CLASSIFICATION
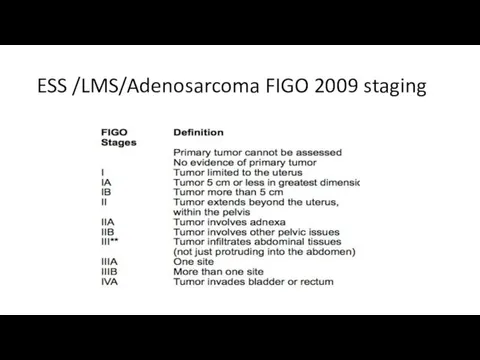
Leiomyosarcomas are now staged using the 2009 FIGO staging system[2] (previously
they were staged like endometrial carcinomas) at time of surgery.
Stage I: tumor is limited to the uterus
IA: ≤5 cm in greatest dimensionIB: >5 cmStage II: tumor extends beyond the uterus, but within the pelvis
IIA: involves adnexa of uterusIIB: involves other pelvic tissuesStage III: tumor infiltrates abdominal tissues
IIIA: 1 siteIIIB: >1 siteIIIC: regional lymph node metastasisStage IVA: invades bladder or rectum
Stage IVB: distant metastasis (including intraabdominal or inguinal lymph nodes; excluding adnexa, pelvic and abdominal tissues)
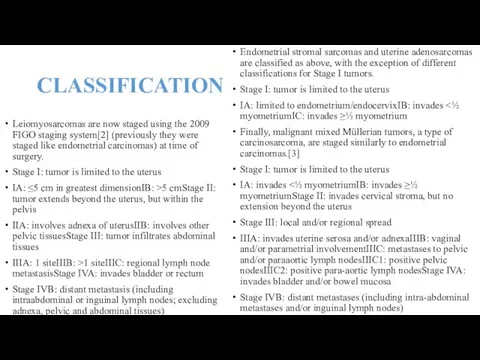
Endometrial stromal sarcomas and uterine adenosarcomas are classified as above, with the exception of different classifications for Stage I tumors.
Stage I: tumor is limited to the uterus
IA: limited to endometrium/endocervixIB: invades <½ myometriumIC: invades ≥½ myometrium
Finally, malignant mixed Müllerian tumors, a type of carcinosarcoma, are staged similarly to endometrial carcinomas.[3]
Stage I: tumor is limited to the uterus
IA: invades <½ myometriumIB: invades ≥½ myometriumStage II: invades cervical stroma, but no extension beyond the uterus
Stage III: local and/or regional spread
IIIA: invades uterine serosa and/or adnexaIIIB: vaginal and/or parametrial involvementIIIC: metastases to pelvic and/or paraaortic lymph nodesIIIC1: positive pelvic nodesIIIC2: positive para-aortic lymph nodesStage IVA: invades bladder and/or bowel mucosa
Stage IVB: distant metastases (including intra-abdominal metastases and/or inguinal lymph nodes)
 Классный час Ежели Вы вежливы
Классный час Ежели Вы вежливы Система питания двигателя от впрыска топлива
Система питания двигателя от впрыска топлива физкультминутки
физкультминутки Социально-экономическое развитие Руси в XI веке
Социально-экономическое развитие Руси в XI веке Болезни желудка и двенадцатиперстной кишки
Болезни желудка и двенадцатиперстной кишки Презентация Наши земляки - Герои Советского Союза (О брасовцах)
Презентация Наши земляки - Герои Советского Союза (О брасовцах) Презентация к празднику День матери Диск
Презентация к празднику День матери Диск Презентация к занятию Давайте разберемся! (программа Планета здоровья)
Презентация к занятию Давайте разберемся! (программа Планета здоровья) Дошкольное образование в Великобритании.
Дошкольное образование в Великобритании. Налог на имущество физических лиц
Налог на имущество физических лиц CREDO бағдарламасы. Konverter
CREDO бағдарламасы. Konverter обобщение знаний по теме Главные особенности природы Земли презентация
обобщение знаний по теме Главные особенности природы Земли презентация Предпринимательство. Защита нематериальных благ. Причинение и возмещение вреда
Предпринимательство. Защита нематериальных благ. Причинение и возмещение вреда Урок Земля отцов - моя земля!
Урок Земля отцов - моя земля! Хранение лекарственных средств
Хранение лекарственных средств Родительское собрание Подростковый алкоголизм
Родительское собрание Подростковый алкоголизм Текст и предложение
Текст и предложение Диалог между верами в целях религиозного плюрализма
Диалог между верами в целях религиозного плюрализма Презентация для работы гражданско-патриотического клуба Моя Россия
Презентация для работы гражданско-патриотического клуба Моя Россия ОСОБЕННОСТИ РАЗВИТИЯ И ВОСПИТАНИЯ ДЕТЕЙ ОТ 3 ДО 4 ЛЕТ
ОСОБЕННОСТИ РАЗВИТИЯ И ВОСПИТАНИЯ ДЕТЕЙ ОТ 3 ДО 4 ЛЕТ Дидактические системы и модели обучения, факторы и цели
Дидактические системы и модели обучения, факторы и цели Рождество
Рождество Организация медицинской помощи сельскому населению
Организация медицинской помощи сельскому населению Урок химии для 8 класса на тему Ковалентная связь.ФГОС.
Урок химии для 8 класса на тему Ковалентная связь.ФГОС. России милый уголок (презентация)
России милый уголок (презентация) Компьютерная графика
Компьютерная графика Ортопедиялық стоматологияда қолданылатын анестезия препараттары. Олардың сипаттамасы
Ортопедиялық стоматологияда қолданылатын анестезия препараттары. Олардың сипаттамасы Негізгі макроэкономикалық көрсеткіштер (мұнайға баррельіне $90 бағасы кезінде)
Негізгі макроэкономикалық көрсеткіштер (мұнайға баррельіне $90 бағасы кезінде)