Содержание
- 2. Zika virus epidemiology Diagnoses and testing Case reporting Zika and pregnancy Clinical management of infants Sexual
- 3. ZIKA VIRUS EPIDEMIOLOGY
- 4. Single stranded RNA virus Genus flavivirus, family Flaviviridae Closely related to dengue, yellow fever, Japanese encephalitis,
- 5. Before 2015, Zika outbreaks occurred in Africa, Southeast Asia, and the Pacific Islands. Currently is a
- 6. Bite from an infected mosquito Maternal-fetal Periconceptional Intrauterine Perinatal Sexual transmission from an infected person to
- 7. Zika may be spread through blood transfusion. Zika virus has been detected in breast milk. There
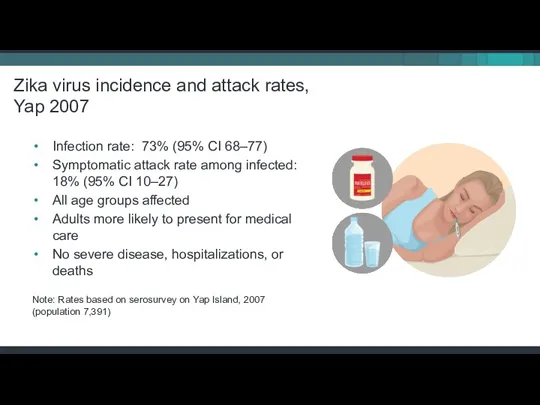
- 8. Infection rate: 73% (95% CI 68–77) Symptomatic attack rate among infected: 18% (95% CI 10–27) All
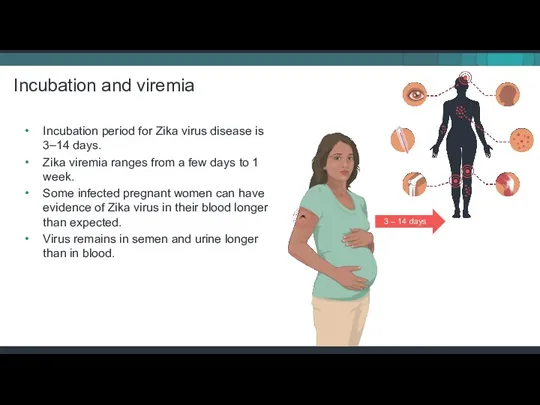
- 9. Incubation period for Zika virus disease is 3–14 days. Zika viremia ranges from a few days
- 10. Clinical illness is usually mild. Symptoms last several days to a week. Severe disease requiring hospitalization
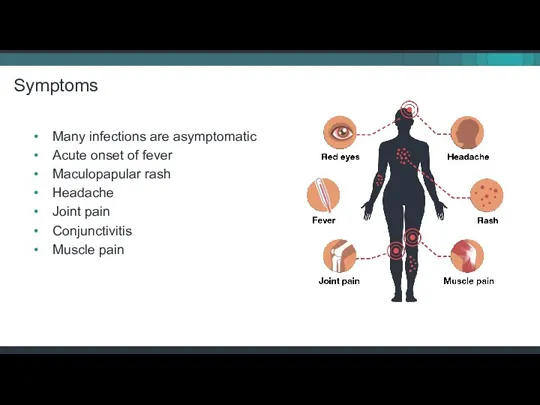
- 11. Many infections are asymptomatic Acute onset of fever Maculopapular rash Headache Joint pain Conjunctivitis Muscle pain
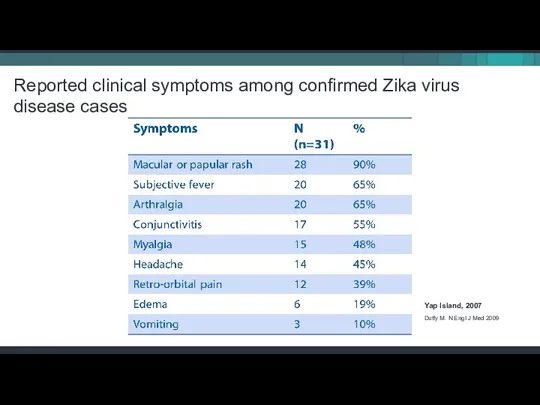
- 12. Reported clinical symptoms among confirmed Zika virus disease cases Yap Island, 2007 Duffy M. N Engl
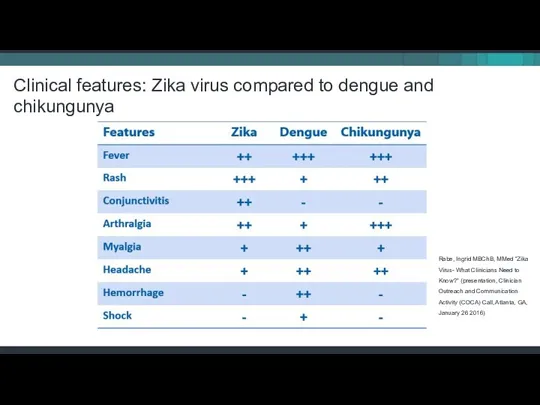
- 13. Clinical features: Zika virus compared to dengue and chikungunya Rabe, Ingrid MBChB, MMed “Zika Virus- What
- 14. DIAGNOSES AND TESTING FOR ZIKA
- 15. All pregnant women should be asked at each prenatal care visit if they Traveled to or
- 16. Who to test for Zika Anyone who has or recently experienced symptoms of Zika and lives
- 17. Diagnostic testing for Zika virus During first 2 weeks after the start of illness (or exposure,
- 18. Differential diagnosis Dengue Chikungunya Leptospirosis Malaria Riskettsia Group A Streptococcus Rubella Measles Parvovirus Enterovirus Adenovirus Other
- 19. Serology cross-reactions with other flaviviruses Zika virus serology (IgM) can be positive due to antibodies against
- 20. Testing for infants CDC recommends laboratory testing for All infants born to mothers with laboratory evidence
- 21. Laboratories for diagnostic testing Testing performed at CDC, select commercial labs, and a few state health
- 22. REPORTING ZIKA CASES
- 23. Zika virus disease is a nationally notifiable condition. Report all confirmed cases to your state health
- 24. CDC is monitoring pregnancy and infant outcomes following Zika infection during pregnancy in US states and
- 25. ZIKA AND PREGNANCY
- 26. Knowledge about Zika virus is increasing rapidly and researchers continue to work to better understand the
- 27. Testing guidance: Pregnant women with possible Zika exposure
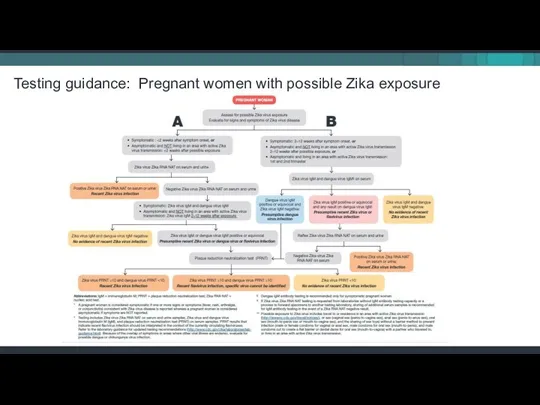
- 28. Clinical management of a pregnant woman with suspected Zika virus infection
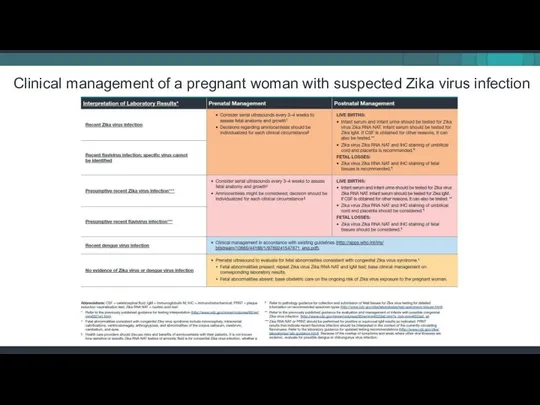
- 29. EVALUATION AND FOLLOW UP OF INFANTS WITH CONFIRMED OR POSSIBLE ZIKA INFECTION
- 30. Zika virus infection during pregnancy is a cause of microcephaly and other severe birth defects. All
- 31. Congenital Zika syndrome is associated with five types of birth defects that are either not seen
- 32. Case definition of microcephaly Definite congenital microcephaly for live births Head circumference (HC) at birth is
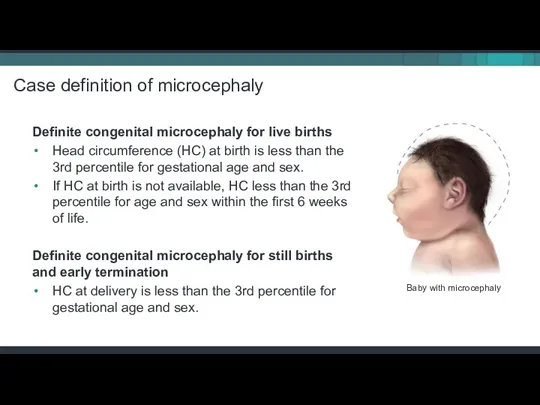
- 33. Definitions for possible congenital microcephaly Possible congenital microcephaly for live births If earlier HC is not
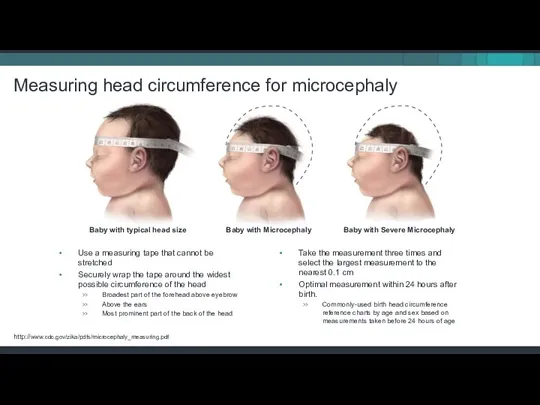
- 34. Measuring head circumference for microcephaly Use a measuring tape that cannot be stretched Securely wrap the
- 35. It’s important to remember that even in places with Zika, women are delivering infants that appear
- 36. Infants born to potentially exposed mothers who were not tested before delivery, or who were tested
- 37. Interim Guidance: Evaluation and testing of infants with possible congenital Zika virus infection
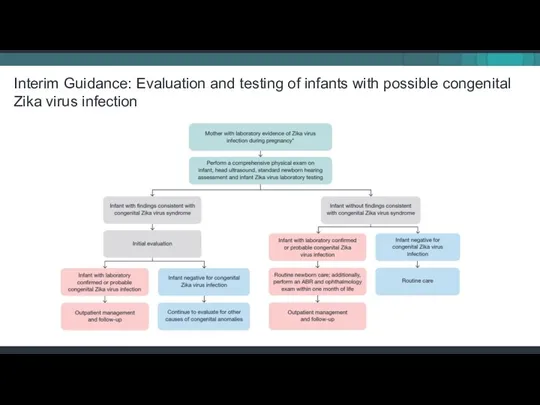
- 38. Consultation with Neurologist - determination of appropriate neuroimaging and evaluation Infectious disease specialist - diagnostic evaluation
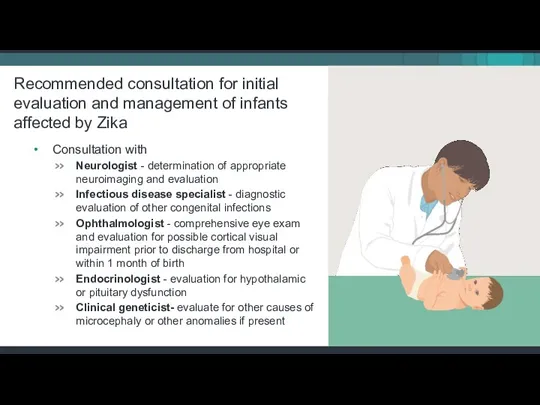
- 39. Consider consultation with Orthopedist, physiatrist, and physical therapist for the management of hypertonia, club foot, or
- 41. Pediatric evaluation and follow up tools Download at: http://www.cdc.gov/zika/pdfs/pediatric-evaluation-follow-up-tool.pdf
- 42. SEXUAL TRANSMISSION
- 43. Zika can be passed through sex from a person who has Zika to his or her
- 44. We know that Zika can remain in semen longer than in other body fluids, including vaginal
- 45. CDC and other public health partners continue research that may help us find out How long
- 46. Not having sex eliminates the risk of getting Zika from sex. Condoms can reduce the chance
- 47. Men and women with possible Zika exposure Decorative image People with a partner who traveled to
- 48. PRECONCEPTION GUIDANCE
- 49. Testing is NOT recommended for asymptomatic couples in which one or both partners has had possible
- 50. Women and men interested in conceiving should talk with their healthcare providers. Factors that may aid
- 51. For women with possible exposure to an area with a CDC Zika travel notice Discuss signs
- 52. For men with possible exposure to with a CDC Zika travel notice Wait at least 6
- 53. For couples with exposure to areas with risk of Zika but no CDC Zika travel notice
- 54. INFECTION CONTROL IN HEALTHCARE SETTINGS
- 55. Standard Precautions should be used to protect healthcare personnel from all infectious disease transmission, including Zika
- 56. Healthcare personnel should assess the likelihood of the presence of body fluids or other infectious material
- 57. WHAT TO TELL PATIENTS ABOUT ZIKA
- 58. Pregnant women should not travel to areas with risk of Zika. If they must travel to
- 59. There is no vaccine or medicine for Zika. Treat the symptoms of Zika Rest Drink fluids
- 60. Protect from mosquito bites during the first week of illness, when Zika virus can be found
- 61. Wear long-sleeved shirts and long pants. Stay and sleep in places with air conditioning and window
- 62. Use Environmental Protection Agency (EPA)-registered insect repellents with one of the following active ingredients: DEET, picaridin,
- 63. Preventing Zika: Mosquito bite protection Do not use insect repellent on babies younger than 2 months
- 65. Скачать презентацию


 Дифференциальная диагностика высыпаний на лице
Дифференциальная диагностика высыпаний на лице Период младшего школьного возраста
Период младшего школьного возраста Оперативный доступ к кровеносным сосудам верхней конечности
Оперативный доступ к кровеносным сосудам верхней конечности Асептика. Профилактика воздушно-капельной инфекции
Асептика. Профилактика воздушно-капельной инфекции Антифосфолипидный синдром
Антифосфолипидный синдром Геномная медицина и стоматология
Геномная медицина и стоматология Организмнің реактивтілігі мен резистенттілігінің патологиядағы маңызы
Организмнің реактивтілігі мен резистенттілігінің патологиядағы маңызы Reconstruction préprothétique par technique directe. Restaurer la dent deulpe
Reconstruction préprothétique par technique directe. Restaurer la dent deulpe Беременность с преждевременным излитием околоплодных вод
Беременность с преждевременным излитием околоплодных вод Рак предстательной железы
Рак предстательной железы Tumors of genitourinary organs
Tumors of genitourinary organs Спирамицин. Способ применения и дозы
Спирамицин. Способ применения и дозы Гипотензивные средства (антигипертензивные средства)
Гипотензивные средства (антигипертензивные средства)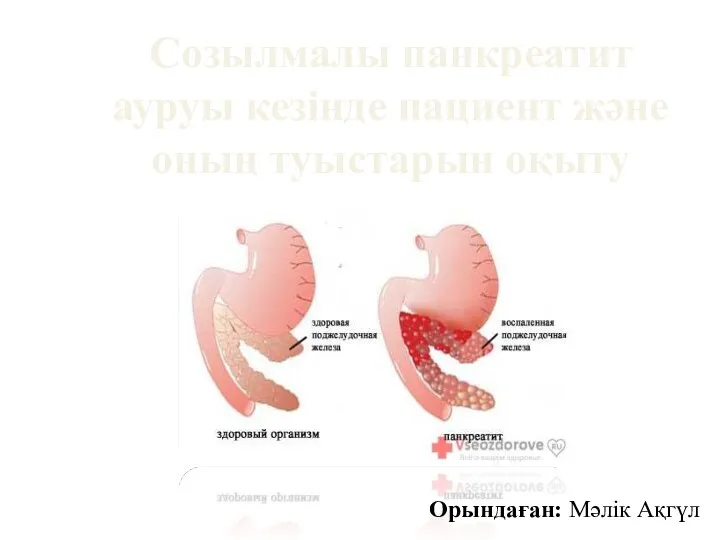 Созылмалы панкреатит ауруы кезінде пациент және оның туыстарын оқыту
Созылмалы панкреатит ауруы кезінде пациент және оның туыстарын оқыту Туберкулёз. Профилактика. Лечение
Туберкулёз. Профилактика. Лечение Pros of using AI in medicine
Pros of using AI in medicine Есту және тепе-теңдік мүшесі
Есту және тепе-теңдік мүшесі Геморрагический инсульт
Геморрагический инсульт Өмір сүру дағдысының екіншілік ИЖЖ қалыптасуындағы рөлі
Өмір сүру дағдысының екіншілік ИЖЖ қалыптасуындағы рөлі Приказ об утверждении перечня состояний при которых оказывается первая помощь, и перечня мероприятий по оказанию первой помощи
Приказ об утверждении перечня состояний при которых оказывается первая помощь, и перечня мероприятий по оказанию первой помощи Смерть мозга
Смерть мозга Внутриутробные инфекции плода и новорождённого
Внутриутробные инфекции плода и новорождённого Судебно-медицинская экспертиза трупов неизвестных лиц
Судебно-медицинская экспертиза трупов неизвестных лиц The Skeletal System
The Skeletal System Interruption volontaire de grossesse (17 janvier 1975)
Interruption volontaire de grossesse (17 janvier 1975) Ранний детский аутизм
Ранний детский аутизм Пороки сердца
Пороки сердца Этическое отношение к искусственному размножению
Этическое отношение к искусственному размножению