts
Normally, a heartbeat has two sounds: “lub” and “dub”. A lub sound is created when the upper chambers of your heart contract to squeeze the blood down to your ventricles.
This, in turn, causes the lower chambers of your heart to contract pushing blood upward into the aorta (largest artery), resulting in a dub sound.
The blood from each contraction of your heart creates a bulge in the artery. This bulge is the pulse you feel.
The pulse can be felt anywhere an artery close to your
The pulse can be felt anywhere an artery close to your
Your wrist (radial)
Inner part of your elbow (brachial)
Side of your throat (carotid)
Temple (temporal)
Groin (femoral)
Back of your knee (popliteal)
Inner part of your ankle joint (posterior tibial)
Foot (dorsalis pedis)
Your pulse rate is exactly equal to your heartbeat because the contractions that your heart creates increase the pressure within your arteries that lead to a palpable pulse. Therefore, checking for your pulse rate is a direct measure of your heart rate.
For trained athletes and people who are physically active, a heart
For trained athletes and people who are physically active, a heart
The same goes for a resting heart rate above normal.
In order to palpate for a radial pulse, follow these steps:
1.
In order to palpate for a radial pulse, follow these steps:
1.
2. Use your free hand to place your point and middle finger gently below your wrist about an inch along from the base of the thumb. Never use your thumb to check for a pulse because it has its own pulse that you may feel, resulting in an inaccurate result.
3. Adjust your point and middle finger until you feel a strong pulse. Do not put too much pressure on your radial artery as it can impede blood flow.
4. Using a watch or a digital timer, count your pulse for one minute. Another way to do this is to count the number of beats for 15 seconds and then multiply it by 4 to get your total beats in a minute. However, this method is not recommended for people with underlying heart disease because the pattern of their pulses might be different (there might be an additional pulse in the first 15 seconds and it can fade in the next 15 seconds). Therefore, counting the pulse for a full minute is recommended in people with heart disease.
In adults, the normal respiratory rate range from 10 to 20
In adults, the normal respiratory rate range from 10 to 20
If one hundred hemoglobin molecules are only carrying 200 oxygen molecules,
If one hundred hemoglobin molecules are only carrying 200 oxygen molecules,
In healthy adults and children, normal oxygen saturation ranges from 95%
In healthy adults and children, normal oxygen saturation ranges from 95%
Oxygen saturation levels are dependent upon several factors such as the following:
Ability of hemoglobin to carry oxygen molecules.
Gas exchange in the lungs.
Oxygen availability.
The concentration of hemoglobin in red blood cells.
For instance, the blood pressure reading is 120/80 mmHg. 120 is
For instance, the blood pressure reading is 120/80 mmHg. 120 is
Like all other vital signs, the blood pressure reading can be affected by activity levels, stress, diet, medications, and underlying medical conditions.
The following are the steps in measuring blood pressure:
1. Remove air
The following are the steps in measuring blood pressure:
1. Remove air
2. Place the cuff about 1 inch above the elbow of the person. Make sure to wrap about two-thirds of the cuff to fit the entire arm. Never place the cuff in a weak arm, wound, or an arteriovenous fistula.
3. Place the gauge of the sphygmomanometer near you so that it is at your eye level.
4. Get the stethoscope and put on the earpieces.
5. Place the flat part of the stethoscope (called diaphragm) at the brachial artery and listen for the pulse.
6. Turn the valve on the bulb of the sphygmomanometer clockwise until it will turn no further. If you hear a hissing sound, this indicates air leak or the valve is loose.
7. Inflate the cuff rapidly by squeezing the bulb repeatedly.
8. Deflate the cuff slowly by turning the valve on the bulb counter-clockwise. Let the needle on the gauge move at about a rate of 2 mm or one marking per second.
9. Listen to the 2 sounds during cuff deflation. The first sound is a clear and loud tapping sound – this is the systolic blood pressure. The second sound is the last tapping sound and is usually weak – this is the diastolic blood pressure. Check the number markings on the gauge of the sphygmomanometer as you hear these sounds and remember them.
10. Turn the valve on the bulb of the sphygmomanometer counter-clockwise all the way to expel all the air from the cuff.
11. Remove the cuff and record the blood pressure.
The average body temperature is 36.5 to 37.5 degrees Celsius or
The average body temperature is 36.5 to 37.5 degrees Celsius or












 Спортивный травматизм
Спортивный травматизм Особенности спектра вторичных заболеваний и их клинического течения у детей с ВИЧ-инфекцией Часть 2
Особенности спектра вторичных заболеваний и их клинического течения у детей с ВИЧ-инфекцией Часть 2 Сенильді психоздың дамуына әкелетін факторлар. Кәрі жастағы психикалық бұзылыстары бар науқастардың реабилитациясы
Сенильді психоздың дамуына әкелетін факторлар. Кәрі жастағы психикалық бұзылыстары бар науқастардың реабилитациясы Зелёная аптека
Зелёная аптека Інсульт. Причини, симптоми інсульту, перша допомога, поради
Інсульт. Причини, симптоми інсульту, перша допомога, поради Грипп. Возбудители гриппа
Грипп. Возбудители гриппа Угарный газ. Патологическая физиология и анатомия отравления. Судебно-медицинское значение
Угарный газ. Патологическая физиология и анатомия отравления. Судебно-медицинское значение Основы клинической физиологии сердца
Основы клинической физиологии сердца Особая профессия – дефектолог-логопед
Особая профессия – дефектолог-логопед Медицина_Podgotovka_k_ekz
Медицина_Podgotovka_k_ekz Оказание первой помощи
Оказание первой помощи Синдром Иценко-Кушинга
Синдром Иценко-Кушинга Тісті тікелей қалпына келтіру.Қолданылатын материалдар
Тісті тікелей қалпына келтіру.Қолданылатын материалдар Средства для наркоза. Этиловый спирт
Средства для наркоза. Этиловый спирт Фибрилляция предсердий
Фибрилляция предсердий Орбитаның жаңа түзілістері
Орбитаның жаңа түзілістері Материнская смертность
Материнская смертность Мамандандырылған медициналық жәрдемді ұйымдастыру
Мамандандырылған медициналық жәрдемді ұйымдастыру Закрытые механические травмы
Закрытые механические травмы Противоглистные и противопротозойные средства
Противоглистные и противопротозойные средства Первая помощь при ранениях, кровотечениях и шоке. Тема № 6
Первая помощь при ранениях, кровотечениях и шоке. Тема № 6 Сердечно-легочная реанимация
Сердечно-легочная реанимация Преждевременные роды
Преждевременные роды Экстрапирамидная система, синдромы поражения
Экстрапирамидная система, синдромы поражения 1 и 2 меридианы в рефлексотерапии. Точечный массаж (акупрессура)
1 и 2 меридианы в рефлексотерапии. Точечный массаж (акупрессура) Патофизиологический эксперимент
Патофизиологический эксперимент Омолаживающая ионотерапия с биозолотом. Lacrima
Омолаживающая ионотерапия с биозолотом. Lacrima Регенерация. Виды репаративной регенерации
Регенерация. Виды репаративной регенерации