Содержание
- 3. Antihypertensive Drugs: I. Diuretics: Hydrochlorthiazide (Dichlothiazide) – Tab. 0.025 and 0.1 g Furosemide (Lasix) – Tab.
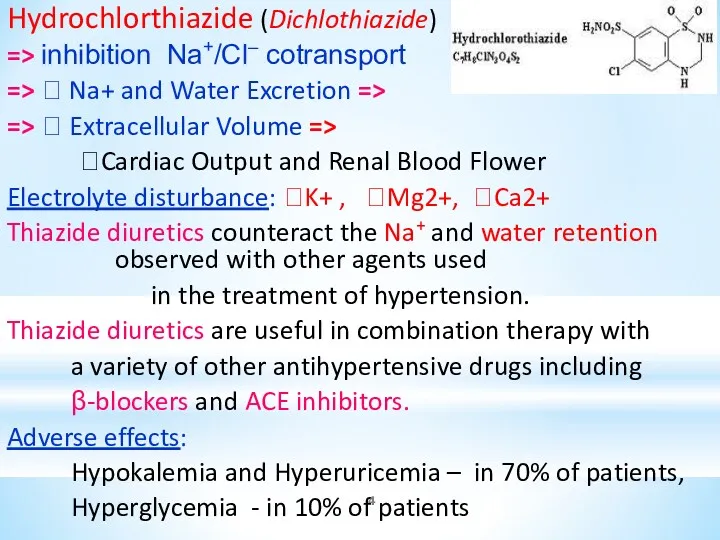
- 4. Hydrochlorthiazide (Dichlothiazide) => inhibition Na+/Cl– cotransport => ? Na+ and Water Excretion => => ? Extracellular
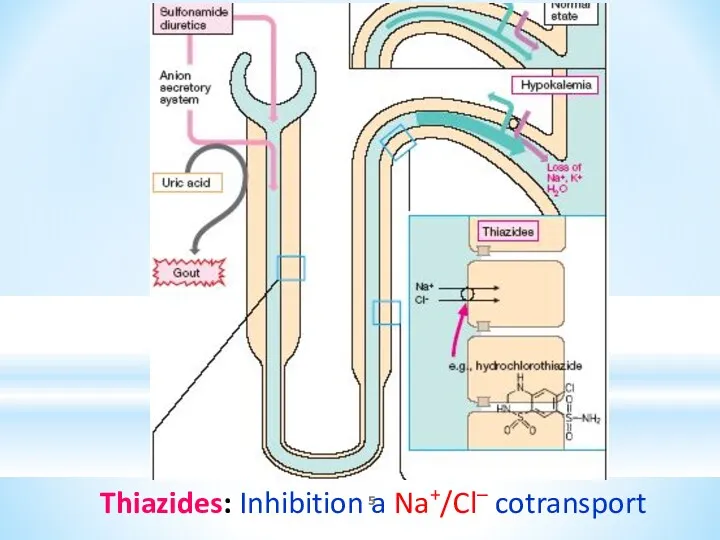
- 5. Thiazides: Inhibition a Na+/Cl– cotransport
- 6. CLINICAL USES OF THIAZIDES: 1. Hypertension 2. CHF. Thiazides can be the diuretic of choice in
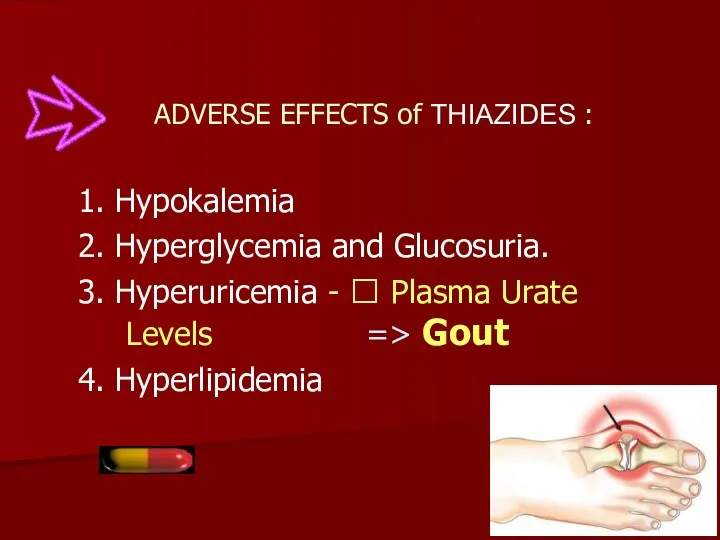
- 7. ADVERSE EFFECTS of THIAZIDES : 1. Hypokalemia 2. Hyperglycemia and Glucosuria. 3. Hyperuricemia - ? Plasma
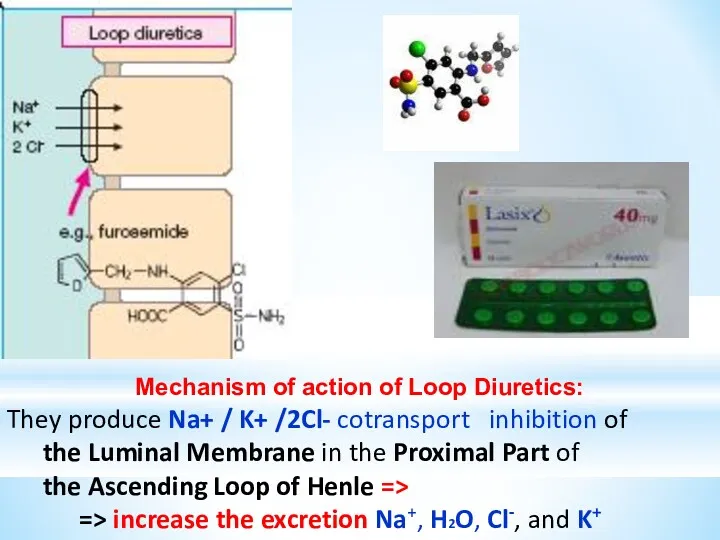
- 8. Mechanism of action of Loop Diuretics: They produce Na+ / K+ /2Cl- cotransport inhibition of the
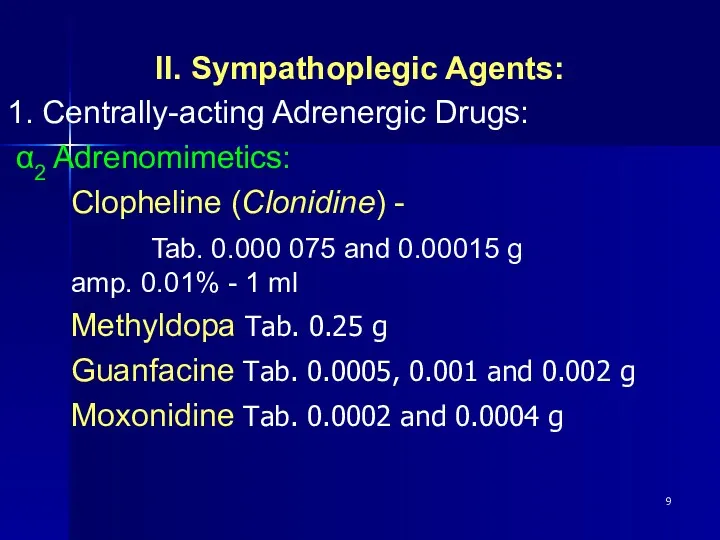
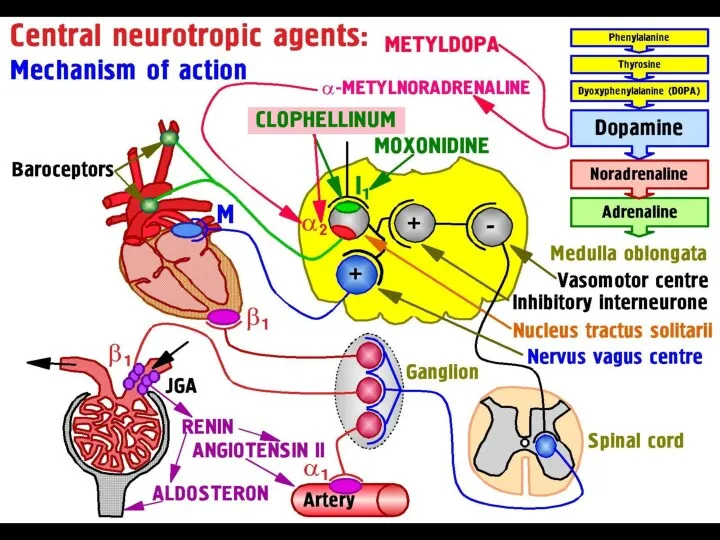
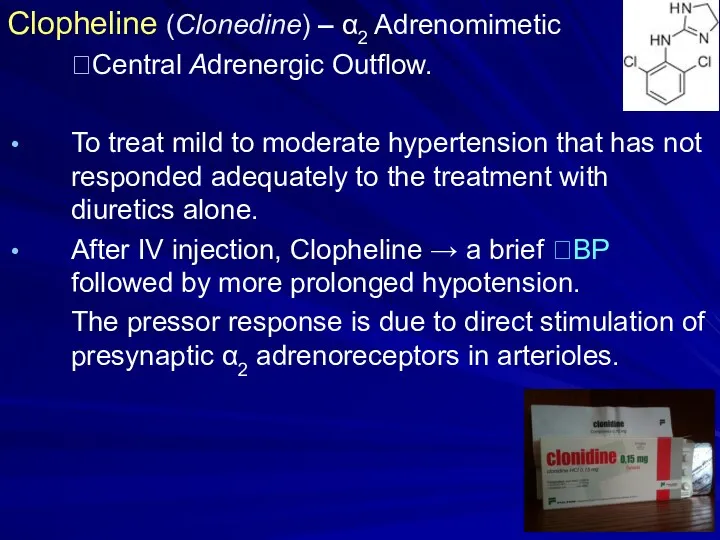
- 9. II. Sympathoplegic Agents: 1. Centrally-acting Adrenergic Drugs: α2 Adrenomimetics: Clopheline (Clonidine) - Tab. 0.000 075 and
- 11. Clopheline (Clonedine) – α2 Adrenomimetic ?Central Adrenergic Outflow. To treat mild to moderate hypertension that has
- 12. 2. Centrally and Peripherally Acting Drugs: a) Sympatholytics: Reserpine – tab. 0.1 mg and 0.25 mg
- 13. Reserpine - blocks the Mg 2+/ ATP – dependent transport of amines - Noradrenaline , Dopamine
- 16. Propranolol - a β-adrenoblocker, is useful for ?BP in mild to moderate hypertension In Severe Hypertension,
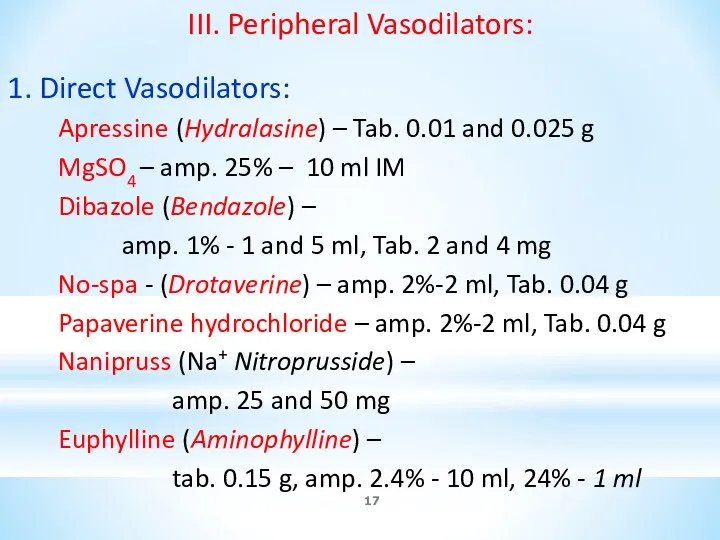
- 17. III. Peripheral Vasodilators: 1. Direct Vasodilators: Apressine (Hydralasine) – Tab. 0.01 and 0.025 g MgSO4 –
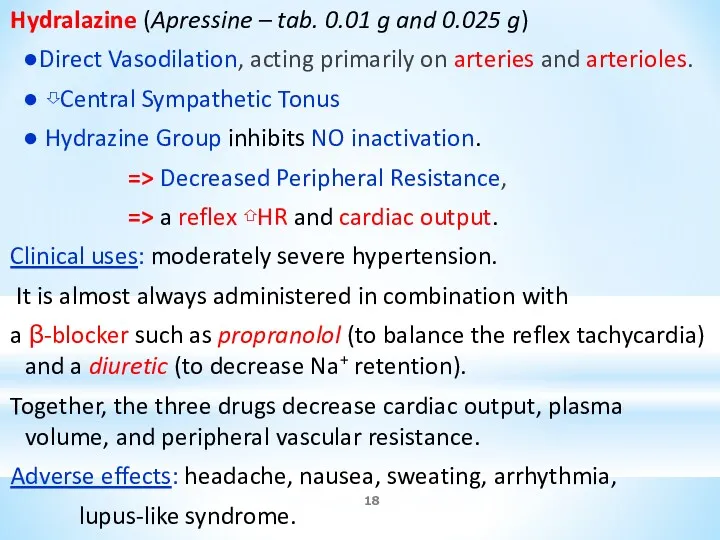
- 18. Hydralazine (Apressine – tab. 0.01 g and 0.025 g) ●Direct Vasodilation, acting primarily on arteries and
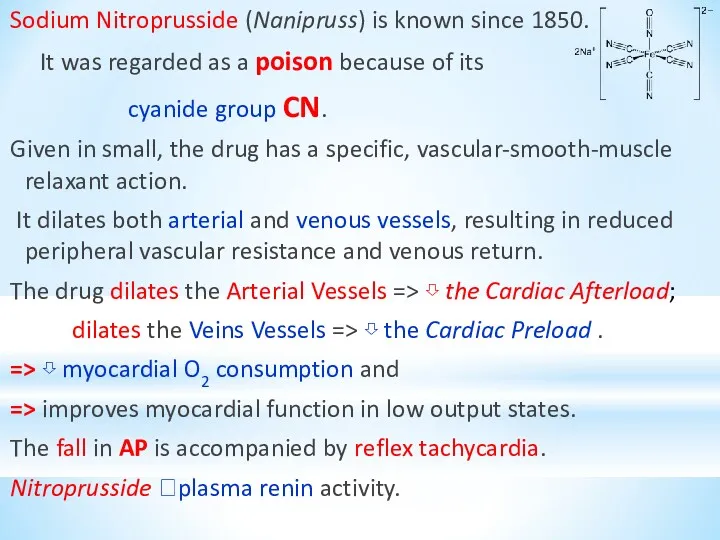
- 19. Sodium Nitroprusside (Nanipruss) is known since 1850. It was regarded as a poison because of its
- 21. 2. Calcium Channel Blockers – block high-threshold Ca2+ channels of L-type A. Diphenylalkylamines: Verapamil (Isoptin) –
- 22. 3. α1 – Blockers: - Prazosin – Tab. 1, 3, 5 mg Doxazosin – Tab. 2
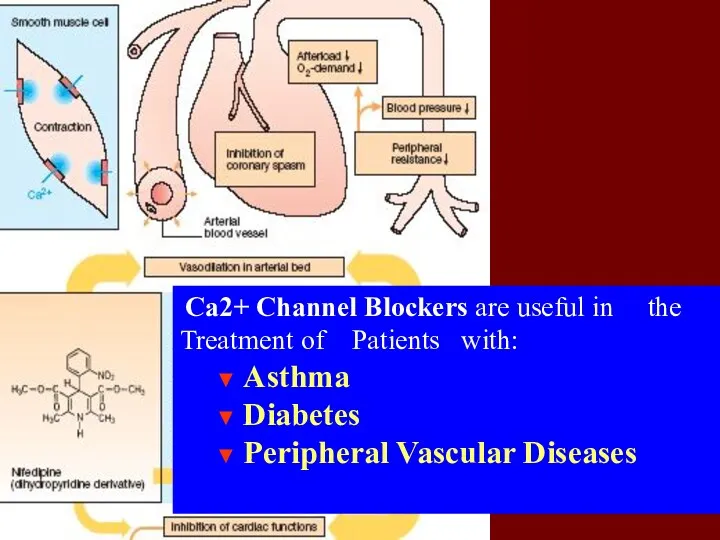
- 23. Ca2+ Channel Blockers are useful in the Treatment of Patients with: ▼ Asthma ▼ Diabetes ▼
- 24. Verapamil appears to have antianginal, antihypertensive and antiarrhythmic action. It manages unstable and chronic stable angina
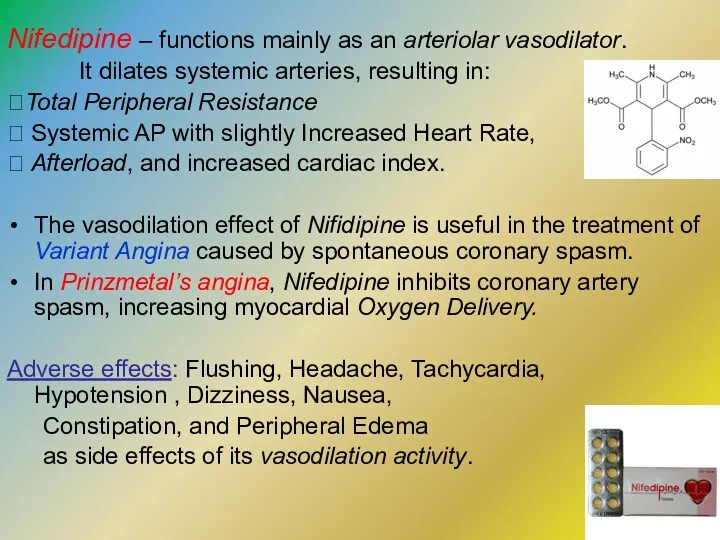
- 25. Nifedipine – functions mainly as an arteriolar vasodilator. It dilates systemic arteries, resulting in: ?Total Peripheral
- 26. Amlodipine is a Dihydropyridine compound – the 2nd Generation long-acting Ca2+ antagonist. It blocks the inward
- 27. Minoxidil – Tab. 5 mg, vial - 2%-10 ml – K+ Channel Activator. The effect results
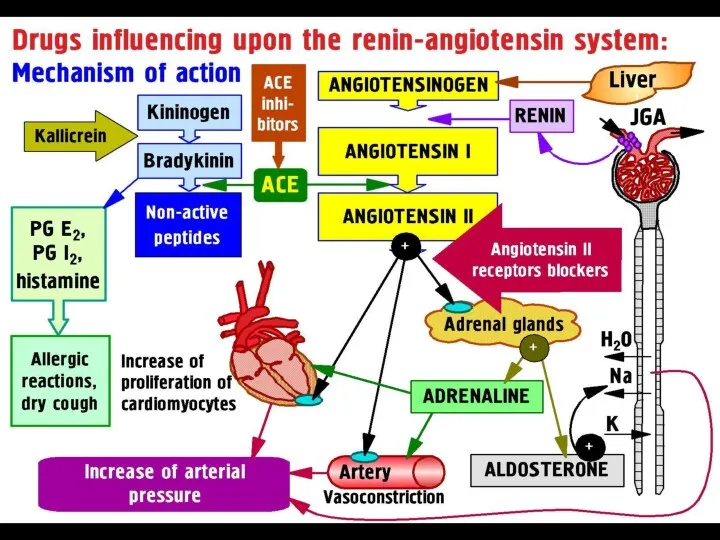
- 28. IV. Agents affecting Renin-Angiotensin System: 1). ACE Inhibitors: Captopril – Tab. 25 and 50 mg Enalapril
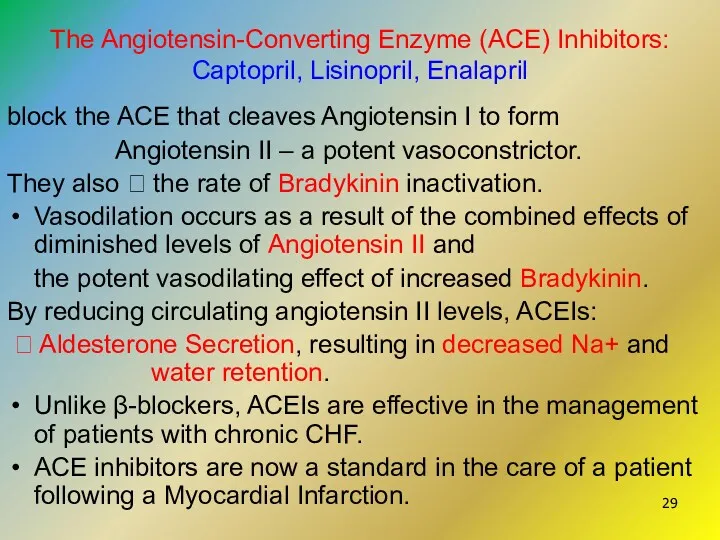
- 29. The Angiotensin-Converting Enzyme (ACE) Inhibitors: Captopril, Lisinopril, Enalapril block the ACE that cleaves Angiotensin I to
- 31. Lipid-lowering Drugs 1. Hydroxy-Methyl-Glutaryl-CoA Reductase Inhibitors: Lovastatin – tab. 20 and 40 mg Pravastatin – tab.
- 32. 3). Group of Nicotinic Acid : Nicotinic acid (Niacin) Tab. 0.05 g; 0.1 g and 0.5
- 33. Hydroxy-methylglutaryl-CoA reductase Inhibitors (Statins ): Lovastatin, Simvastatin, Pravastatin Fluvastatin, and Atorvastatin – inhibit the 1st enzymatic
- 34. Fibrates Clofibrate, Fenofibrate and Gemfibrozil – derivatives of fibric acid and are similar to Endogenous Fatty
- 35. Nicotinic acid – inhibits Lipolysis in adipose tissue – the producer of circulating Free Fatty Acids
- 36. Cholestyramine and Cholestipol are Anion Exchange Resins that bind Negatively Charged Bile Acid and Bile Salts
- 38. Скачать презентацию



 Учебно - методическое пособие. Картотека загадок.
Учебно - методическое пособие. Картотека загадок.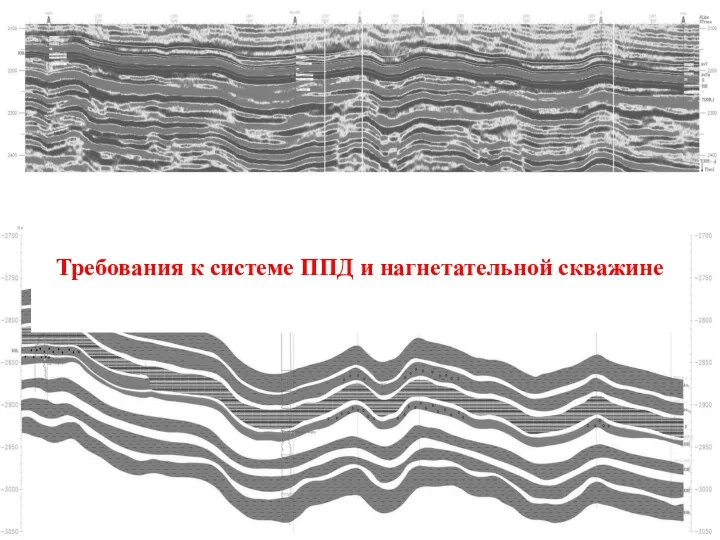 Требования к системе ППД и нагнетательной скважине
Требования к системе ППД и нагнетательной скважине Проект Фестиваль Добрый
Проект Фестиваль Добрый внутренняя и внешняя среда организации
внутренняя и внешняя среда организации Виртуальная реальность
Виртуальная реальность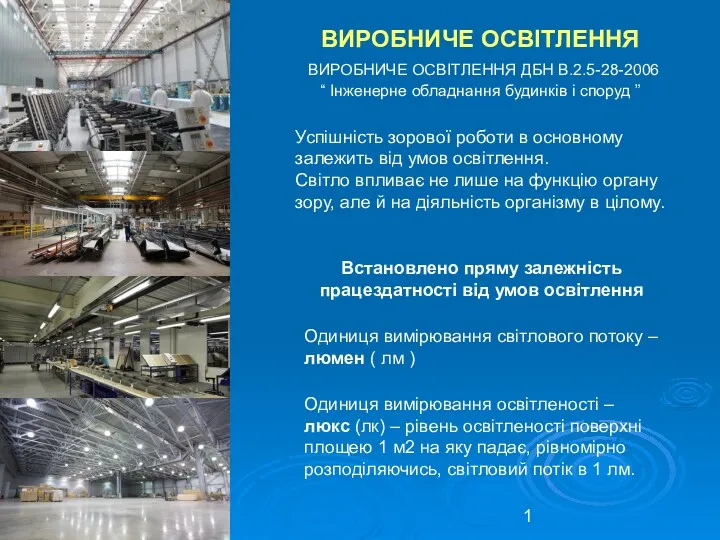 Виробниче освітлення
Виробниче освітлення Про Красную Шапочку, или как один мальчик полюбил фильм из-за музыки (2 класс)
Про Красную Шапочку, или как один мальчик полюбил фильм из-за музыки (2 класс) Презентация Наше здоровье - в наших руках
Презентация Наше здоровье - в наших руках Классическая школа управления. Школа научного менеджмента. Административная школа управления
Классическая школа управления. Школа научного менеджмента. Административная школа управления Технологии растениеводства. Технологии обработки почвы
Технологии растениеводства. Технологии обработки почвы Цунами. Тридцать шесть видов Фудзи
Цунами. Тридцать шесть видов Фудзи Русские народные игры
Русские народные игры Наполеон Бонапарт
Наполеон Бонапарт Аппараты по продаже воды
Аппараты по продаже воды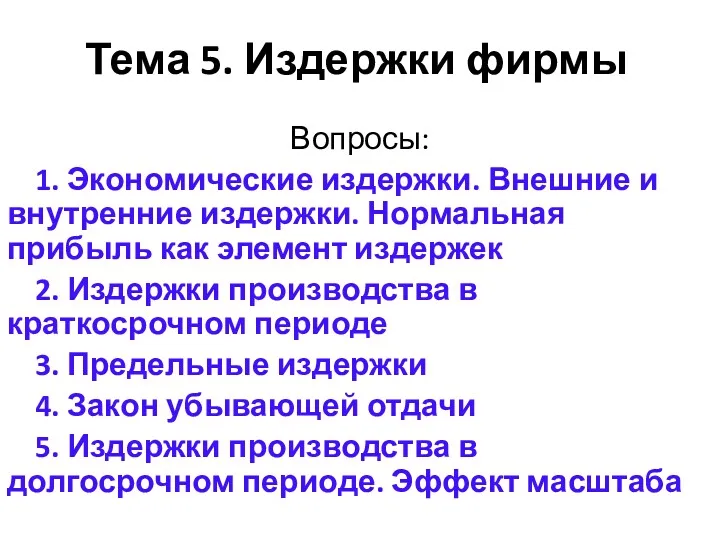 Издержки фирмы
Издержки фирмы Прямая речь
Прямая речь Использование ТКМ на уроках химии.Тема занятия Влияет ли строение вещества на его физические свойства? 11 класс
Использование ТКМ на уроках химии.Тема занятия Влияет ли строение вещества на его физические свойства? 11 класс Разработка методики расчета криогенного блока очистки гелия от высококипящих примесей
Разработка методики расчета криогенного блока очистки гелия от высококипящих примесей Виды постоянных сигналов. Их классификация и места установки
Виды постоянных сигналов. Их классификация и места установки Проектирование первого этапа строительства мусоросортировочного комплекса мощностью до 150 000 тонн твердых коммунальных отходов
Проектирование первого этапа строительства мусоросортировочного комплекса мощностью до 150 000 тонн твердых коммунальных отходов Конструирование электронных узлов приборов/ Конструирование модулей ЭС
Конструирование электронных узлов приборов/ Конструирование модулей ЭС Water Supply
Water Supply Михаил Васильевич Ломоносов - Петр Великий русской литературы
Михаил Васильевич Ломоносов - Петр Великий русской литературы Геометрический смысл производной
Геометрический смысл производной №29- Симфоническая музыка
№29- Симфоническая музыка Благодать вам и мир от Бога Отца и Господа нашего Иисуса Христа
Благодать вам и мир от Бога Отца и Господа нашего Иисуса Христа Роль школьной библиотеки в обеспечении и информационной поддержке учебно-воспитательного процесса
Роль школьной библиотеки в обеспечении и информационной поддержке учебно-воспитательного процесса Створення iPad
Створення iPad