Содержание
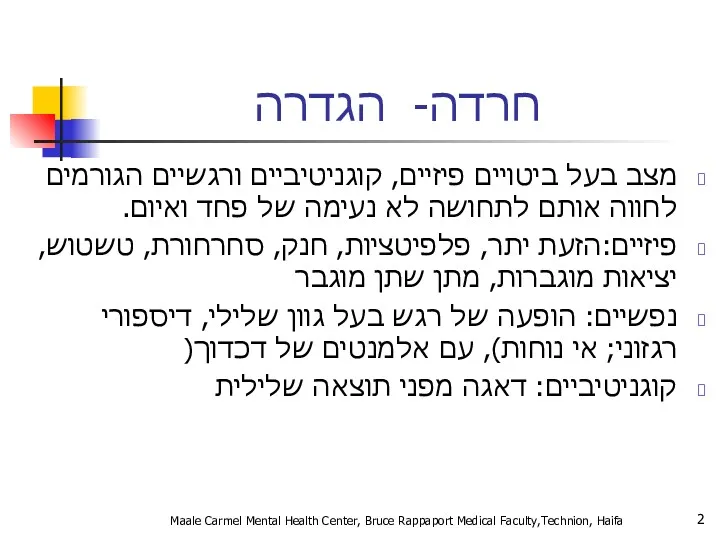
- 2. חרדה- הגדרה מצב בעל ביטויים פיזיים, קוגניטיביים ורגשיים הגורמים לחווה אותם לתחושה לא נעימה של פחד
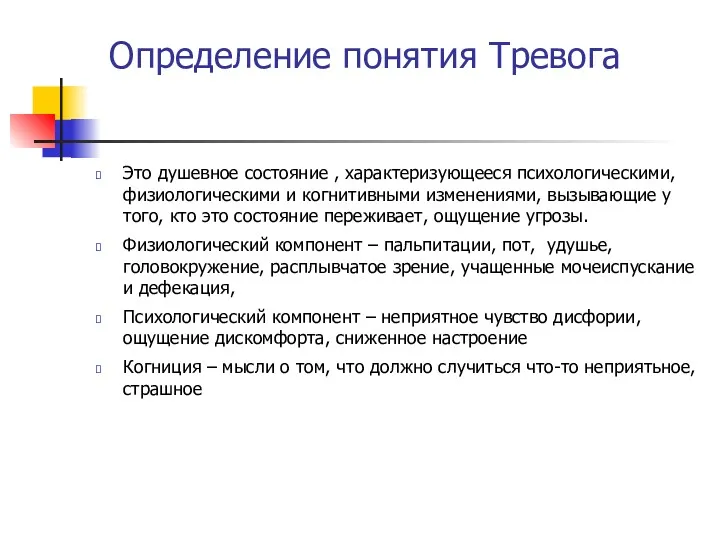
- 3. Определение понятия Тревога Это душевное состояние , характеризующееся психологическими, физиологическими и когнитивными изменениями, вызывающие у того,
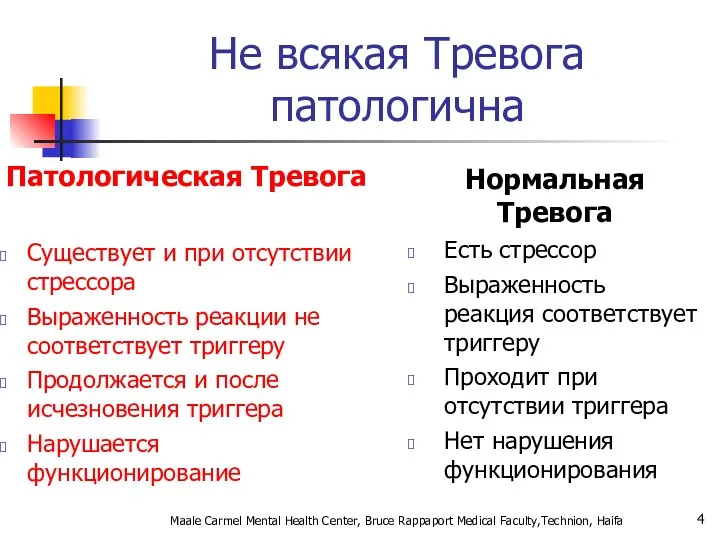
- 4. Maale Carmel Mental Health Center, Bruce Rappaport Medical Faculty,Technion, Haifa Не всякая Тревога патологична Патологическая Тревога
- 5. Tirat Carmel Mental Health Center, Bruce Rappaport Medical Faculty,Technion, Haifa
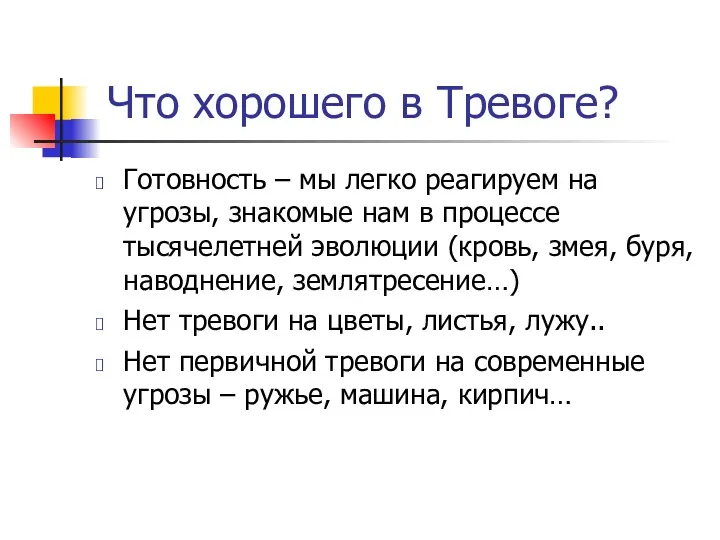
- 6. תפקידה החיובי של חרדה מוכנות- אנו נוטים להגיב יותר לאיומים המוכרים לנו מאלפי שנות אבולוציה (נחש,
- 7. Что хорошего в Тревоге? Готовность – мы легко реагируем на угрозы, знакомые нам в процессе тысячелетней
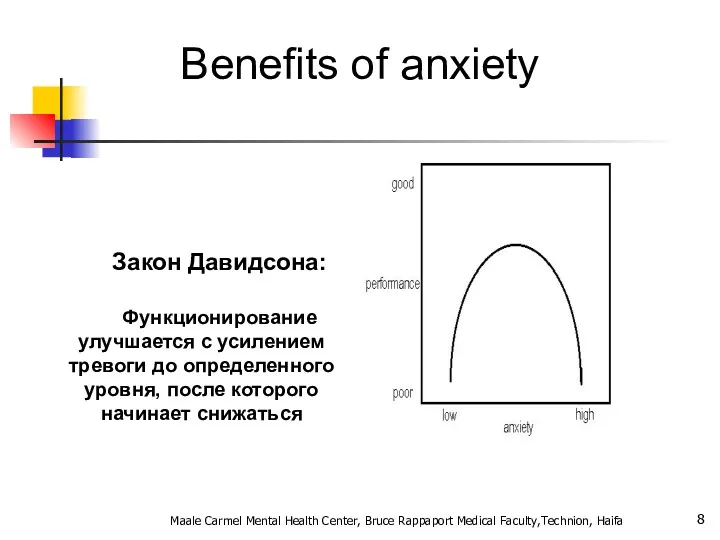
- 8. Benefits of anxiety Закон Давидсона: Функционирование улучшается с усилением тревоги до определенного уровня, после которого начинает
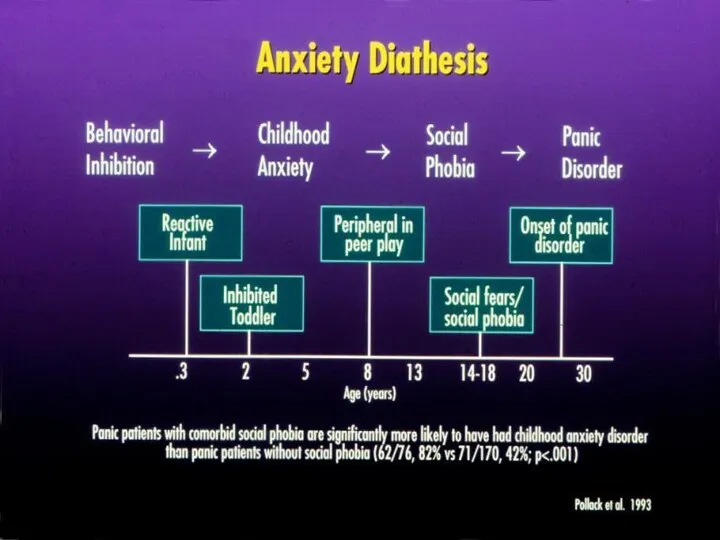
- 9. General considerations for anxiety disorders Often have an early onset- teens or early twenties Show 2:1
- 10. The differential diagnosis of anxiety. Psychiatric and Medical disorders. Psychiatr Clin North Am 1985 Mar;8(1):3-23 Primary
- 11. What characteristics of primary anxiety disorders predict subsequent major depressive disorder. J Clin Psychiatry 2004 May;65(5):618-25
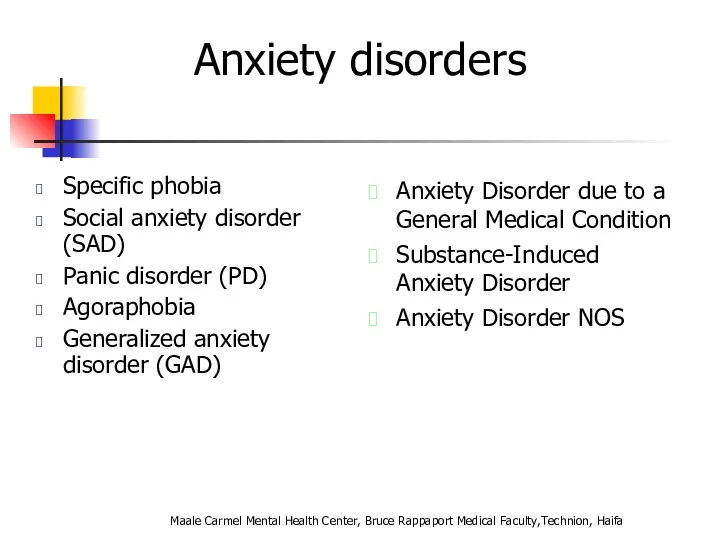
- 12. Anxiety disorders Specific phobia Social anxiety disorder (SAD) Panic disorder (PD) Agoraphobia Generalized anxiety disorder (GAD)
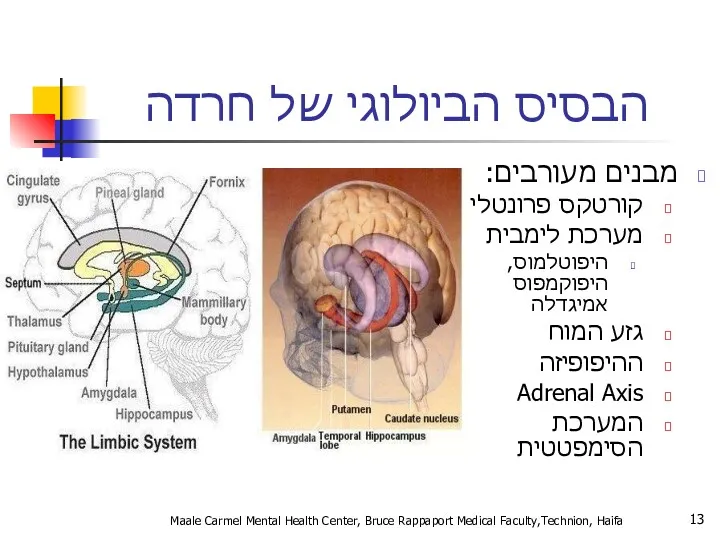
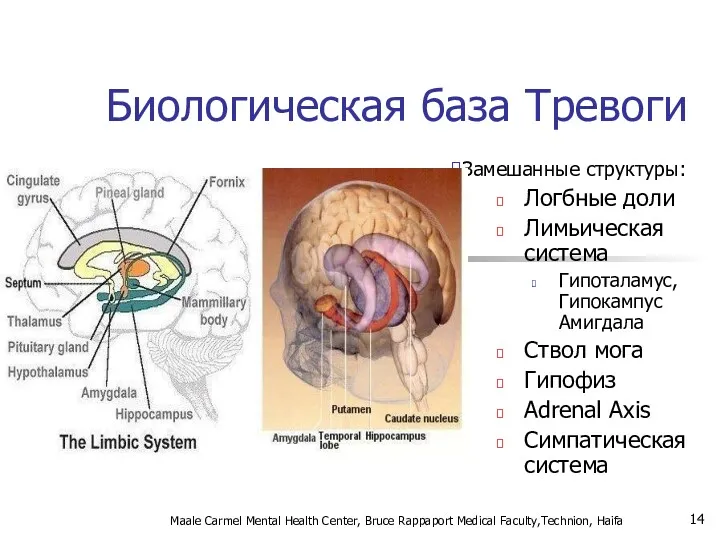
- 13. הבסיס הביולוגי של חרדה מבנים מעורבים: קורטקס פרונטלי מערכת לימבית היפוטלמוס, היפוקמפוס אמיגדלה גזע המוח ההיפופיזה
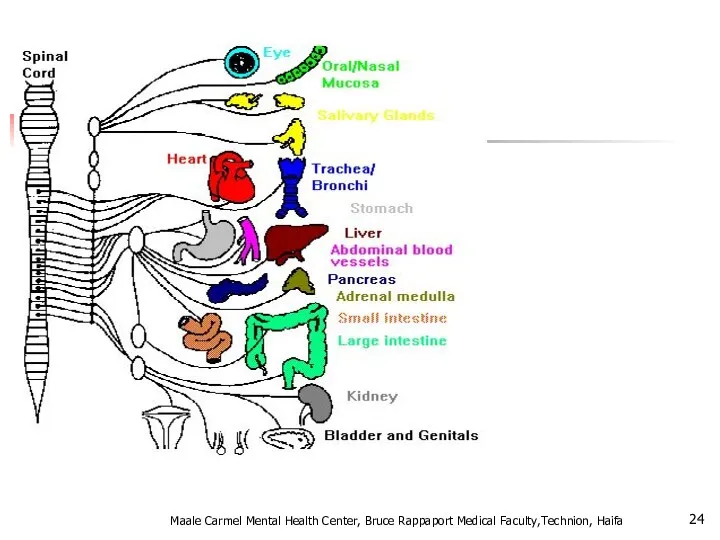
- 14. Биологическая база Тревоги Замешанные структуры: Логбные доли Лимьическая система Гипоталамус, Гипокампус Амигдала Ствол мога Гипофиз Adrenal
- 15. חרדה- מודלים ביולוגיים אמנם המחקר העכשווי מתמקד במבנים אנטומיים כגון האמיגדלה, ההיפוקמפוס ומסלולים נוירואנדוקרינים אבל... תגובות
- 16. אריק קנדל, חתן פרס נובל לרפואה/פיזיולוגיה לשנת 2000 Maale Carmel Mental Health Center, Bruce Rappaport Medical
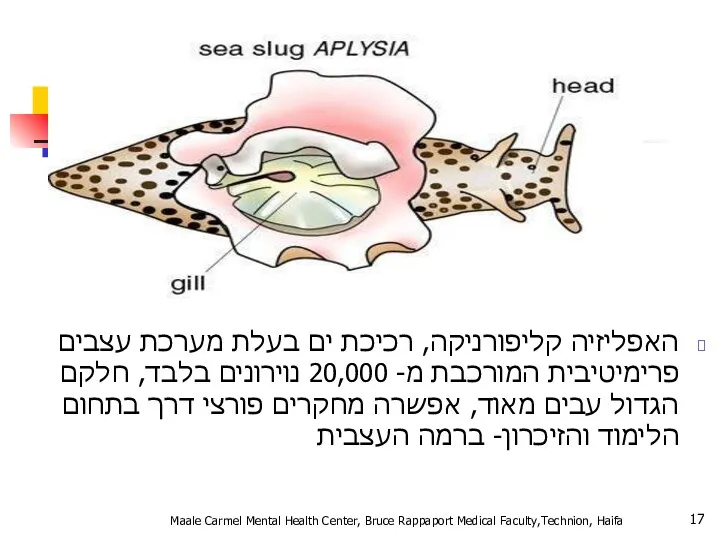
- 17. האפליזיה קליפורניקה, רכיכת ים בעלת מערכת עצבים פרימיטיבית המורכבת מ- 20,000 נוירונים בלבד, חלקם הגדול עבים
- 18. נגיעה בסיפון של האפליזיה גורמת לרתיעה נגיעה חוזרת בסיפון של האפליזיה מפחיתה את הרתיעה = הביטואציה
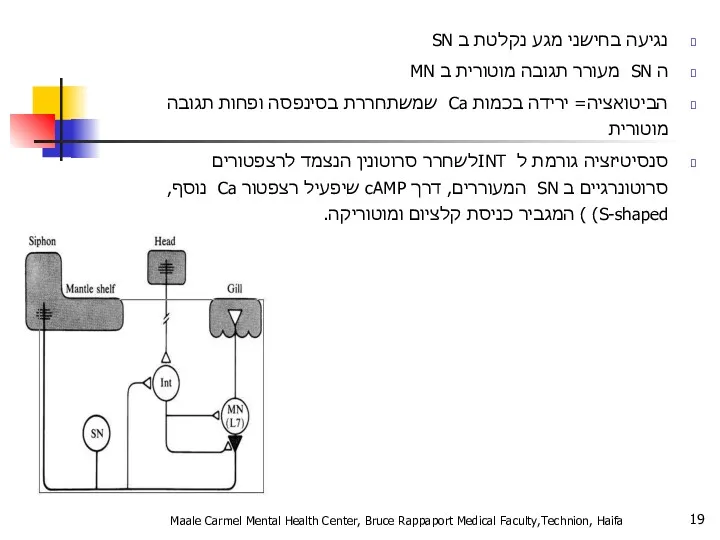
- 19. נגיעה בחישני מגע נקלטת ב SN ה SN מעורר תגובה מוטורית ב MN הביטואציה= ירידה בכמות
- 20. תגובת דחק Fight or Flight תגובה פיזיולוגית לדחק מווסתת דרך ההיפותלמוס ומבנים נוספים מאפשרת להתגונן בפני
- 21. Fight or Flight Физиологическая реакция на стресс Адаптируется с помощью гипоталамуса и других мозговоых структур Позволяет
- 22. מה קורה בתגובה הסימפתטית? מתרחשת על ידי אדרנלין ונוראדרנלין מעלה קצב לב והתכווצות הלב קצב נשימה
- 23. Что происходи при реакции симпатической системы? Происходит с помошью адреналина и норадреналина Усиливает частоту и силу
- 24. Maale Carmel Mental Health Center, Bruce Rappaport Medical Faculty,Technion, Haifa
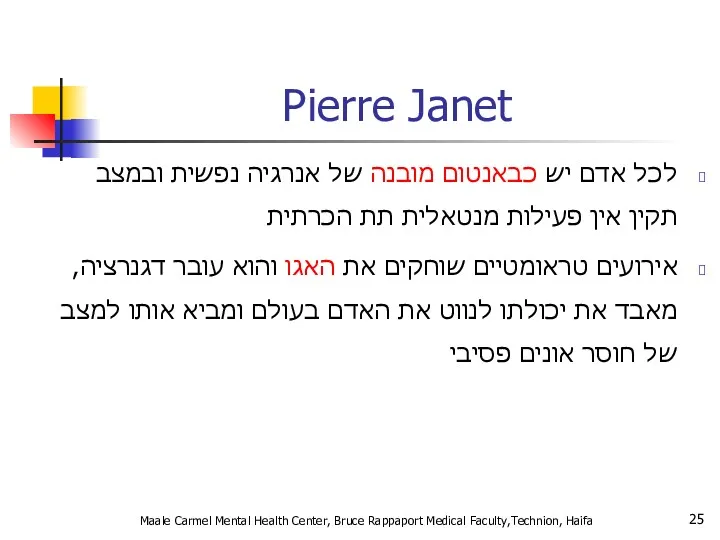
- 25. Maale Carmel Mental Health Center, Bruce Rappaport Medical Faculty,Technion, Haifa Pierre Janet לכל אדם יש כבאנטום
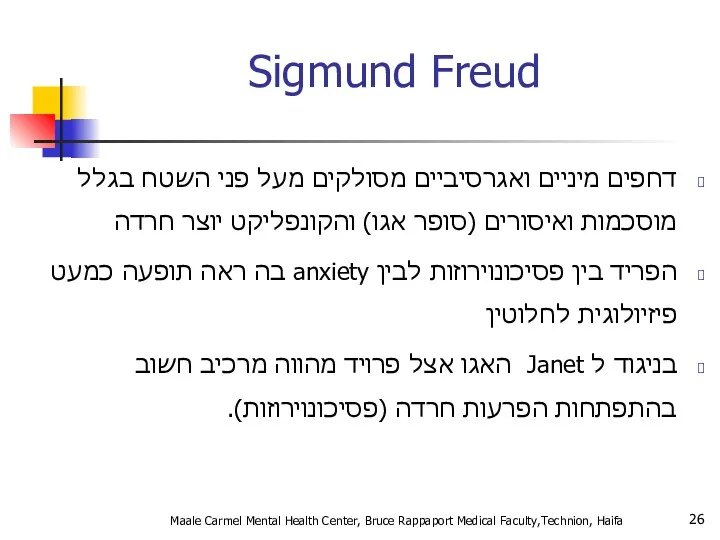
- 26. Sigmund Freud דחפים מיניים ואגרסיביים מסולקים מעל פני השטח בגלל מוסכמות ואיסורים (סופר אגו) והקונפליקט יוצר
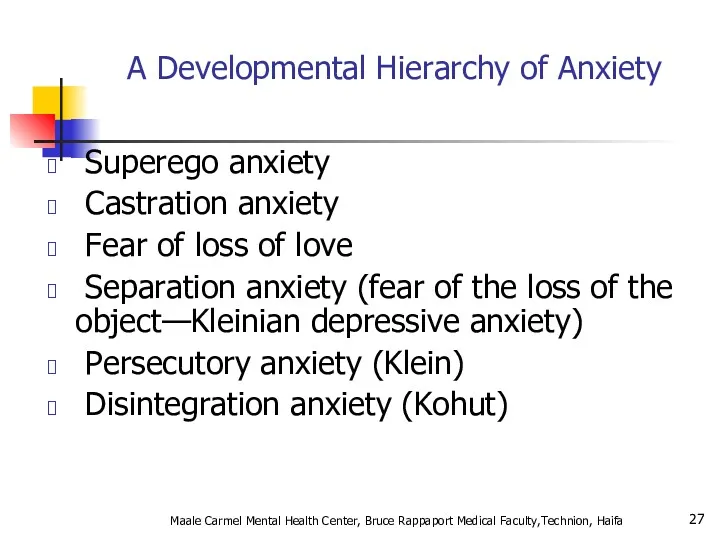
- 27. A Developmental Hierarchy of Anxiety Superego anxiety Castration anxiety Fear of loss of love Separation anxiety
- 28. Tirat Carmel Mental Health Center, Bruce Rappaport Medical Faculty,Technion, Haifa
- 29. Tirat Carmel Mental Health Center, Bruce Rappaport Medical Faculty,Technion, Haifa
- 30. Tirat Carmel Mental Health Center, Bruce Rappaport Medical Faculty,Technion, Haifa
- 31. Tirat Carmel Mental Health Center, Bruce Rappaport Medical Faculty,Technion, Haifa
- 32. Tirat Carmel Mental Health Center, Bruce Rappaport Medical Faculty,Technion, Haifa
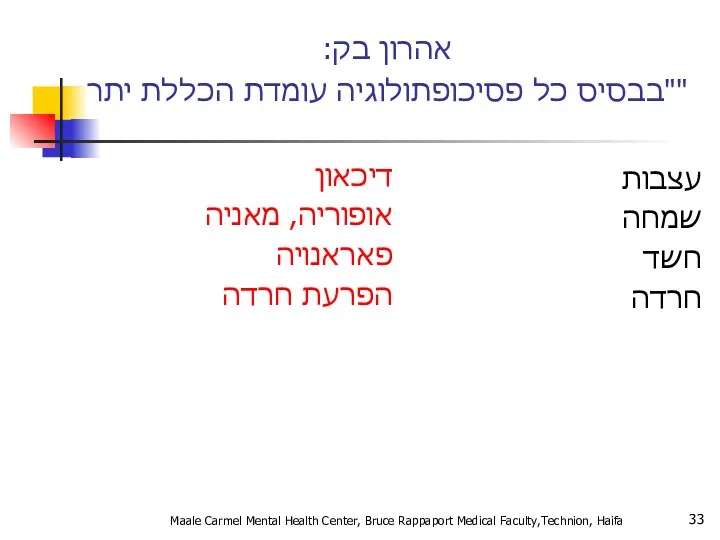
- 33. אהרון בק: "בבסיס כל פסיכופתולוגיה עומדת הכללת יתר" דיכאון אופוריה, מאניה פאראנויה הפרעת חרדה עצבות שמחה
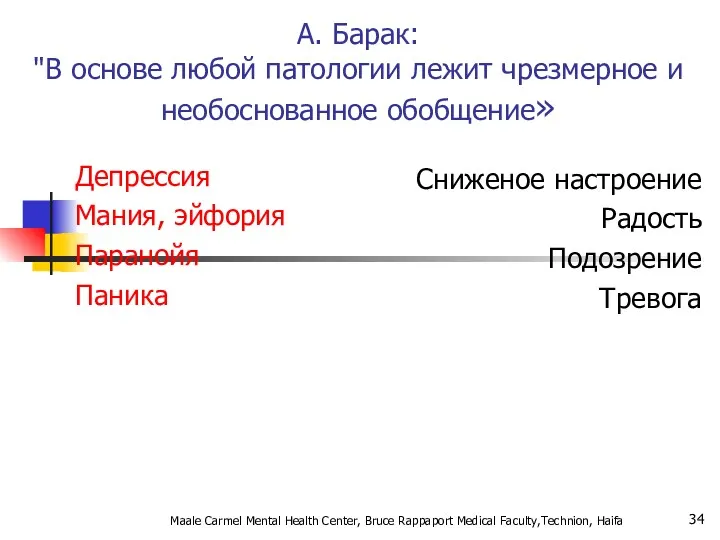
- 34. А. Барак: "В основе любой патологии лежит чрезмерное и необоснованное обобщение» Депрессия Мания, эйфория Паранойя Паника
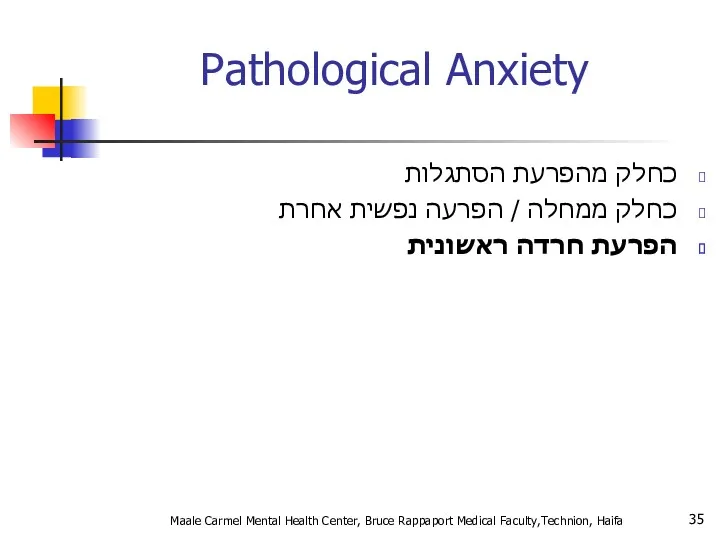
- 35. Pathological Anxiety כחלק מהפרעת הסתגלות כחלק ממחלה / הפרעה נפשית אחרת הפרעת חרדה ראשונית Maale Carmel
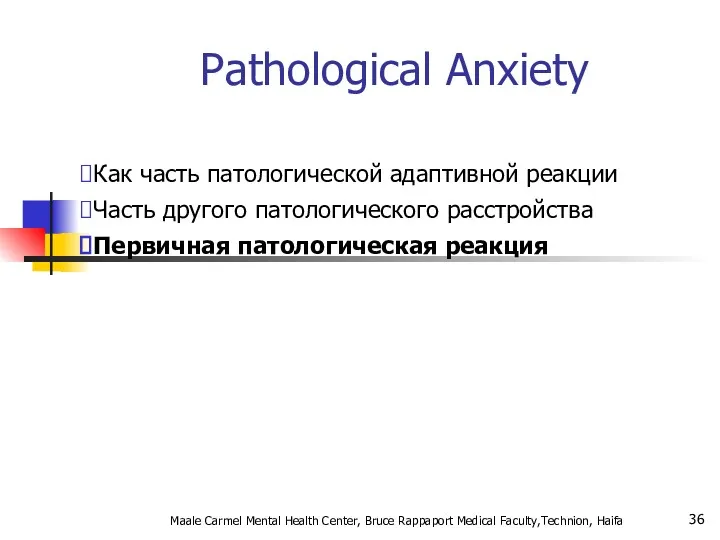
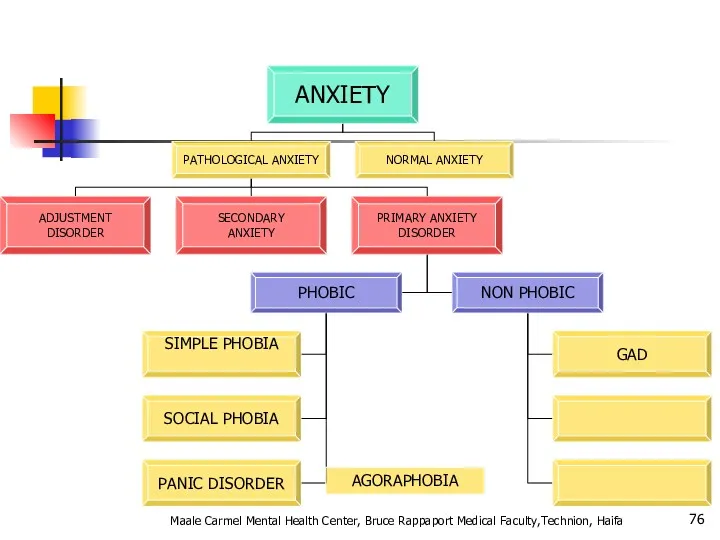
- 36. Pathological Anxiety Как часть патологической адаптивной реакции Часть другого патологического расстройства Первичная патологическая реакция Maale Carmel
- 37. Primary Anxiety Disorders הפרעות חרדה לא פוביות: GENERAILIZED ANXIETY DISORDER OCD הפרעות חרדה פוביות: SIMPLE PHOBIA
- 38. Primary Anxiety Disorders Нефобические тревожные реакции: GENERAILIZED ANXIETY DISORDER Фобические тревожные реакии: SIMPLE PHOBIA SOCIAL PHOBIA
- 39. אפידמיולוגיה ברוב המקרים נשים סובלות יותר, במיוחד בגילים בין 16 ל – 40. פחד קהל פי
- 40. Эпидемиология В большинстве своем женщины страдают чаще мужчин, в основном в возрасте 16-40 лет Социофобия в
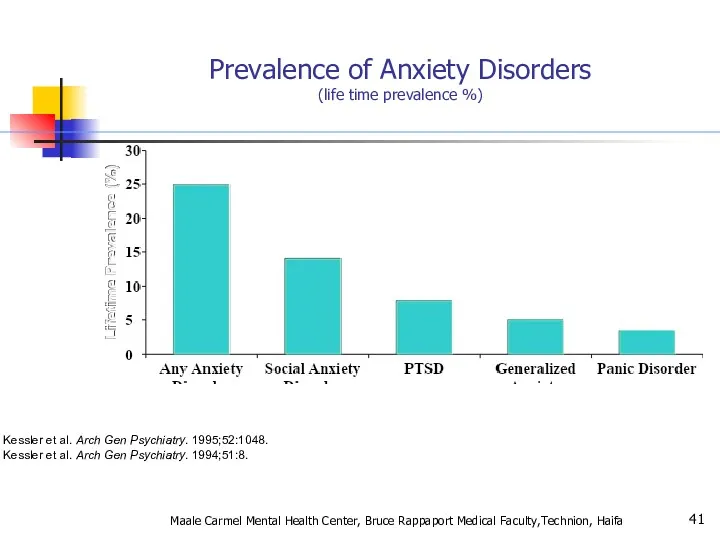
- 41. Kessler et al. Arch Gen Psychiatry. 1995;52:1048. Kessler et al. Arch Gen Psychiatry. 1994;51:8. Prevalence of
- 42. Genetic Epidemiology of Anxiety Disorders There is significant familial aggregation for PD, GAD, OCD and phobias
- 43. Anxiety Disorders “The anxiety must be out of proportion to the actual danger or threat in
- 44. Agoraphobia , Specific Phobia, and Social Anxiety Disorder Changes in criteria : Clients over 18 do
- 45. Panic Attacks and Agoraphobia are “unlinked” in DSM- 5 DSM- IV terminology describing different types of
- 46. Specific Phobia Maale Carmel Mental Health Center, Bruce Rappaport Medical Faculty,Technion, Haifa
- 47. Animal Type Natural Environment Type (e.g., heights, storms, water) Blood-Injection-Injury Type Situational Type (e.g., airplanes, elevators,
- 48. Specific Phobia Marked or persistent fear (>6 months) that is excessive or unreasonable cued by the
- 49. SPECIFIC PHOBIA בשאר הזמן תפקוד נורמאלי המנעות מאפשרת חיים נורמאליים שכיחות גבוהה –עד 20% מהאוכלוסייה בד"כ
- 50. SOCIAL PHOBIA בדומה לפוביה פשוטה אך כאן הפחד חסר הגיון מאינטראקציה חברתית, ומכאן: יותר פגיעה תפקודית
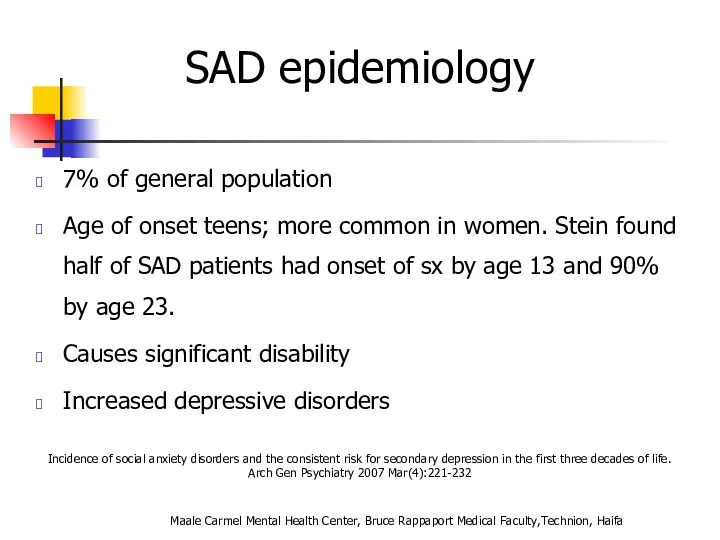
- 51. Incidence of social anxiety disorders and the consistent risk for secondary depression in the first three
- 52. אבחנה יותר בעייתית (הפרעת אישיות?? ) שני סוגים: LIMITED PERVASIVE Maale Carmel Mental Health Center, Bruce
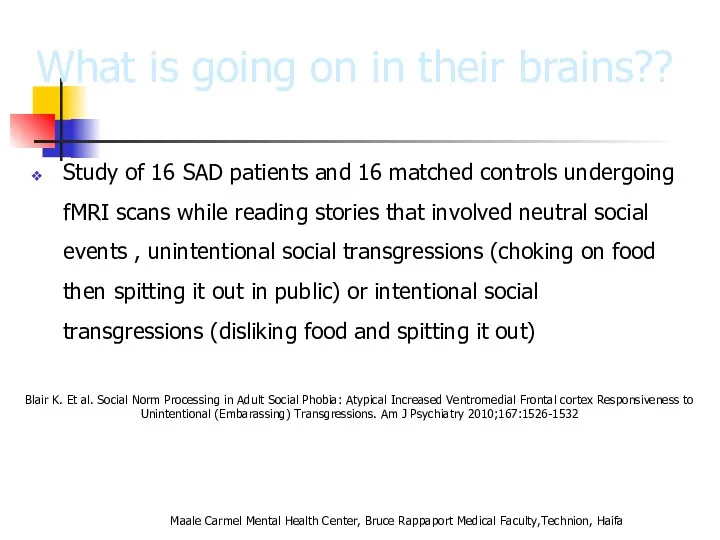
- 53. What is going on in their brains?? Study of 16 SAD patients and 16 matched controls
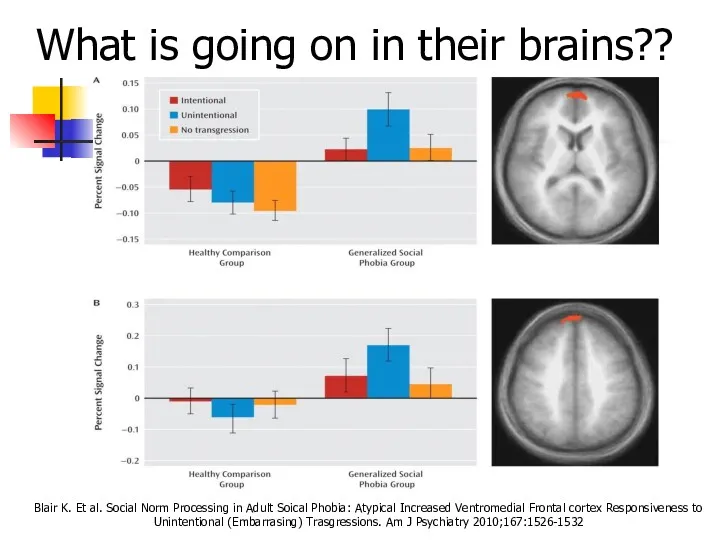
- 54. What is going on in their brains?? Both groups ↑ medial prefrontal cortex activity in response
- 55. What is going on in their brains?? Blair K. Et al. Social Norm Processing in Adult
- 56. Functional imaging studies in SAD Several studies have found hyperactivity of the amygdala even with a
- 57. Social Anxiety Disorder treatment Social skills training, behavior therapy, cognitive therapy Medication – SSRIs, SNRIs, MAOIs,
- 58. סיבוכים: דיכאון שימוש בחומרים ממכרים Maale Carmel Mental Health Center, Bruce Rappaport Medical Faculty,Technion, Haifa
- 59. PANIC DISORDER התקף אימה, חרדה בעוצמה קיצונית מופיע ספונטאנית (לפחות בתחילת המחלה) הכללת אירועים חרדה מטרימהANTICIPATION
- 60. Panic Disorder Recurrent unexpected panic attacks and for a one month period or more of: Persistent
- 61. A Panic Attack is: Palpitations or rapid heart rate Sweating Trembling or shaking Shortness of breath
- 62. Panic disorder epidemiology 2-3% of general population; 5-10% of primary care patients.Onset in teens or early
- 63. Things to keep in mind A panic attack ≠ panic disorder Panic disorder often has a
- 64. With Agoraphobia פחד או המנעות להיות במקומות או במצבים בהם יש קושי לברוח או לקבל עזרה.
- 65. טיפול: שילוב של טיפול CBT ותרופות: נוגדי דיכאון נוגדי חרדה לשלב הראשון סיבוכים : דיכאון עד
- 66. Panic Disorder Comorbidity 50-60% have lifetime major depression One third have current depression 20-25% have history
- 67. Panic Disorder Etiology Drug/Alcohol Genetics Social learning Cognitive theories Neurobiology/conditioned fear Psychosocial stressors Prior separation anxiety
- 68. Treatment See 70% or better treatment response Education, reassurance, elimination of caffeine, alcohol, drugs, OTC stimulants
- 69. Agoraphobia Marked fear or anxiety for more than 6 months about two or more of the
- 70. Agoraphobia The individual fears or avoids these situations because escape might be difficult or help might
- 71. Prevalence 2% of the population Females to males:2:1 Mean onset is 17 years 30% of persons
- 72. Generalized Anxiety פחד או חרדה מוגזמים, ללא כל אחיזה במציאות, מלווים בביטוים של מתח מוטורי, פעילות
- 73. Generalized Anxiety Disorder Excessive worry more days than not for at least 6 months about a
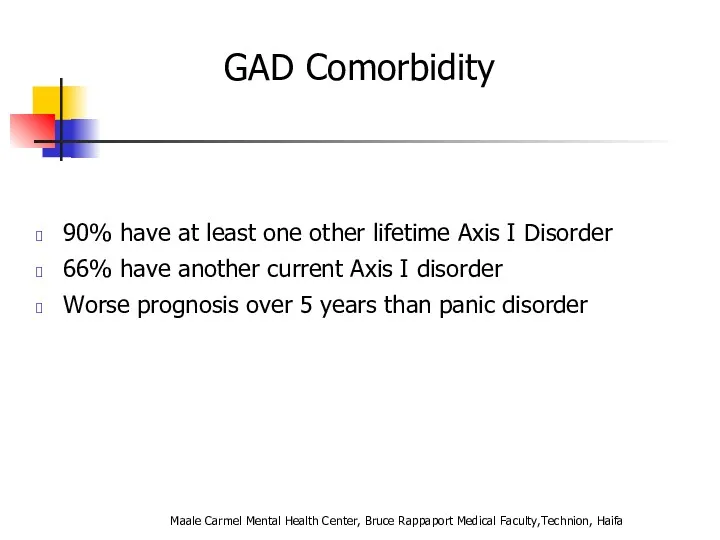
- 74. GAD Comorbidity 90% have at least one other lifetime Axis I Disorder 66% have another current
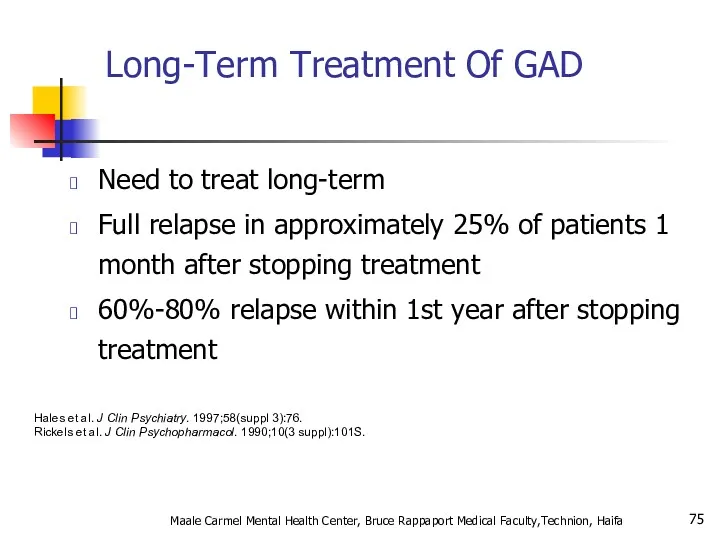
- 75. Long-Term Treatment Of GAD Need to treat long-term Full relapse in approximately 25% of patients 1
- 76. Maale Carmel Mental Health Center, Bruce Rappaport Medical Faculty,Technion, Haifa AGORAPHOBIA
- 77. Tirat Carmel Mental Health Center, Bruce Rappaport Medical Faculty,Technion, Haifa
- 78. Pharmacotherapy for Anxiety Disorders Antidepressants Serotonin Selective Reuptake Inhibitors (SSRIs) Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) Atypical Antidepressants
- 79. Benzodiazepines Other Agents Azaspirones Beta blockers Anticonvulsants Other strategies Maale Carmel Mental Health Center, Bruce Rappaport
- 80. Discontinuation of Treatment for Anxiety Disorders Withdrawal/rebound more common with Bzd than other anxiolytic treatment Relapse:
- 81. Strategies for Anxiolytic Discontinuation Slow taper Switch to longer-acting agent for taper Cognitive-Behavioral therapy Adjunctive Antidepressant
- 82. Strategies for Refractory Anxiety Disorder Maximize dose Combine antidepressant and benzodiazepine Administer cognitive-behavioral therapy Attend to
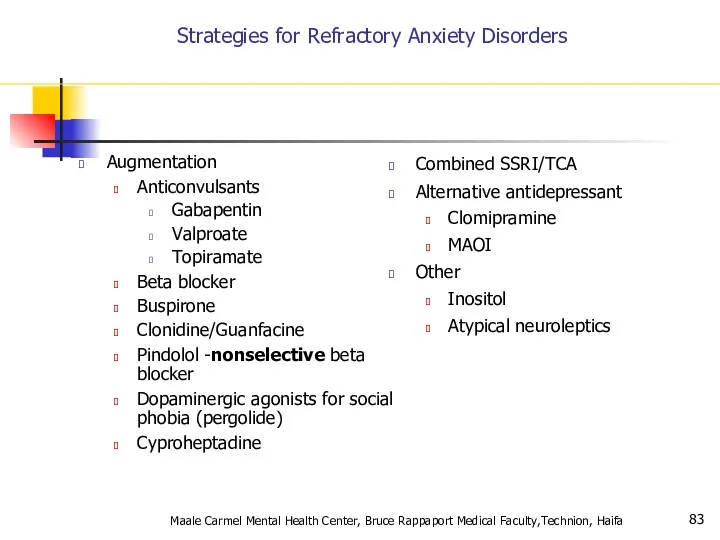
- 83. Strategies for Refractory Anxiety Disorders Augmentation Anticonvulsants Gabapentin Valproate Topiramate Beta blocker Buspirone Clonidine/Guanfacine Pindolol -nonselective
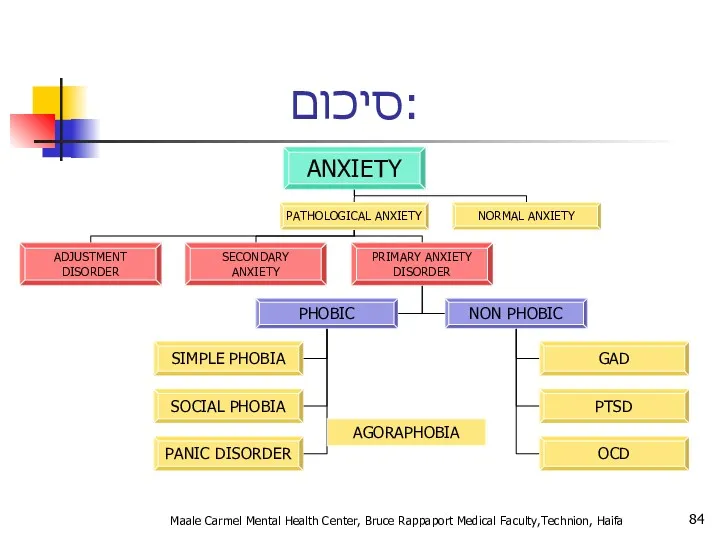
- 84. סיכום: Maale Carmel Mental Health Center, Bruce Rappaport Medical Faculty,Technion, Haifa AGORAPHOBIA
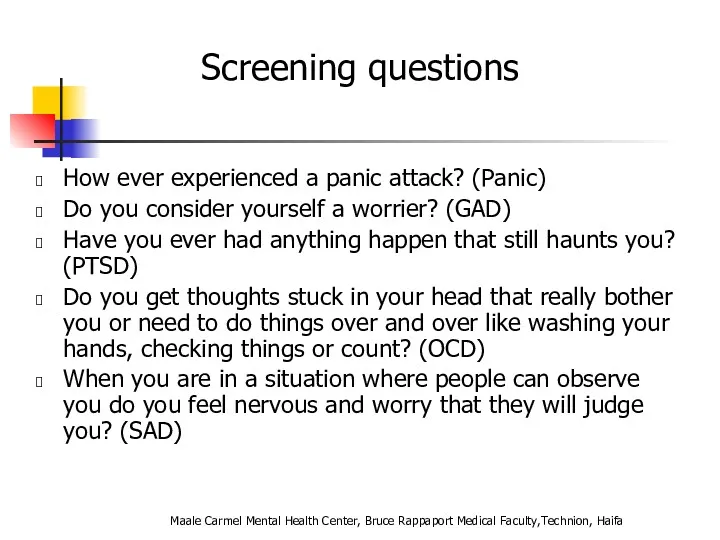
- 85. Screening questions How ever experienced a panic attack? (Panic) Do you consider yourself a worrier? (GAD)
- 86. Take home points Anxiety, Obsessive-Compulsive and Related, and Trauma and Stressor-related disorders are common, common, common!
- 87. Tirat Carmel Mental Health Center, Bruce Rappaport Medical Faculty,Technion, Haifa Question
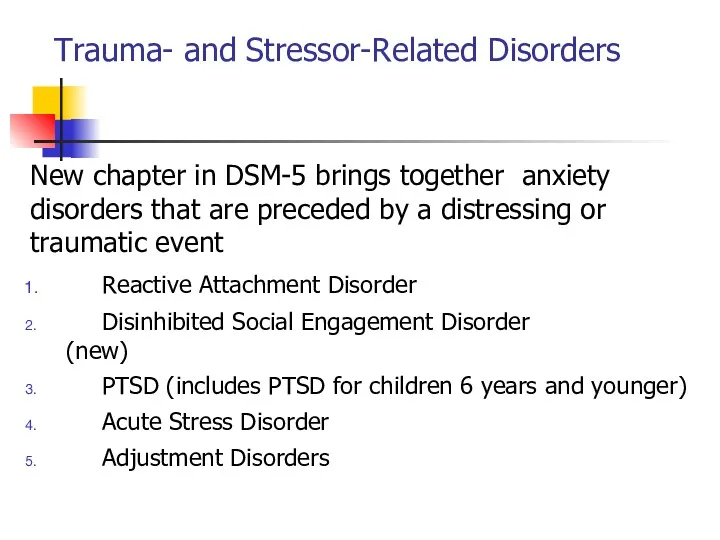
- 89. Trauma- and Stressor-Related Disorders New chapter in DSM-5 brings together anxiety disorders that are preceded by
- 90. Disinhibited Social Engagement Disorder “The essential feature of disorder is a pattern of behavior that involves
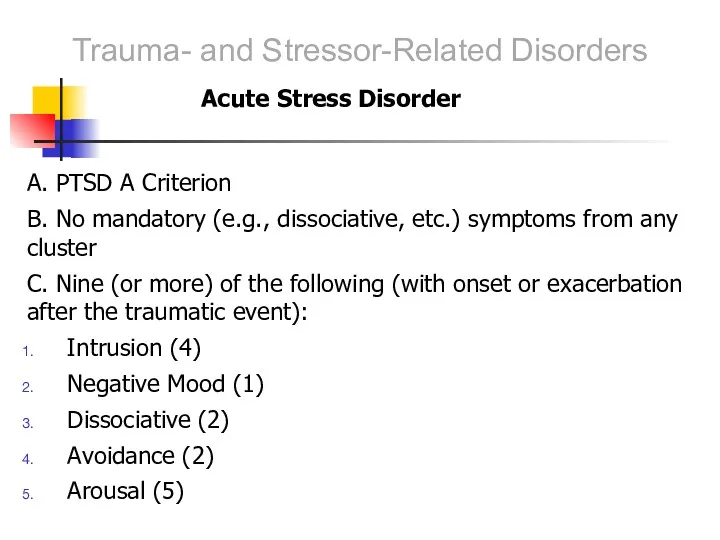
- 91. A. PTSD A Criterion B. No mandatory (e.g., dissociative, etc.) symptoms from any cluster C. Nine
- 92. Adjustment Disorders are redefined as an array of stress-response syndromes occurring after exposure to a distressing
- 93. Chronic Adjustment Disorder Omitted by mistake from DSM-5 Acute AD – less than 6 months Chronic
- 94. Other Specified Trauma/Stressor-Related Disorder (309.89) AD with duration more than 6 months without prolonged duration of
- 95. Reactive Attachment Disorder Emotionally withdrawn behavior Social/emotional disturbance - reduced responsiveness, limited affect &/or irritability, sadness
- 96. Persistent Complex Bereavement Disorder Onset > 12 months after death of loved one Yearning/Sorrow/Pre-occupation with deceased
- 97. Persistent Complex Bereavement Disorder (PCBD) Diagnostic Criteria-ICD The person experienced the death of a close relative
- 98. Persistent Complex Bereavement Disorder (PCBD) Preoccupation with the circumstances of the death. In children, this preoccupation
- 99. Reactive Distress to the Death Marked difficulty accepting the death. In children, this is dependent on
- 100. Social/Identity Disruption A desire to die in order to be with the deceased. Difficulty trusting other
- 101. Specify if: With Traumatic Bereavement: Following a death that occurred under traumatic circumstances (e.g. homicide, suicide,
- 102. Tirat Carmel Mental Health Center, Bruce Rappaport Medical Faculty,Technion, Haifa
- 103. Changes in PTSD Criteria Four symptom clusters, rather than three -Re-experiencing -Avoidance -Persistent negative alterations in
- 104. Changes in PTSD Criteria DSM-5 more clearly defines what constitutes a traumatic event Sexual assault is
- 105. Changes in PTSD Criteria Recognition of PTSD in Young children Developmentally sensitive: Criteria have been modified
- 106. DSM-5: PTSD Criterion A A. The person was exposed to: death, threatened death, actual or threatened
- 107. Criterion A (continued): 3. Indirectly, by learning that a close relative or close friend was exposed
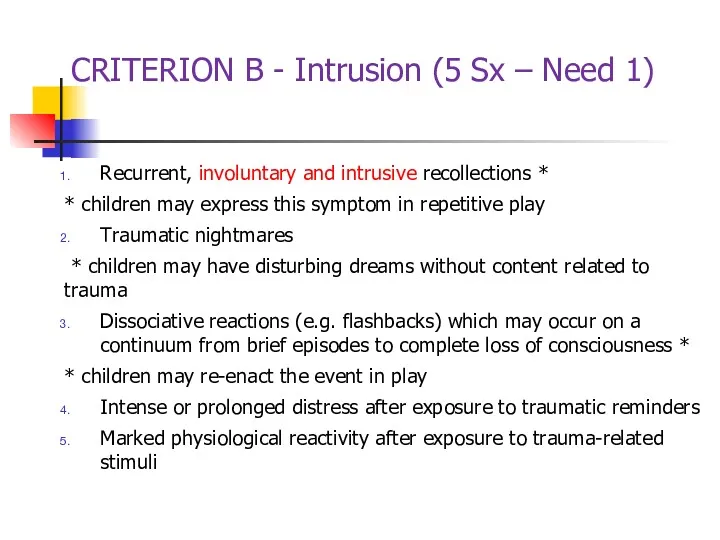
- 108. CRITERION B - Intrusion (5 Sx – Need 1) Recurrent, involuntary and intrusive recollections * *
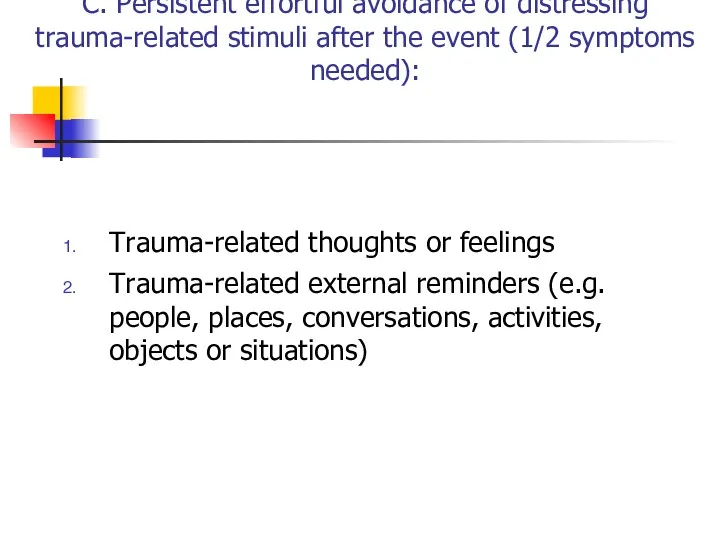
- 109. C. Persistent effortful avoidance of distressing trauma-related stimuli after the event (1/2 symptoms needed): Trauma-related thoughts
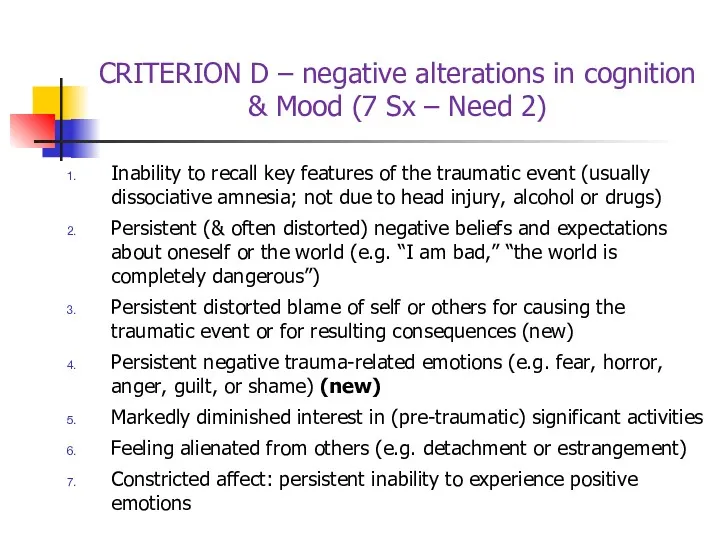
- 110. CRITERION D – negative alterations in cognition & Mood (7 Sx – Need 2) Inability to
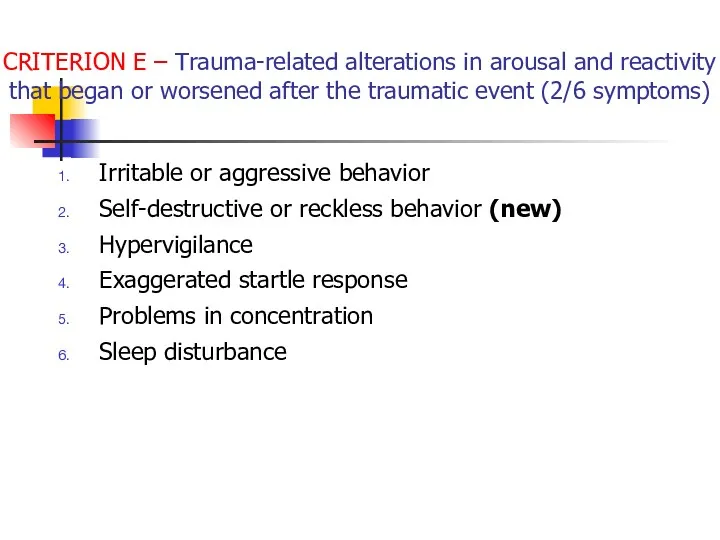
- 111. CRITERION E – Trauma-related alterations in arousal and reactivity that began or worsened after the traumatic
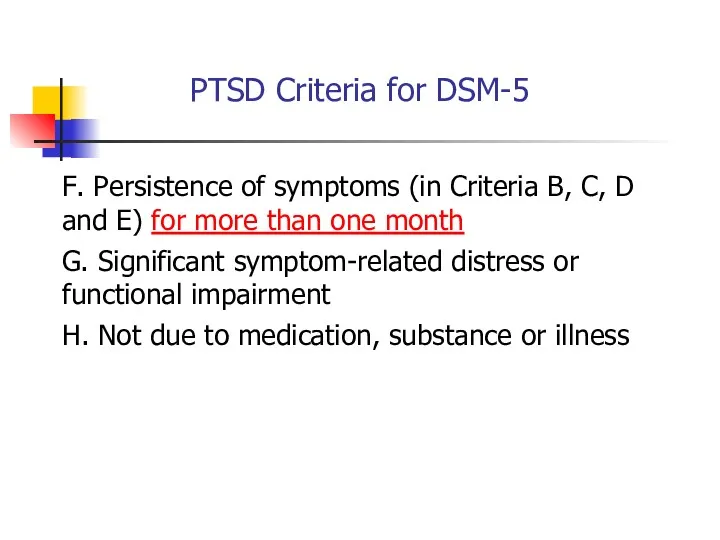
- 112. PTSD Criteria for DSM-5 F. Persistence of symptoms (in Criteria B, C, D and E) for
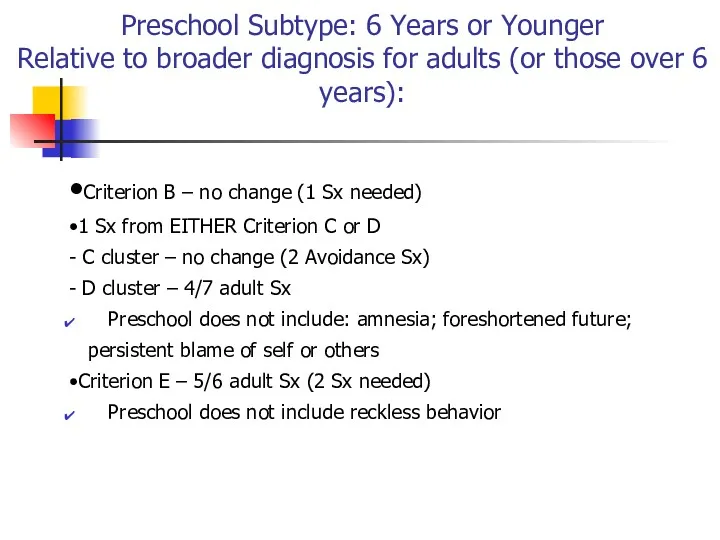
- 113. Preschool Subtype: 6 Years or Younger Relative to broader diagnosis for adults (or those over 6
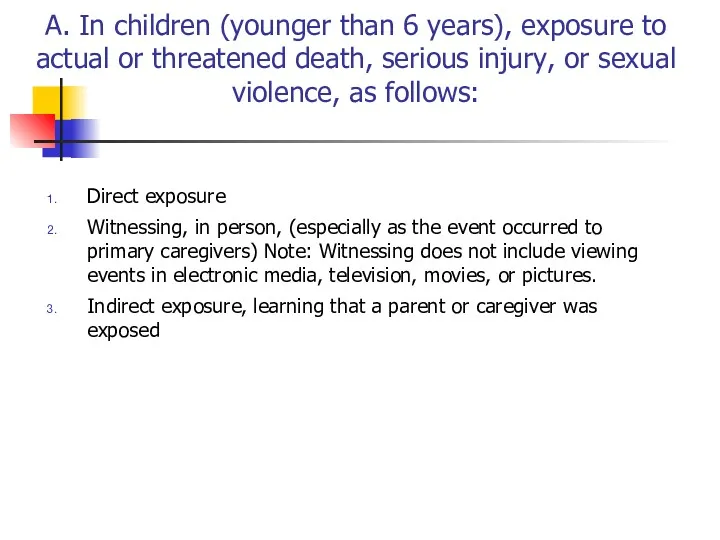
- 114. A. In children (younger than 6 years), exposure to actual or threatened death, serious injury, or
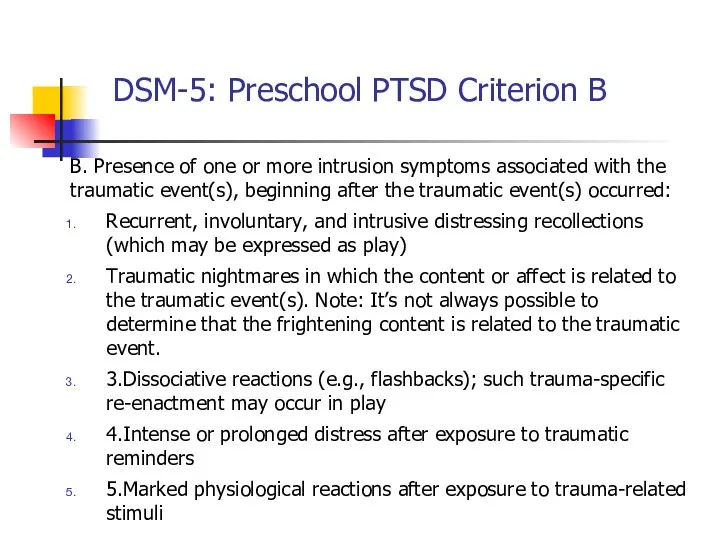
- 115. DSM-5: Preschool PTSD Criterion B B. Presence of one or more intrusion symptoms associated with the
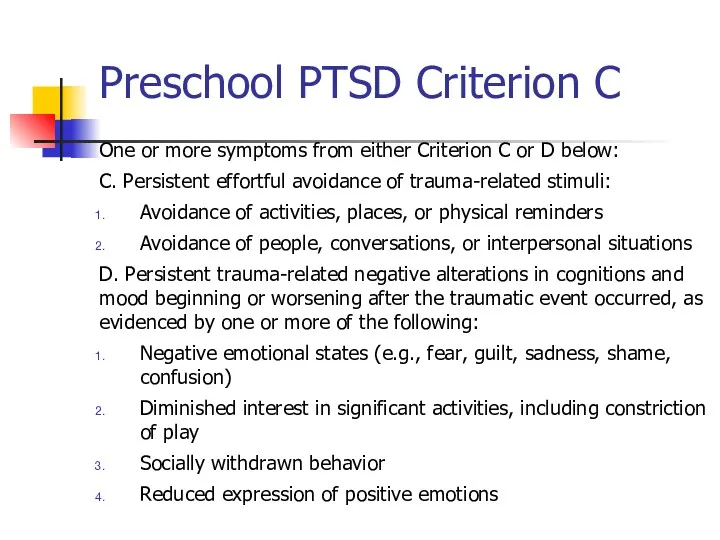
- 116. Preschool PTSD Criterion C One or more symptoms from either Criterion C or D below: C.
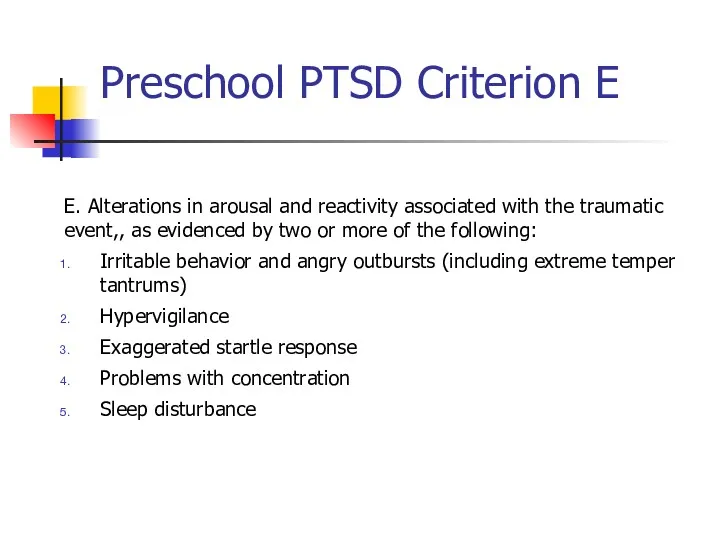
- 117. Preschool PTSD Criterion E E. Alterations in arousal and reactivity associated with the traumatic event,, as
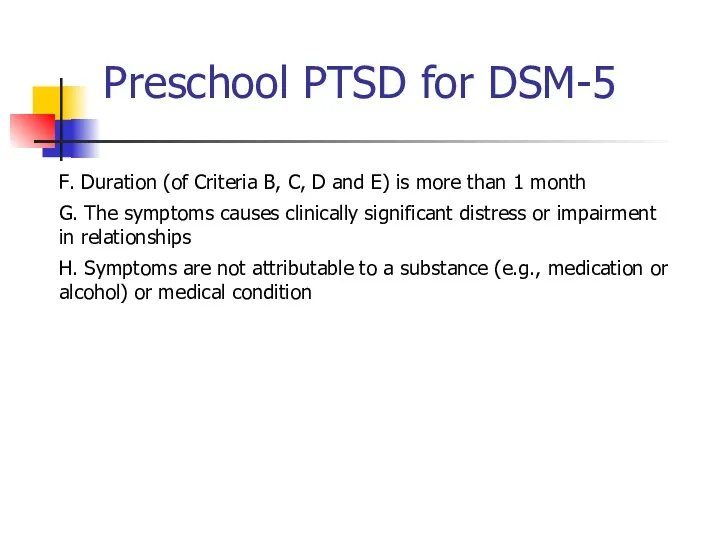
- 118. Preschool PTSD for DSM-5 F. Duration (of Criteria B, C, D and E) is more than
- 119. Summary: PTSD in DSM-5 Perhaps PTSD should be re-conceptualized as a spectrum disorder in which several
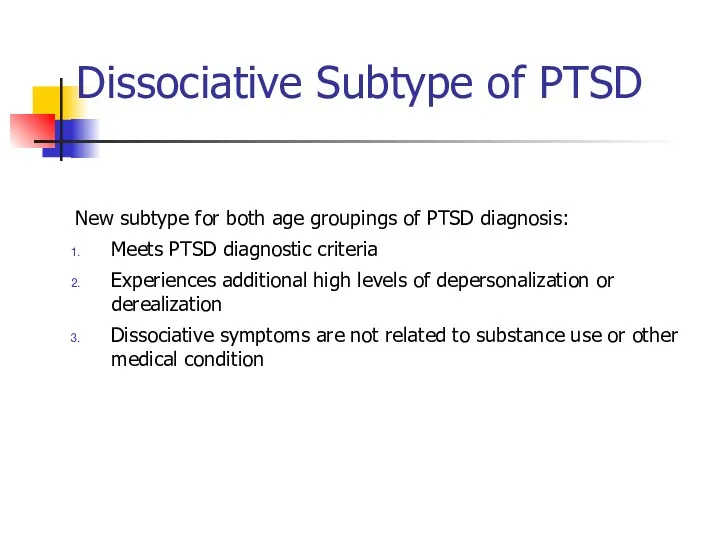
- 120. Dissociative Subtype of PTSD New subtype for both age groupings of PTSD diagnosis: Meets PTSD diagnostic
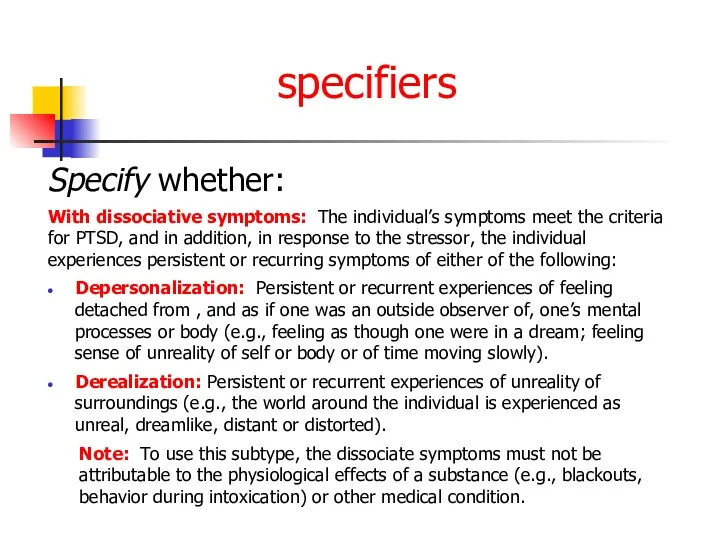
- 121. specifiers Specify whether: With dissociative symptoms: The individual’s symptoms meet the criteria for PTSD, and in
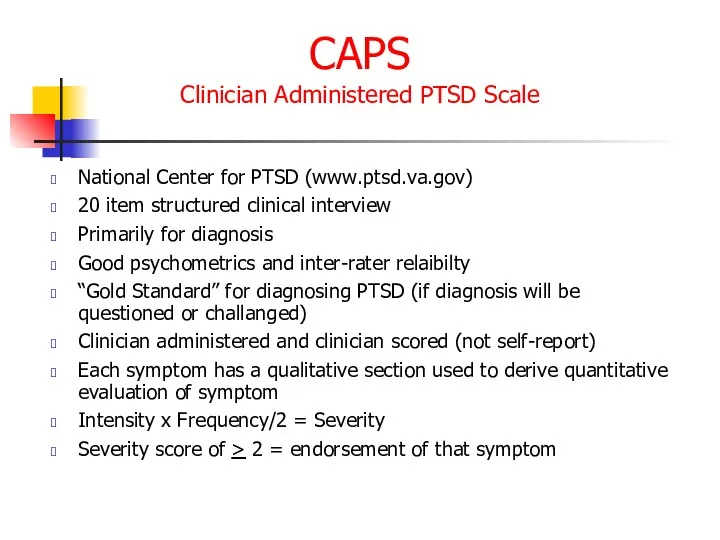
- 122. CAPS Clinician Administered PTSD Scale National Center for PTSD (www.ptsd.va.gov) 20 item structured clinical interview Primarily
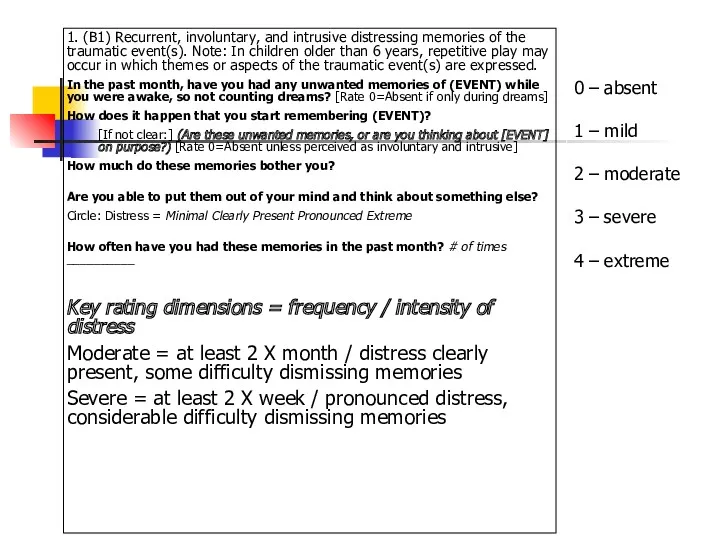
- 123. 1. (B1) Recurrent, involuntary, and intrusive distressing memories of the traumatic event(s). Note: In children older
- 124. PCL Posttraumatic Check List National Center for PTSD (www.ptsd.va.gov) Simple, easy to administer Self-report or clinician
- 125. TRS Trauma Recovery Scale Gentry, 1996 Developed as an outcome instrument Good psychometrics (Chronbach’s a =
- 126. Early Sessions Graphic Time Line of life including ALL significant traumatic experiences Verbal Narrative using GTL
- 127. PTSD Epidemiology 7-9% of general population 60-80% of trauma victims 30% of combat veterans 50-80% of
- 128. PTSD Epidemiology בין אבחנות בודדות ב DSM שמדברת על אטיולוגיה זוהי תגובה נפשית קשה הנגרמת כתגובה
- 129. Comorbidities Depression Other anxiety disorders Substance use disorders Somatization Dissociative disorders Maale Carmel Mental Health Center,
- 130. Acute PTSD - symptoms less than three months Chronic PTSD - symptoms more than three months
- 131. Can occur at any age, including childhood, and can affect anyone. Individuals who have recently immigrated
- 132. Onset Symptoms usually begin within the first 3 months after the trauma, although there may be
- 133. Tirat Carmel Mental Health Center, Bruce Rappaport Medical Faculty,Technion, Haifa
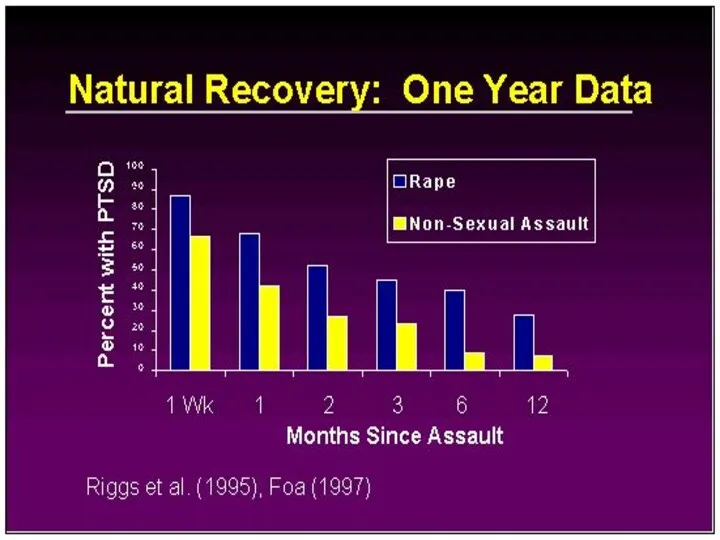
- 134. Course The symptoms and the relative predominance of re-experiencing, avoidance, and increased arousal symptoms may vary
- 135. Course Continued The severity, duration, and proximity of an individual’s exposure to a traumatic event are
- 136. Rape (49%) Severe beating or physical assault (31.9%) Other sexual assault (23.7%) Serious accident or injury
- 137. Differential Diagnosis Differential diagnosis of the disorder or problem; that is, what other disorders or problems
- 138. While the symptoms of posttraumatic stress disorder (PTSD) may seem similar to those of other disorders,
- 139. Differences between Acute Stress Disorder In general, the symptoms of acute stress disorder must occur within
- 140. Differences between PTSD and Obsessive-Compulsive Disorder Both have recurrent, intrusive thoughts as a symptom, but the
- 141. Differences Between PTSD and Adjustment Disorder PTSD symptoms can also seem similar to adjustment disorder because
- 142. Differences Between PTSD and Depression Depression after trauma and PTSD both may present numbing and avoidance
- 143. מי מיועד יותר? עוצמה של סטרסור פתאומיות (לא צפוי) חוסר יכולת לשלוט על מתרחש sexual as
- 144. An adult's risk for psychological distress will increase as the number of the following factors increases:
- 145. For women, the presence of a spouse, especially if he is significantly distressed Psychiatric history Severe
- 146. Why PTSD Victims Might Be Resistant to Getting Help Sometimes hard because people expect to be
- 147. During a Traumatic Event Norepinephrine- Mobilizing fear, the flight response, sympathetic activation, consolidating memory Too much
- 148. Causal Attributions “PTSD is typified by both automatic, involuntary symptoms, (e.g. flashbacks, intrusive thoughts, autonomic hyperarousal)
- 149. Treatment Individual Therapy Group Support (especially for Chronic PTSD) Medication
- 150. Treatment Continued For PTSD in children, adolescents, and geriatrics the preferred treatment is psychotherapy Acute PTSD
- 151. Treatment Continued Exposure Therapy- Education about common reactions to trauma, breathing retraining, and repeated exposure to
- 152. Treatment Continued “Cognitive Restructuring involved teaching and reinforcing self-monitoring or thoughts and emotions, identifying automatic thoughts
- 153. Medications approved for the treatment of Anxiety Disorders including PTSD SSRIs – Sertraline (Zoloft), Paroxetine (Paxil),
- 154. Tricyclic Antidepressants- Clomiprimine (Anafranil), Doxepin (Sinequan) Nortriptyline (Aventyl), Amitriptyline (Elavil), Maprotiline (Ludiomil) Desipramine (Norpramin) Affects concentration
- 155. Treatment With treatment, symptoms should improve after 3 months In Chronic PTSD cases, 1-2 years
- 156. Noradrenergic Agents Beta Blockers – Propranolol Future Direction of Treatment
- 157. PTSD - Treatment שילוב של טיפול תרופתי בנוגדי דיכאון וחרדה בפועל מגיעים לכל הספקטרום של התרופות
- 158. Future Direction of Treatment Continued “Early Diagnosis and intervention- either psychotherapeutic or pharmacological- following trauma may
- 159. PTSD Myths PTSD is a complex disorder that often is misunderstood. Not everyone who experiences a
- 160. PTSD Myths Continued MYTH: People should be able to move on with their lives after a
- 161. PTSD Myths Continued MYTH: People suffer from PTSD right after they experience a traumatic event. FACT:
- 162. What is Prolonged Exposure? PE is a type of CBT, which is designed to specifically target
- 163. education about common reactions to trauma breathing retraining (or relaxation training) prolonged (repeated) exposure to trauma
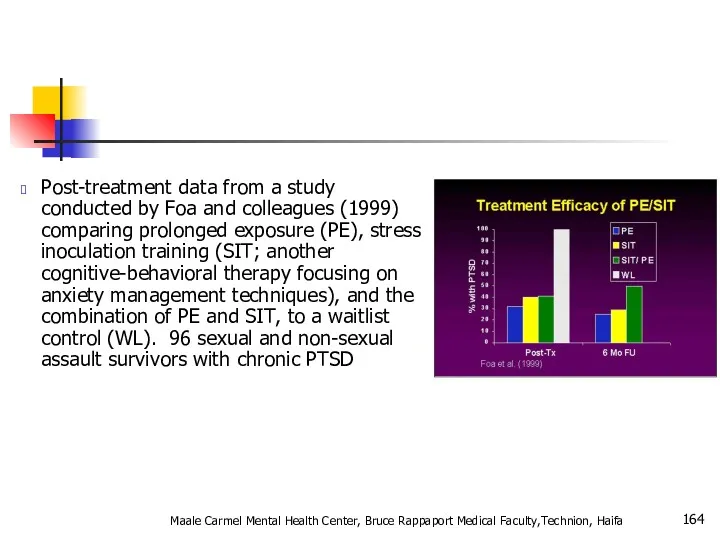
- 164. Post-treatment data from a study conducted by Foa and colleagues (1999) comparing prolonged exposure (PE), stress
- 165. Combat Reaction Combat stress reaction, better known as "Shell Shock" is the post traumatic reaction of
- 166. The Background of Combat Reaction The transition from civilian life to military life is acute. The
- 167. In wartime, a new and even more acute transition is added - the transition from conditions
- 168. On the other hand the soldier feels solidarity with his unit, pride and honor and a
- 169. Risk Factors Risk factors for Combat Reaction are all the factors that influence the incidence of
- 170. Enforced passivity. When the soldier is deprived of activity and is in a state of waiting
- 171. PIE principles Proximity - treat the casualties close to the front and within sound of the
- 172. The US services now use the more recently developed BICEPS principles: Brevity Immediacy Centrality or Contact
- 173. Treatment results Data from the 1982 Lebanon war showed that with proximal treatment 90% of CSR
- 174. Controversy Throughout wars but notably during the Vietnam War there has been a conflict amongst doctors
- 175. תסמונת שואה דור ראשון דור שני Maale Carmel Mental Health Center, Bruce Rappaport Medical Faculty,Technion, Haifa
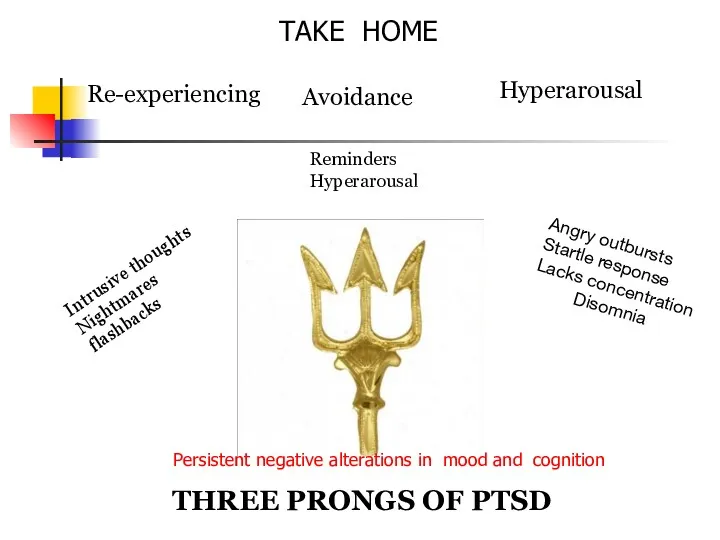
- 176. Re-experiencing Intrusive thoughts Nightmares flashbacks Avoidance Hyperarousal Reminders Hyperarousal Angry outbursts Startle response Lacks concentration Disomnia
- 178. Скачать презентацию




















 Невербальные средства общения
Невербальные средства общения Манипуляции
Манипуляции Деловые и межкультурные коммуникации. Типы конфликтных личностей
Деловые и межкультурные коммуникации. Типы конфликтных личностей Вербальные и невербальные средства коммуникации
Вербальные и невербальные средства коммуникации Методы диагностики конфликтных ситуаций в ОО
Методы диагностики конфликтных ситуаций в ОО Профессиональный отбор
Профессиональный отбор Представление о внимании в современной когнитивной психологии
Представление о внимании в современной когнитивной психологии Профессиональное самоопределение личности
Профессиональное самоопределение личности Общая характеристика одаренности в психологии
Общая характеристика одаренности в психологии Невербальное общение. Язык жестов
Невербальное общение. Язык жестов Психологиялық тесттер
Психологиялық тесттер Комп'ютерна залежність - ознаки, стадії, причини виникнення та профілактика. Селфіманія - хвороба чи спосіб самовираження
Комп'ютерна залежність - ознаки, стадії, причини виникнення та профілактика. Селфіманія - хвороба чи спосіб самовираження Особенности развития психологической готовности подростка к разрешению конфликтов
Особенности развития психологической готовности подростка к разрешению конфликтов Особенности общения с пациентами с нарушениями слуха, зрения, речи, с асоциальным рискованным поведением
Особенности общения с пациентами с нарушениями слуха, зрения, речи, с асоциальным рискованным поведением Когнитивные стили и социально-психологические характеристики руководителей (часть 2)
Когнитивные стили и социально-психологические характеристики руководителей (часть 2) Психология ребёнка и взаимоотношений
Психология ребёнка и взаимоотношений Тұлға . Басқару жүйесіндегі жеке тұлға
Тұлға . Басқару жүйесіндегі жеке тұлға Професиограмма, психограмма
Професиограмма, психограмма Синектика. Метод поиска творческих решений
Синектика. Метод поиска творческих решений Характер и темперамент личности
Характер и темперамент личности Психология конфликта
Психология конфликта Структура психологической службы в учреждениях и органах исполняющих уголовные наказания и нормативно-правовые документы
Структура психологической службы в учреждениях и органах исполняющих уголовные наказания и нормативно-правовые документы Психокоррекционная работа детского практического психолога
Психокоррекционная работа детского практического психолога Управление человеческими ресурсами: инструкция по применению для специалистов муниципальных органов управления образованием
Управление человеческими ресурсами: инструкция по применению для специалистов муниципальных органов управления образованием Психологические особенности обучения взрослых
Психологические особенности обучения взрослых Общение и речь. Коммуникативные барьеры
Общение и речь. Коммуникативные барьеры Ораторская речь и её особенности
Ораторская речь и её особенности Готовность ребёнка к школьному обучению
Готовность ребёнка к школьному обучению