Содержание
- 2. Chemotherapy of Bacterial Infections ~~~~~~~~ Antibiotics
- 3. Definitions of Antibiotics OLD: An antibiotic is a chemical substance produced by various species of microorganisms
- 4. Impact of Modern Healthcare on Life Expectancy
- 5. History Paul Ehrlich “Magic Bullet” Chemicals with selective toxicity ORIGIN: Selective Stains DRUG: Arsphenamine (1910) “606”
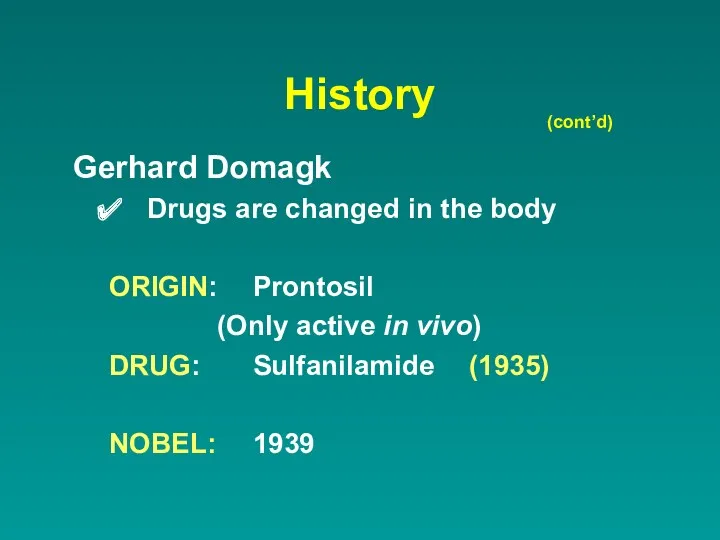
- 6. History (cont’d) Gerhard Domagk Drugs are changed in the body ORIGIN: Prontosil (Only active in vivo)
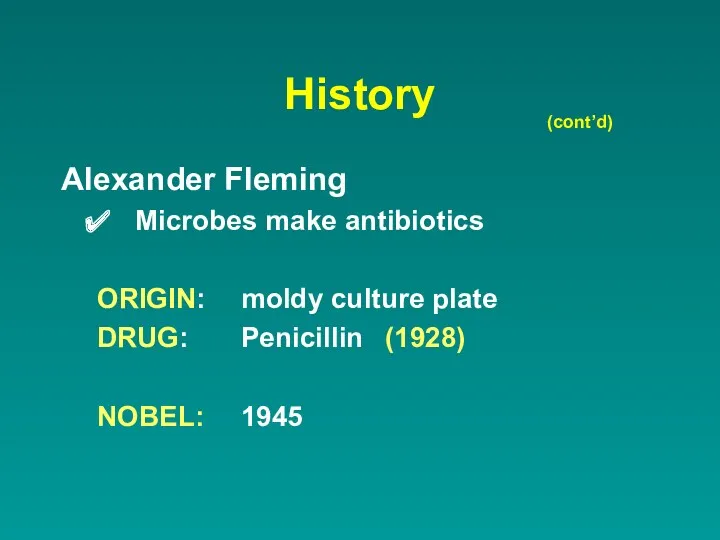
- 7. History Alexander Fleming Microbes make antibiotics ORIGIN: moldy culture plate DRUG: Penicillin (1928) NOBEL: 1945 (cont’d)
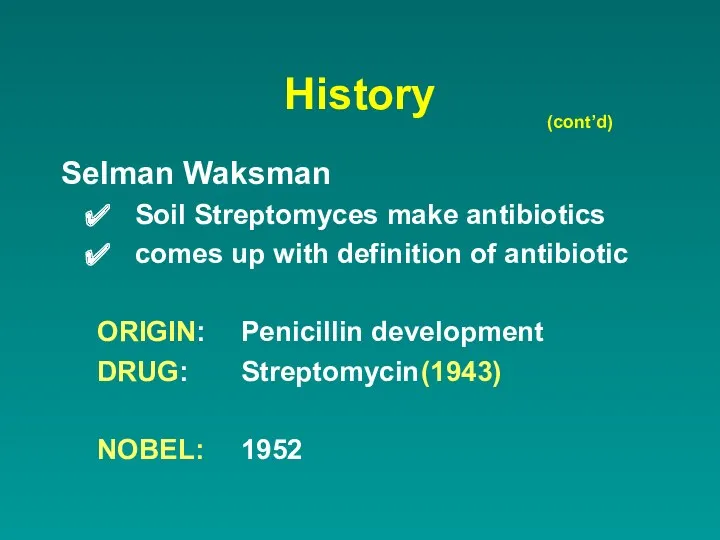
- 8. History (cont’d) Selman Waksman Soil Streptomyces make antibiotics comes up with definition of antibiotic ORIGIN: Penicillin
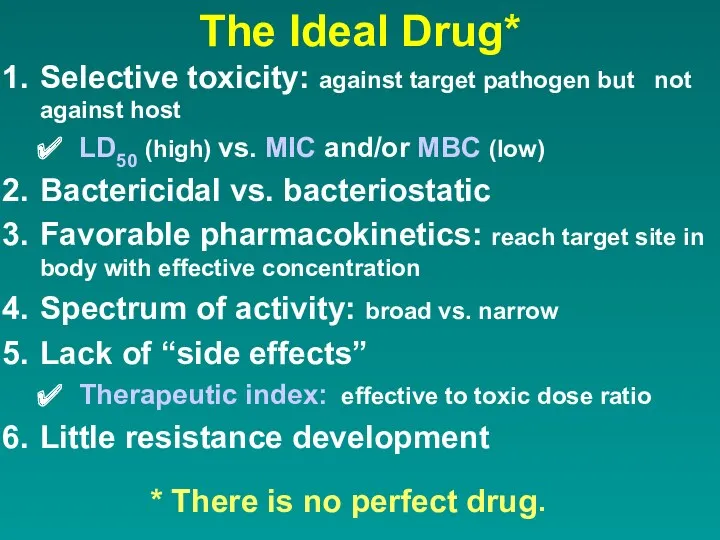
- 9. The Ideal Drug* Selective toxicity: against target pathogen but not against host LD50 (high) vs. MIC
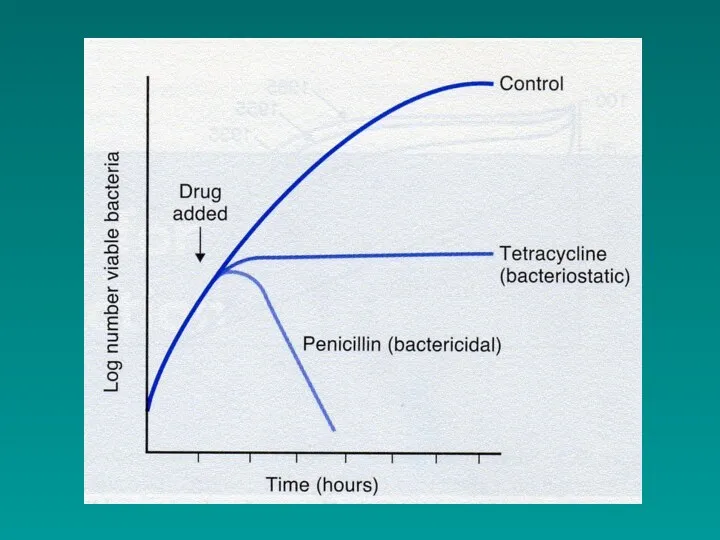
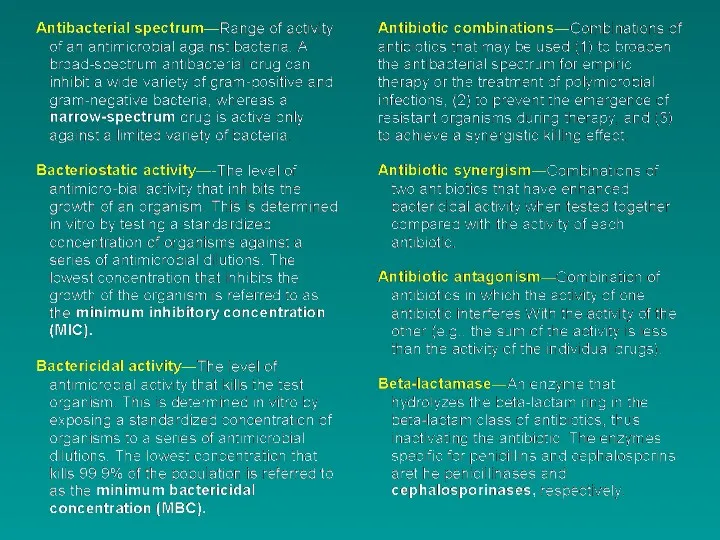
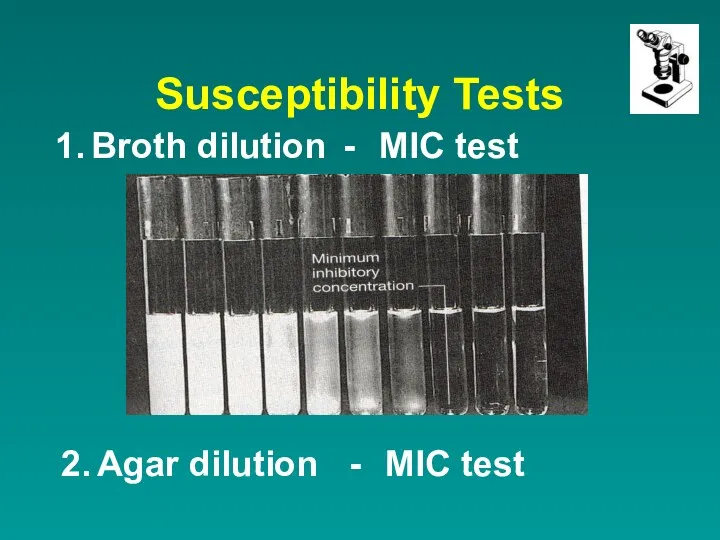
- 12. Susceptibility Tests 1. Broth dilution - MIC test 2. Agar dilution - MIC test
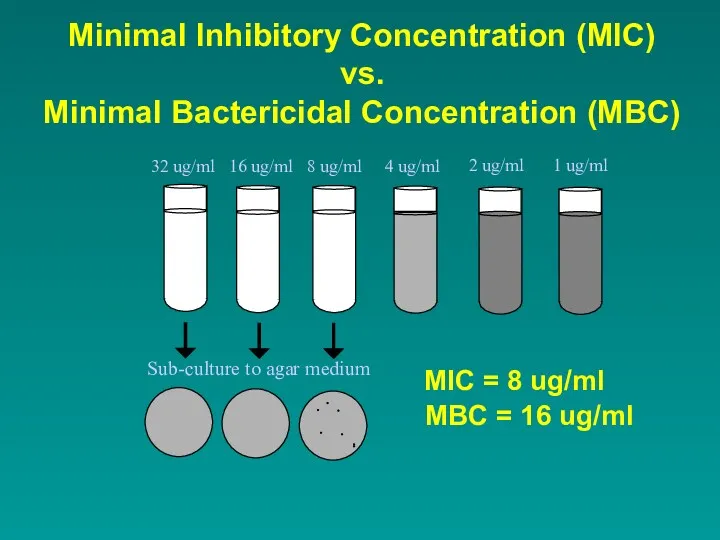
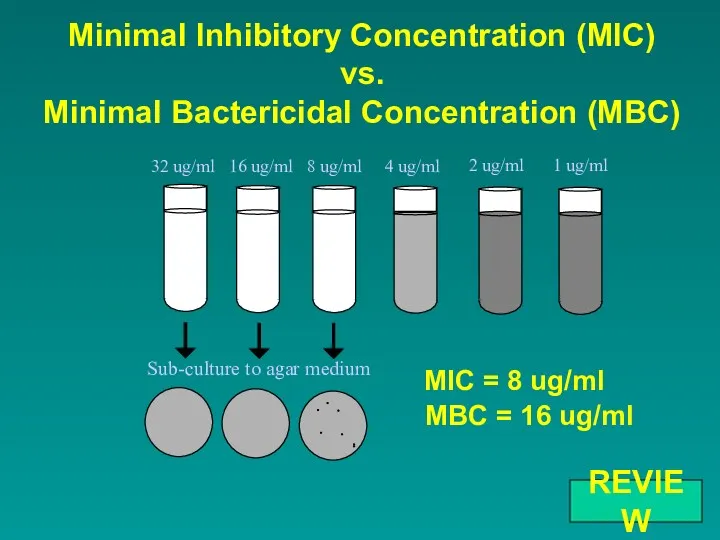
- 13. Minimal Inhibitory Concentration (MIC) vs. Minimal Bactericidal Concentration (MBC)
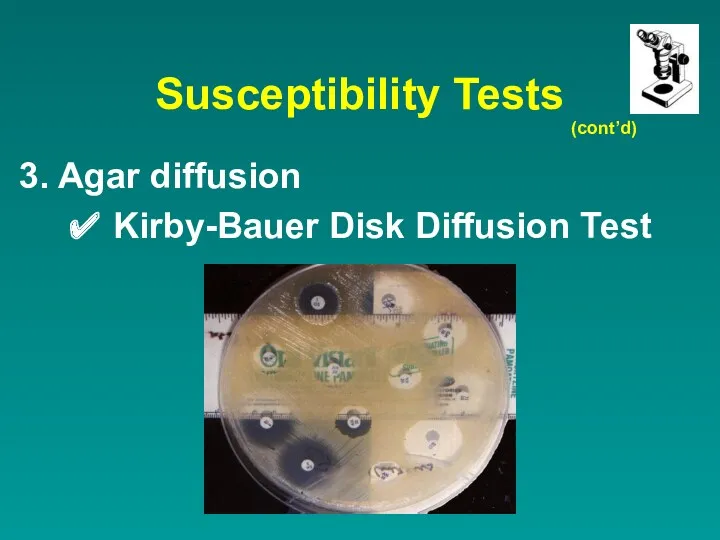
- 14. Susceptibility Tests Agar diffusion ✔ Kirby-Bauer Disk Diffusion Test (cont’d)
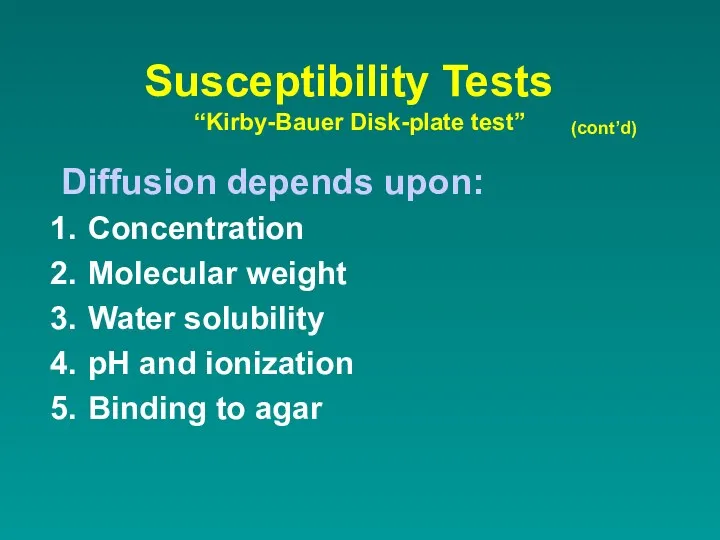
- 15. Susceptibility Tests “Kirby-Bauer Disk-plate test” Diffusion depends upon: Concentration Molecular weight Water solubility pH and ionization
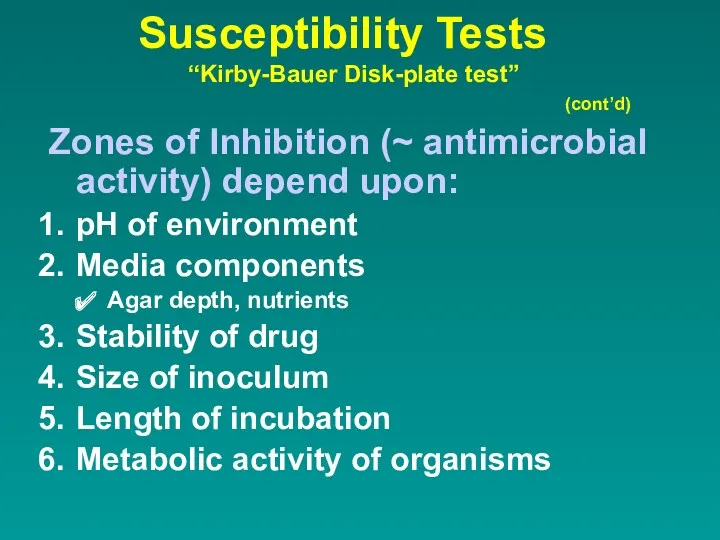
- 16. Susceptibility Tests “Kirby-Bauer Disk-plate test” Zones of Inhibition (~ antimicrobial activity) depend upon: pH of environment
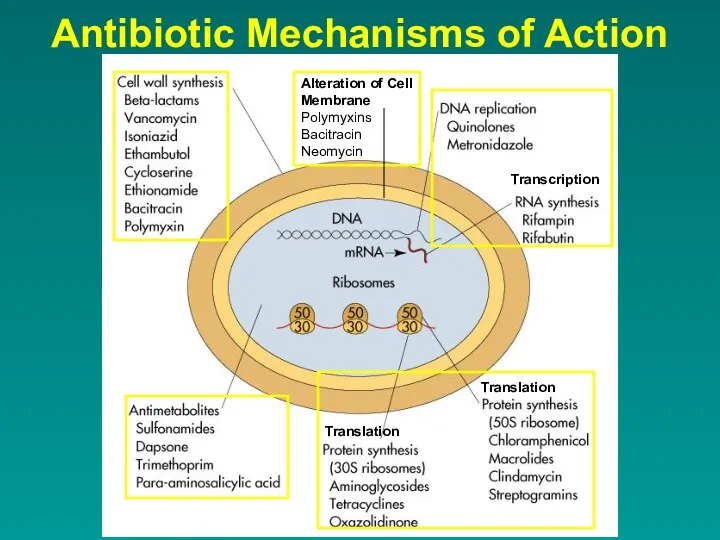
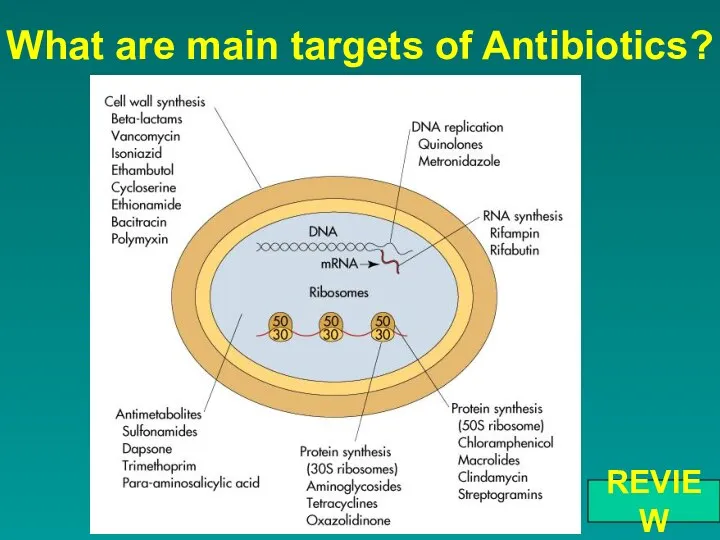
- 17. Antibiotic Mechanisms of Action Transcription Translation Translation Alteration of Cell Membrane Polymyxins Bacitracin Neomycin
- 18. Mechanism of Action ANTIMETABOLITE ACTION Sulfonamides an analog of PABA, works by competitive inhibition Trimethoprim-sulfamethoxazole a
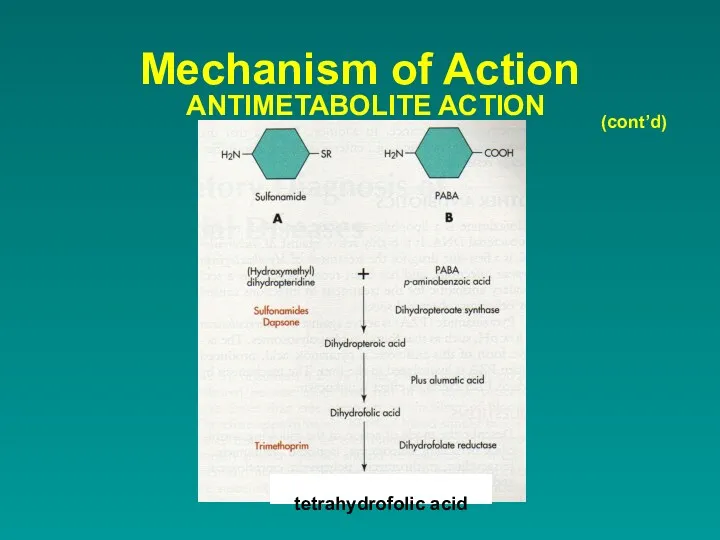
- 19. Mechanism of Action ANTIMETABOLITE ACTION (cont’d) tetrahydrofolic acid
- 20. Mechanism of Action 2. ALTERATION OF CELL MEMBRANES Polymyxins and colistin destroys membranes active against gram
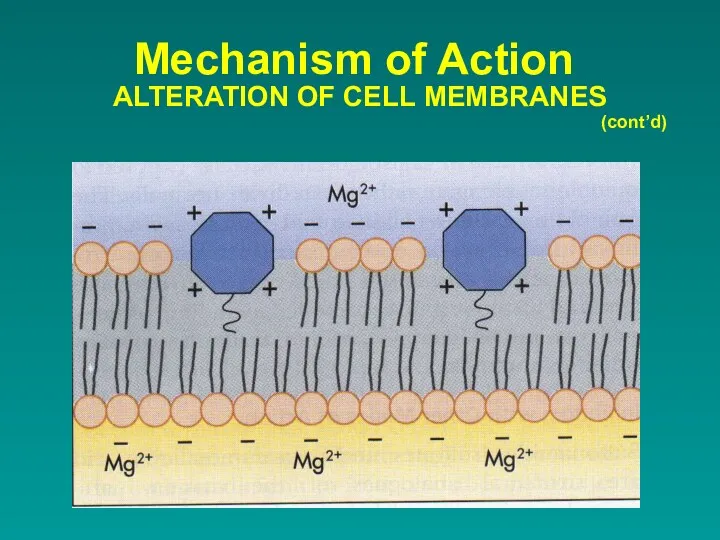
- 21. Mechanism of Action ALTERATION OF CELL MEMBRANES (cont’d)
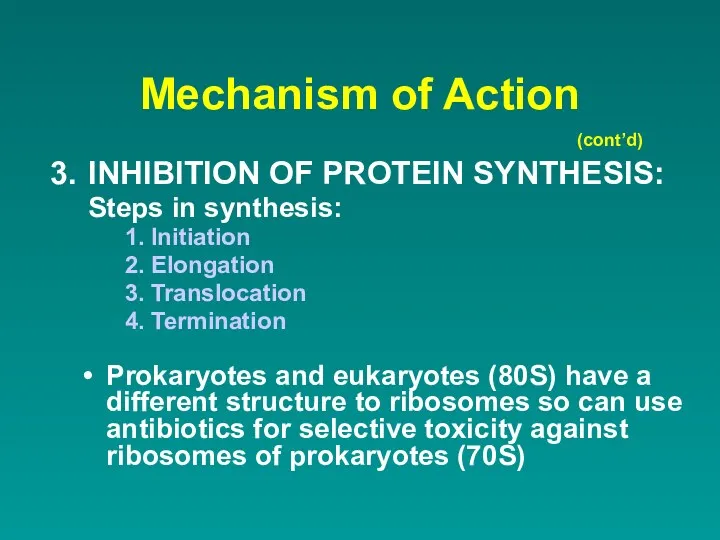
- 22. Mechanism of Action INHIBITION OF PROTEIN SYNTHESIS: Steps in synthesis: Initiation Elongation Translocation Termination (cont’d) Prokaryotes
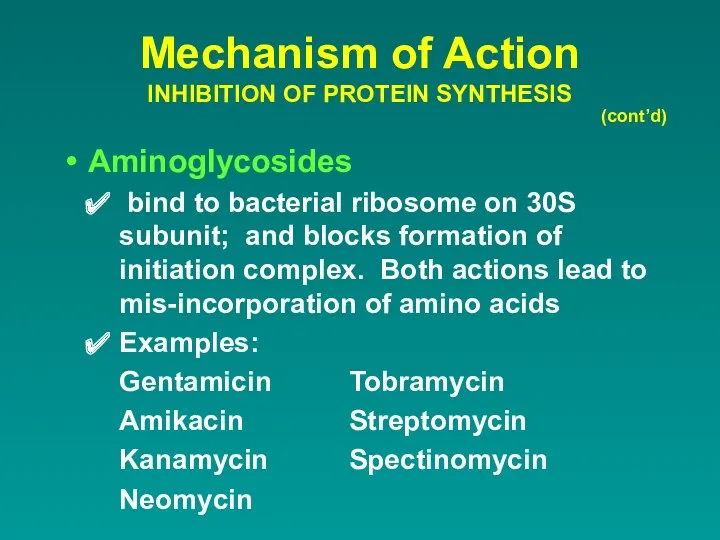
- 23. Mechanism of Action INHIBITION OF PROTEIN SYNTHESIS (cont’d) Aminoglycosides bind to bacterial ribosome on 30S subunit;
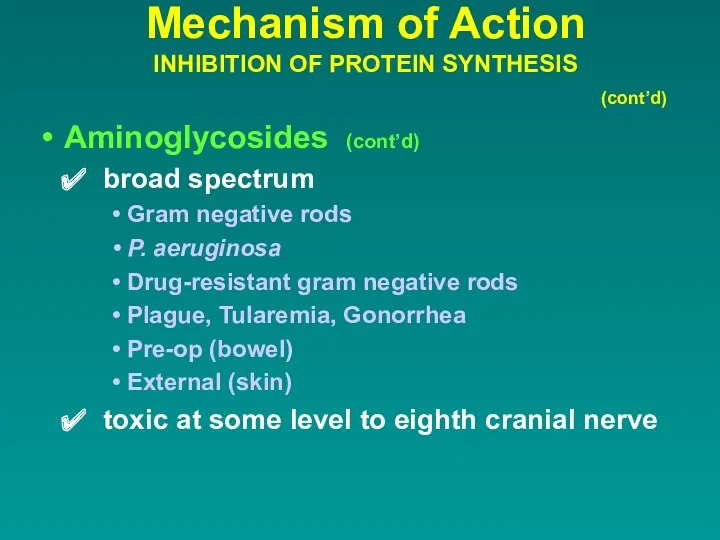
- 24. Mechanism of Action INHIBITION OF PROTEIN SYNTHESIS (cont’d) Aminoglycosides (cont’d) broad spectrum Gram negative rods P.
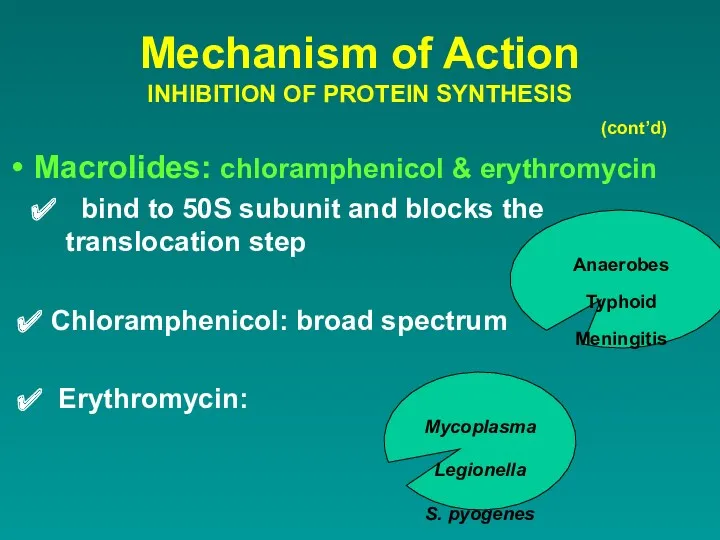
- 25. Mechanism of Action INHIBITION OF PROTEIN SYNTHESIS (cont’d) Macrolides: chloramphenicol & erythromycin bind to 50S subunit
- 26. Mechanism of Action INHIBITION OF PROTEIN SYNTHESIS (cont’d) Clindamycin binds to 50S subunit and interferes with
- 27. Tetracyclines bind to 30S subunit and interferes with the attachment of the tRNA carrying amino acids
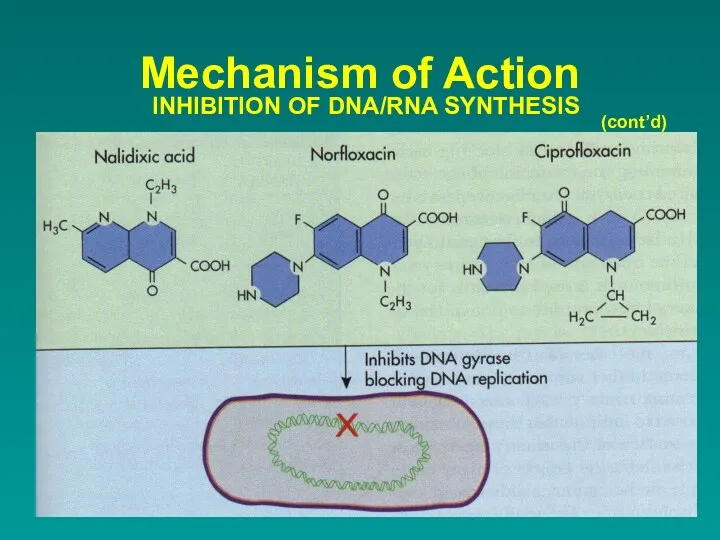
- 28. Mechanism of Action 4. INHIBITION OF DNA/RNA SYNTHESIS Rifampin binds to RNA polymerase active against gram
- 29. Mechanism of Action INHIBITION OF DNA/RNA SYNTHESIS Metronidazole breaks down into intermediate that causes breakage of
- 30. (cont’d) Mechanism of Action INHIBITION OF DNA/RNA SYNTHESIS
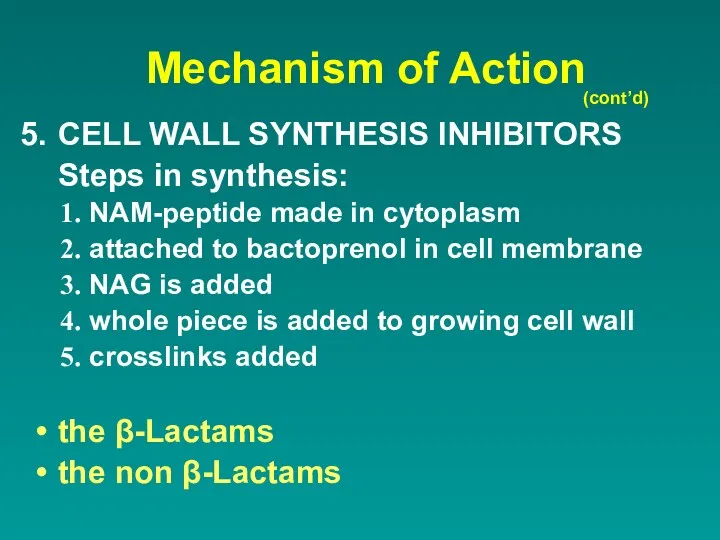
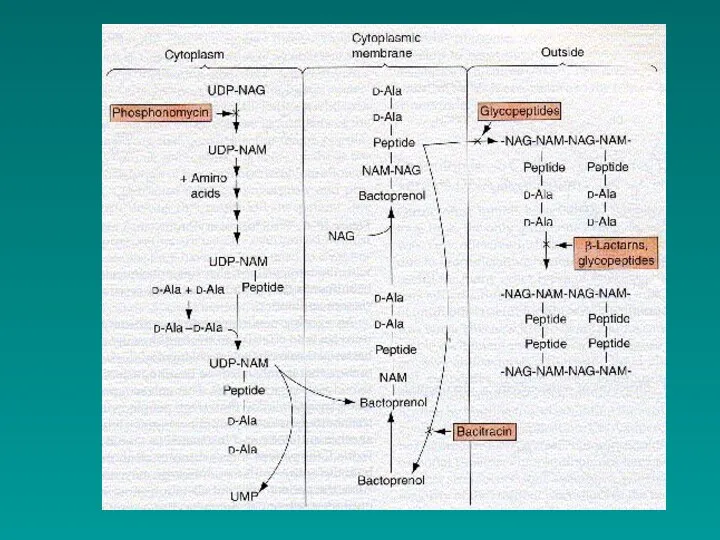
- 31. Mechanism of Action CELL WALL SYNTHESIS INHIBITORS Steps in synthesis: NAM-peptide made in cytoplasm attached to
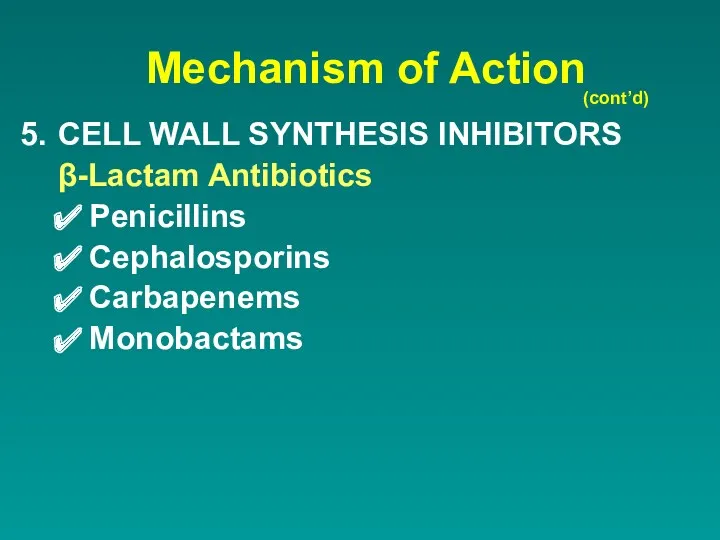
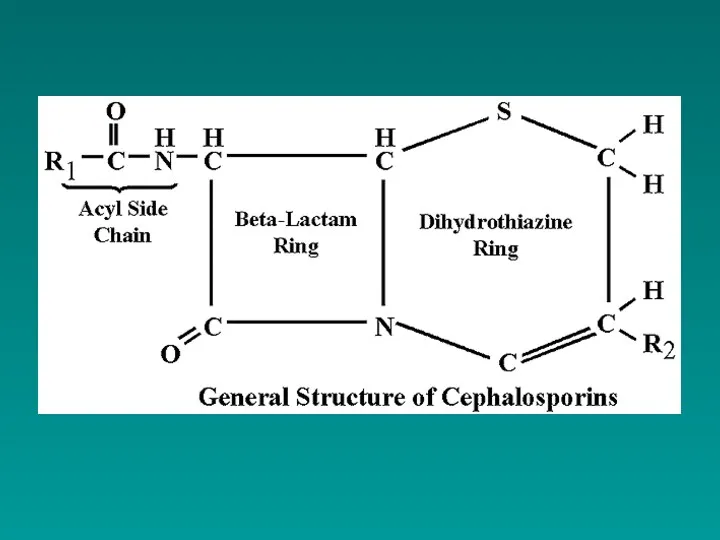
- 33. Mechanism of Action CELL WALL SYNTHESIS INHIBITORS β-Lactam Antibiotics Penicillins Cephalosporins Carbapenems Monobactams (cont’d)
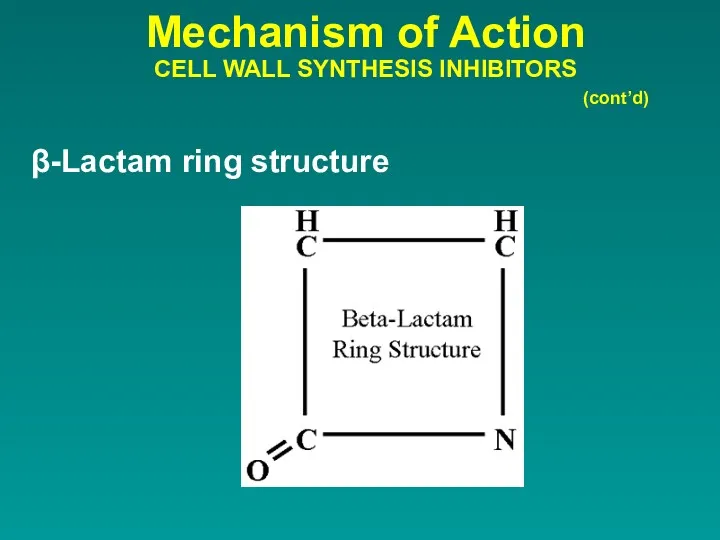
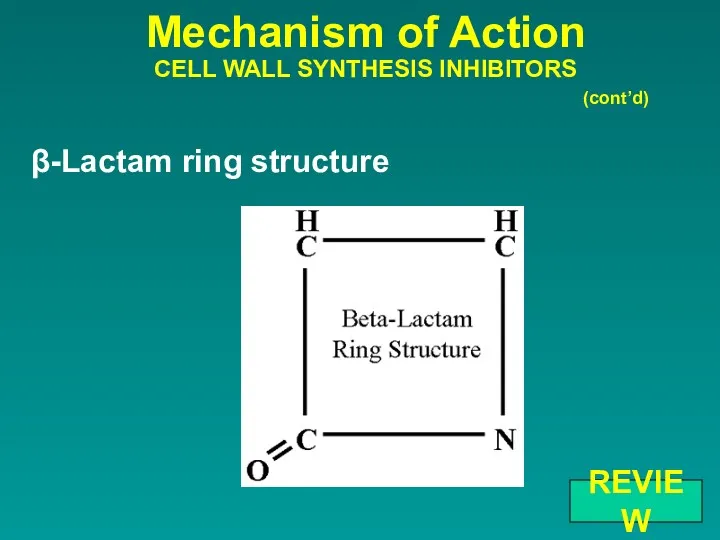
- 34. Mechanism of Action CELL WALL SYNTHESIS INHIBITORS β-Lactam ring structure (cont’d)
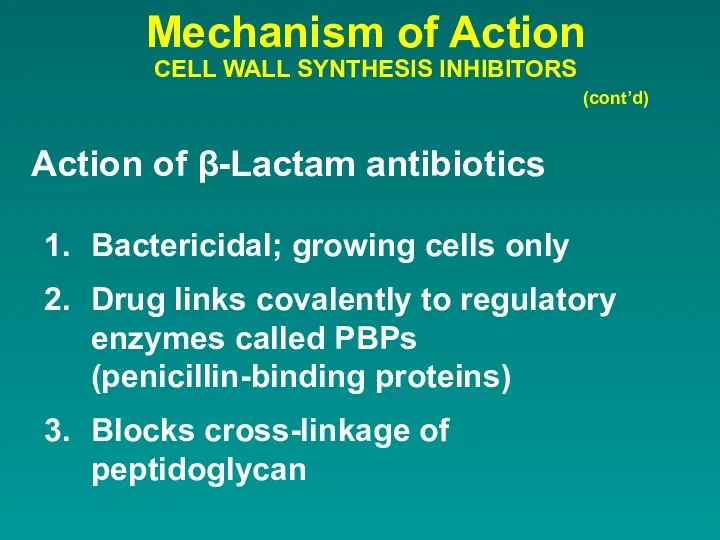
- 36. Mechanism of Action CELL WALL SYNTHESIS INHIBITORS Action of β-Lactam antibiotics (cont’d) Bactericidal; growing cells only
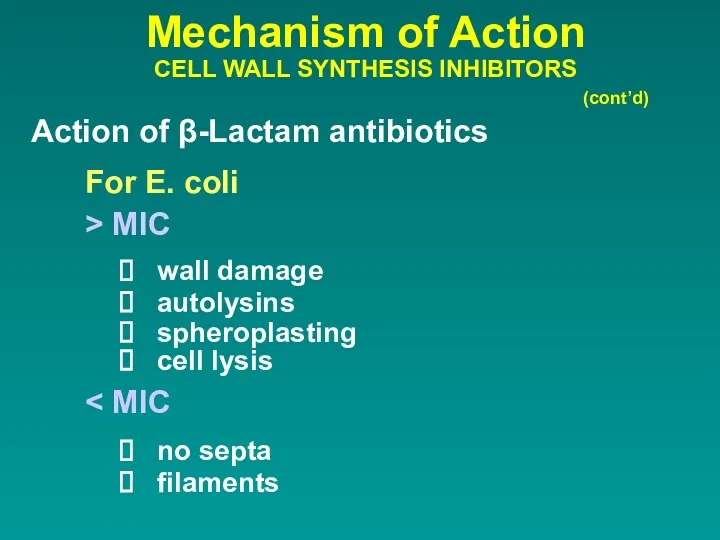
- 37. Mechanism of Action CELL WALL SYNTHESIS INHIBITORS Action of β-Lactam antibiotics (cont’d) For E. coli >
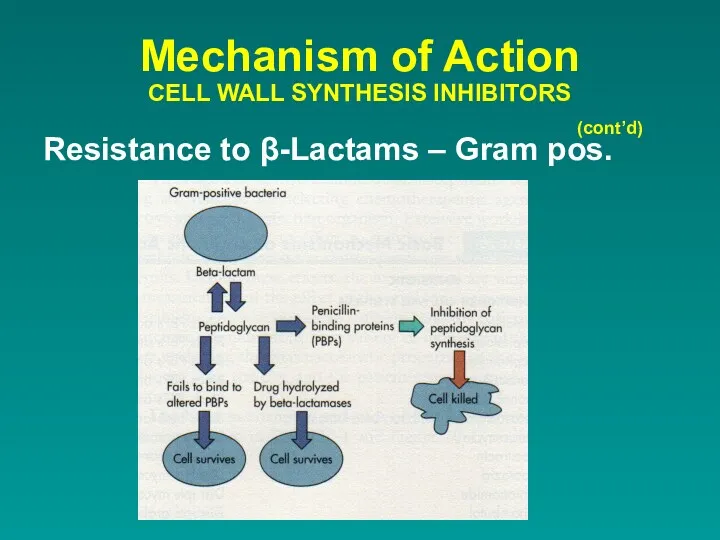
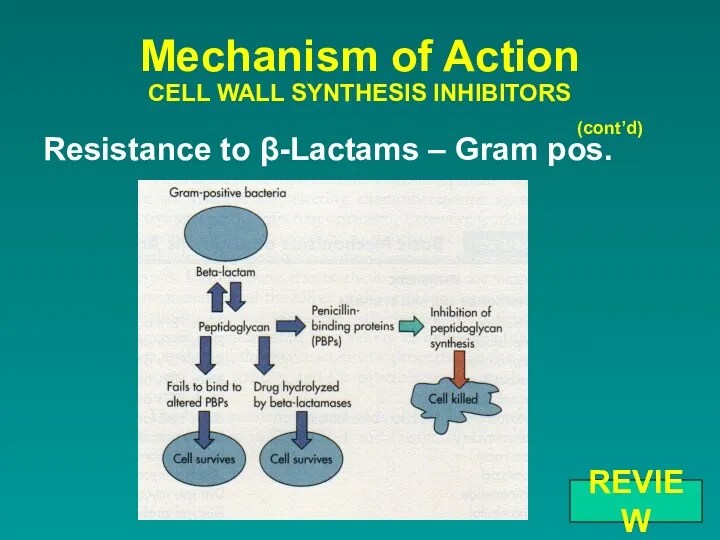
- 39. Resistance to β-Lactams – Gram pos. Mechanism of Action CELL WALL SYNTHESIS INHIBITORS (cont’d)
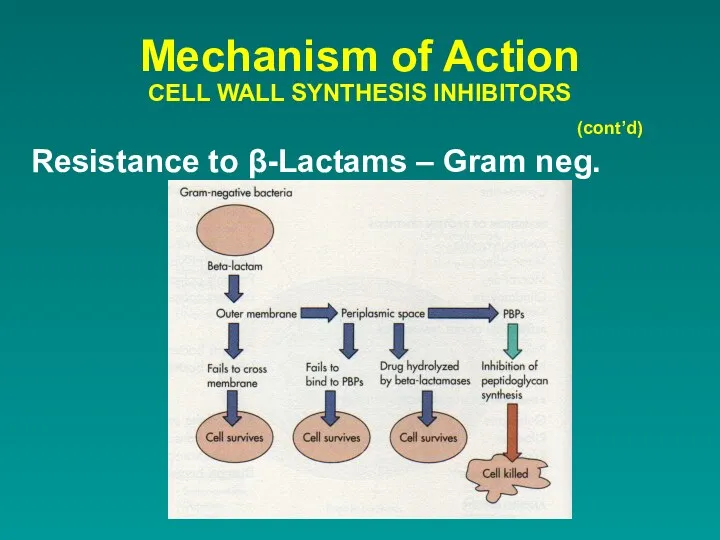
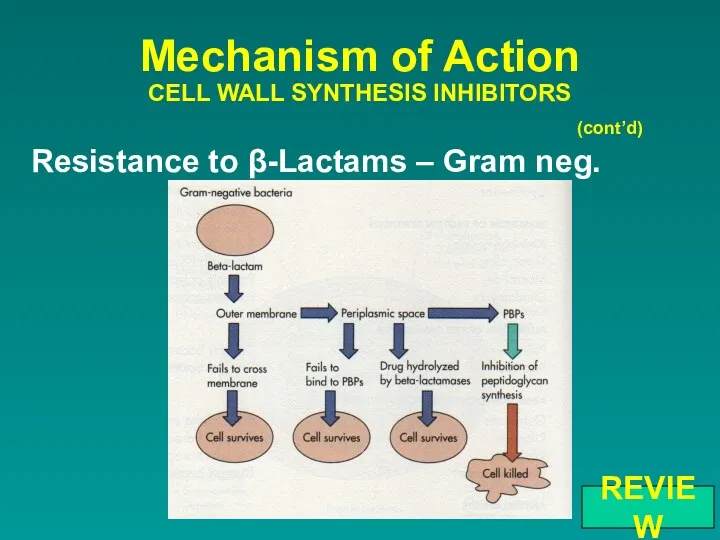
- 40. Resistance to β-Lactams – Gram neg. Mechanism of Action CELL WALL SYNTHESIS INHIBITORS (cont’d)
- 41. Non - β-Lactams Mechanism of Action CELL WALL SYNTHESIS INHIBITORS (cont’d) Vancomycin active against gram positive
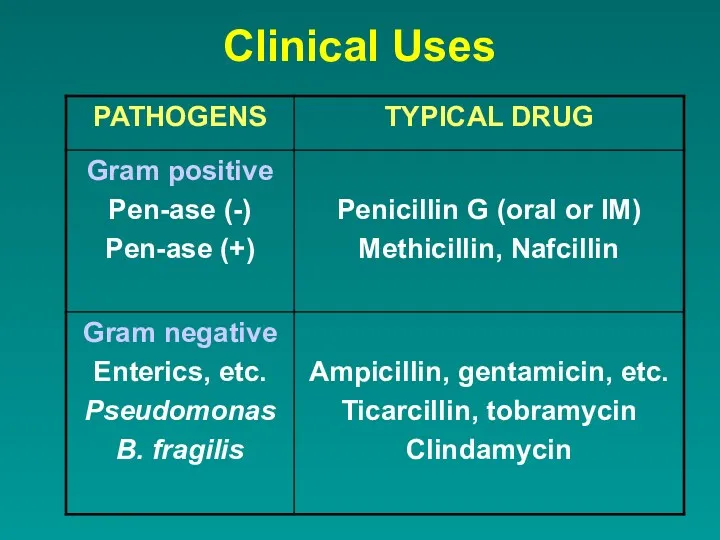
- 42. Clinical Uses
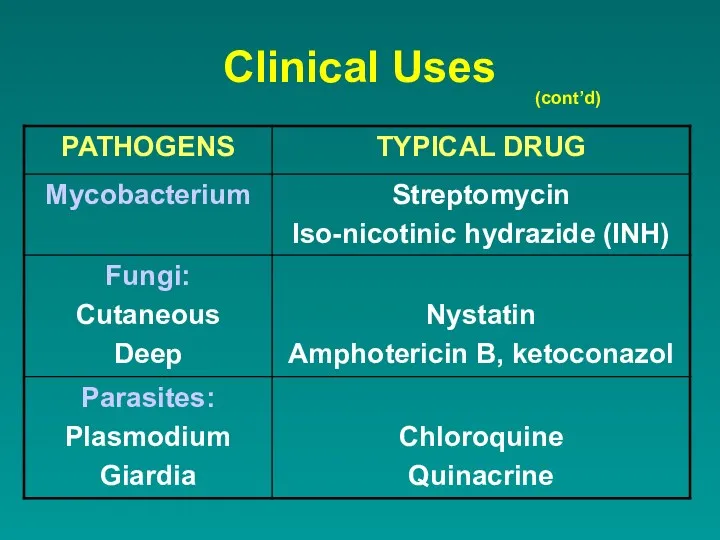
- 43. Clinical Uses (cont’d)
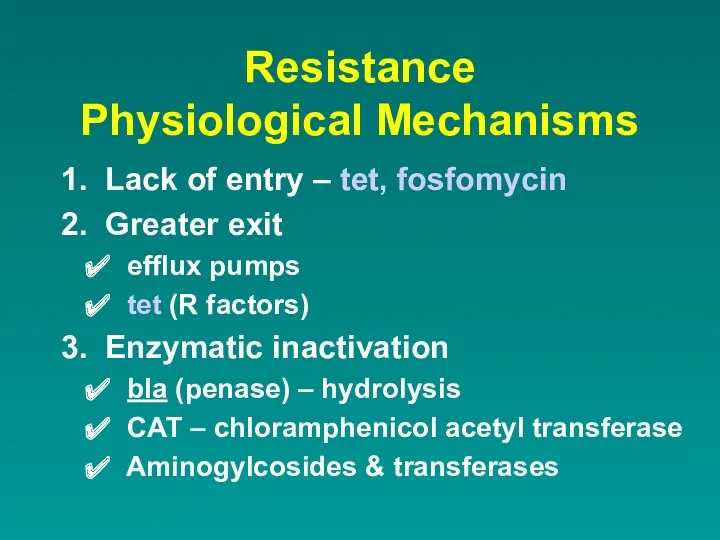
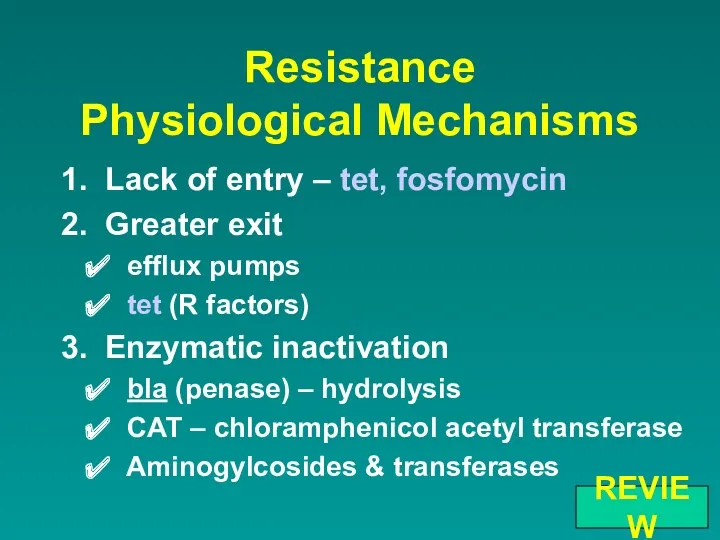
- 44. Resistance Physiological Mechanisms 1. Lack of entry – tet, fosfomycin 2. Greater exit efflux pumps tet
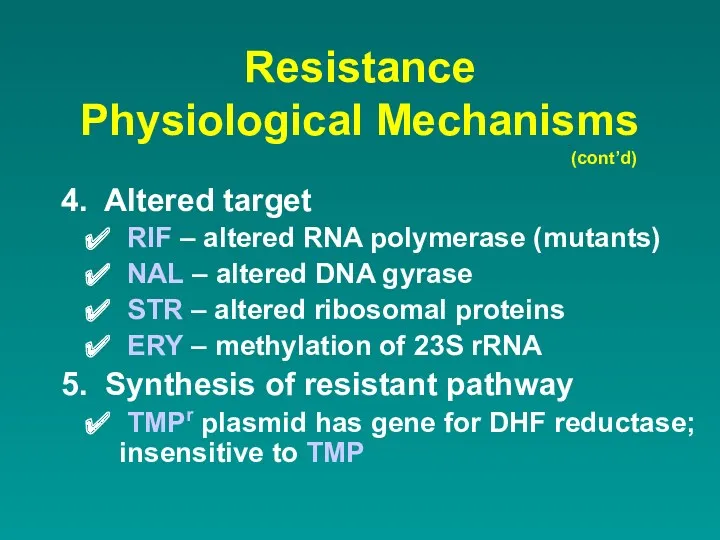
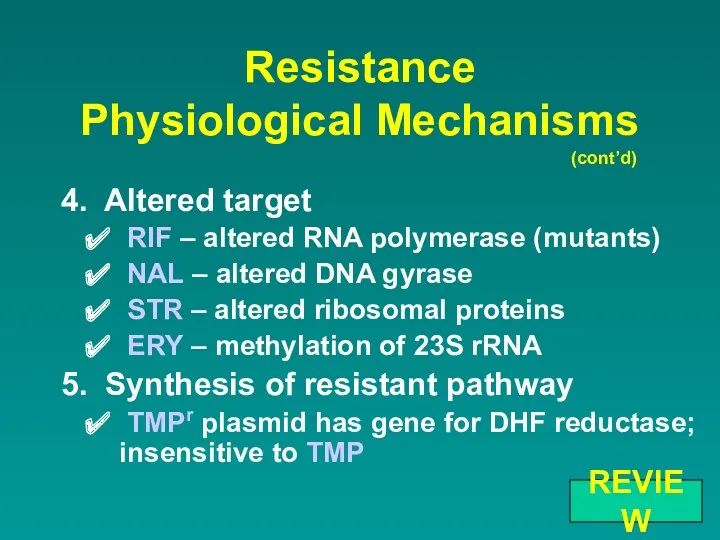
- 45. Resistance Physiological Mechanisms 4. Altered target RIF – altered RNA polymerase (mutants) NAL – altered DNA
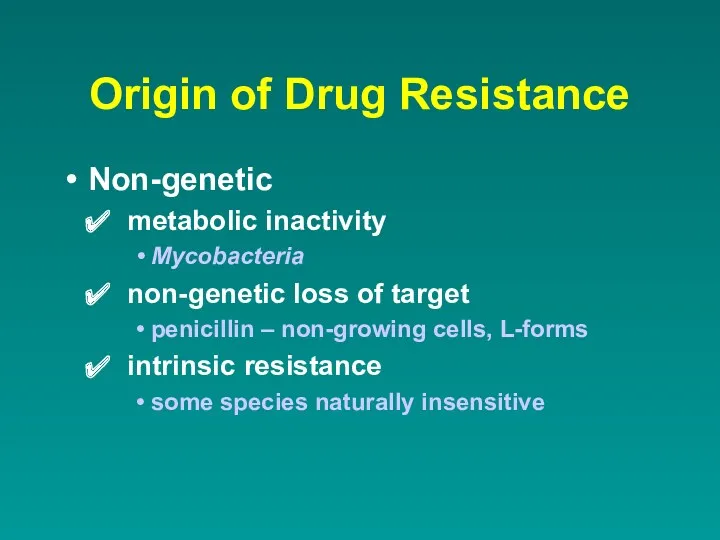
- 46. Origin of Drug Resistance Non-genetic metabolic inactivity Mycobacteria non-genetic loss of target penicillin – non-growing cells,
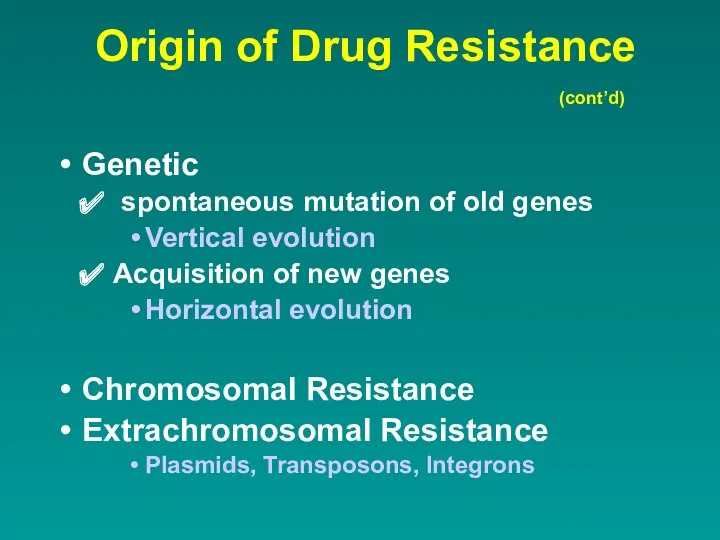
- 47. Origin of Drug Resistance Genetic spontaneous mutation of old genes Vertical evolution Acquisition of new genes
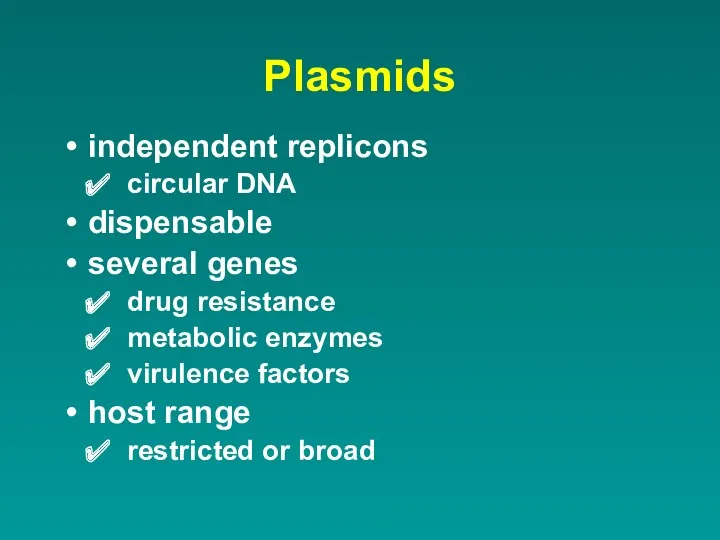
- 48. Plasmids independent replicons circular DNA dispensable several genes drug resistance metabolic enzymes virulence factors host range
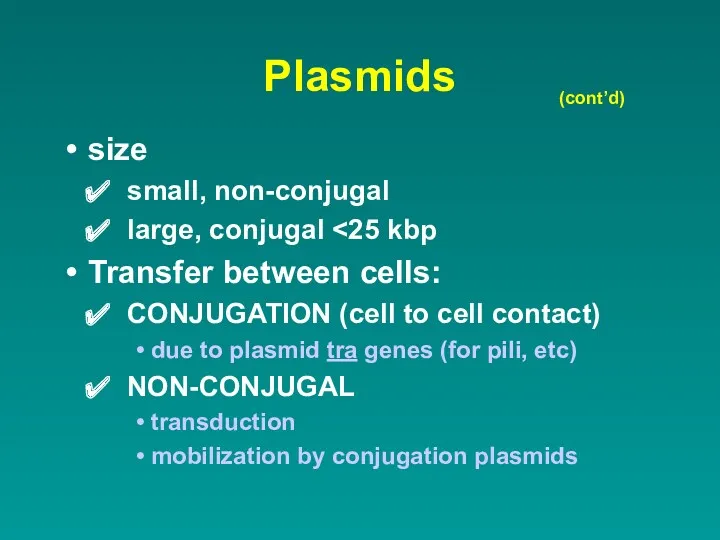
- 49. Plasmids size small, non-conjugal large, conjugal Transfer between cells: CONJUGATION (cell to cell contact) due to
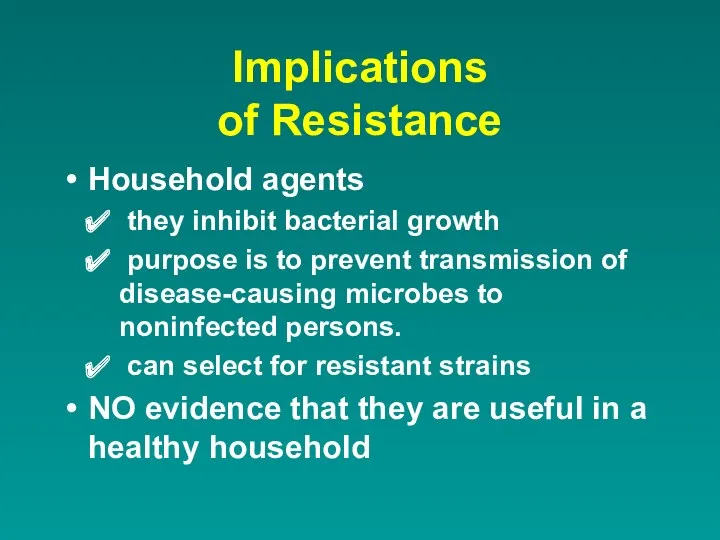
- 50. Implications of Resistance Household agents they inhibit bacterial growth purpose is to prevent transmission of disease-causing
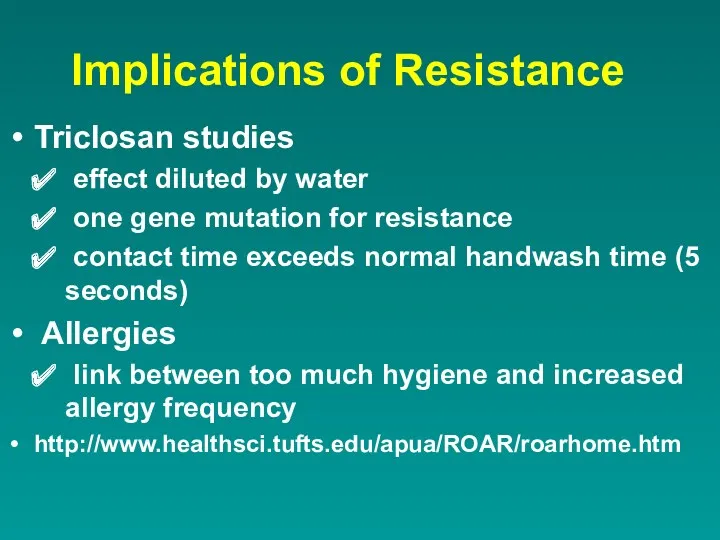
- 51. Implications of Resistance Triclosan studies effect diluted by water one gene mutation for resistance contact time
- 52. Implications of Resistance www.roar.apua.org
- 54. REVIEW
- 55. Minimal Inhibitory Concentration (MIC) vs. Minimal Bactericidal Concentration (MBC) REVIEW
- 56. What are main targets of Antibiotics? REVIEW
- 57. Mechanism of Action INHIBITION OF CELL WALL SYNTHESIS β-Lactams Non β-Lactams REVIEW
- 58. Mechanism of Action CELL WALL SYNTHESIS INHIBITORS β-Lactam ring structure (cont’d) REVIEW
- 59. Mechanism of Action Aminoglycosides Macrolides Chloramphenicol Erythromycin Tetracyclines Clindamycin INHIBITION OF PROTEIN SYNTHESIS REVIEW
- 60. Mechanism of Action INHIBITION OF NUCLEIC ACID SYNTHESIS Rifampin Metronidazole Quinolones and fluoroquinolones REVIEW
- 61. Mechanism of Action DISRUPTION OF CELL MEMBRANES Polymyxins Colistin REVIEW
- 62. Mechanism of Action ANTIMETABOLITE ACTION Sulfonamides Trimethoprim-sulfamethoxazole REVIEW
- 63. Resistance Physiological Mechanisms 1. Lack of entry – tet, fosfomycin 2. Greater exit efflux pumps tet
- 64. Resistance Physiological Mechanisms 4. Altered target RIF – altered RNA polymerase (mutants) NAL – altered DNA
- 65. Resistance to β-Lactams – Gram pos. Mechanism of Action CELL WALL SYNTHESIS INHIBITORS (cont’d) REVIEW
- 66. Resistance to β-Lactams – Gram neg. Mechanism of Action CELL WALL SYNTHESIS INHIBITORS (cont’d) REVIEW
- 68. Скачать презентацию



 здоровьем дорожить умейте 1 часть
здоровьем дорожить умейте 1 часть Цитология. Клеточная теория. Строение клетки
Цитология. Клеточная теория. Строение клетки Водоросли
Водоросли Оплодотворение. Строение половых клеток
Оплодотворение. Строение половых клеток Организация деятельности учащихся при компьютерном эксперименте
Организация деятельности учащихся при компьютерном эксперименте Деление клеток, мейоз
Деление клеток, мейоз Нервная система
Нервная система Безпека харчування в умовах ситуацій воєнного стану
Безпека харчування в умовах ситуацій воєнного стану Биологические задачи. Подготовка к ЕГЭ
Биологические задачи. Подготовка к ЕГЭ Генетикалық инженерия негіздері
Генетикалық инженерия негіздері Продукты пчеловодства
Продукты пчеловодства Рослини-хижаки
Рослини-хижаки Хромосомалар
Хромосомалар Презентация Многообразие биогеоценозов
Презентация Многообразие биогеоценозов Аминокислоты. Определение молекулярной формулы органического вещества
Аминокислоты. Определение молекулярной формулы органического вещества Морфофункциональная характеристика черепа
Морфофункциональная характеристика черепа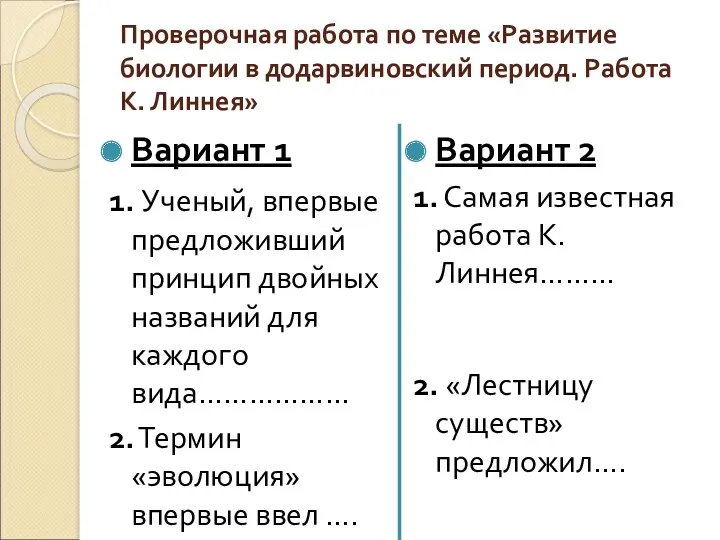 Проверочная работа по теме Развитие биологии в додарвиновский период. Работа К. Линнея
Проверочная работа по теме Развитие биологии в додарвиновский период. Работа К. Линнея Строение и функции кожи
Строение и функции кожи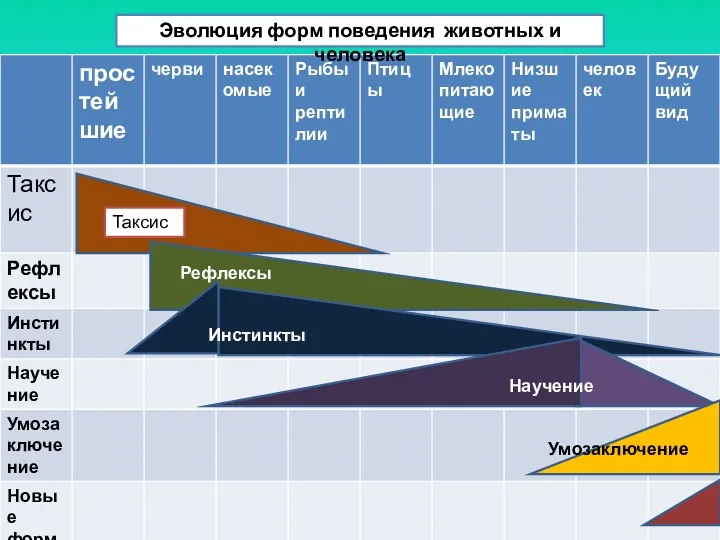 Эволюция форм поведения животных и человека
Эволюция форм поведения животных и человека Органоиды клетки
Органоиды клетки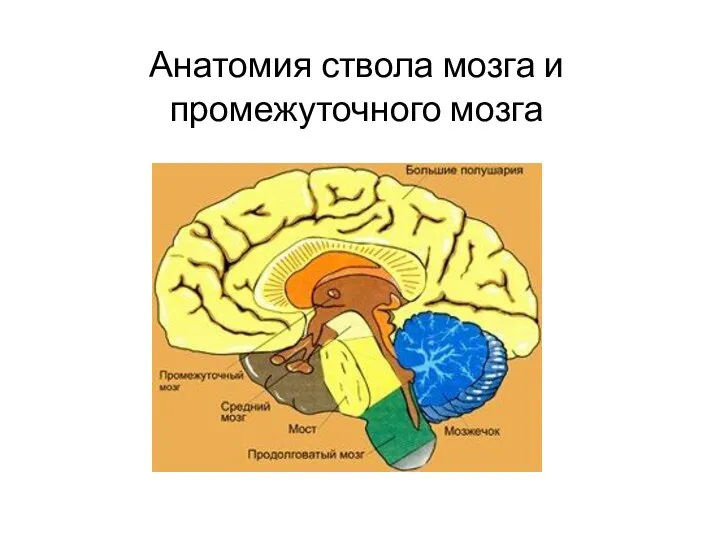 Анатомия ствола мозга и промежуточного мозга
Анатомия ствола мозга и промежуточного мозга 5 весняних квіток
5 весняних квіток Система органов чувств (сенсорная система). Зрительный анализатор
Система органов чувств (сенсорная система). Зрительный анализатор Ізоляція та видоутворення
Ізоляція та видоутворення Круги кровообращения человека. ЕГЭ
Круги кровообращения человека. ЕГЭ Такие разные насекомые. Формирование целостной картины мира в подготовительной группе
Такие разные насекомые. Формирование целостной картины мира в подготовительной группе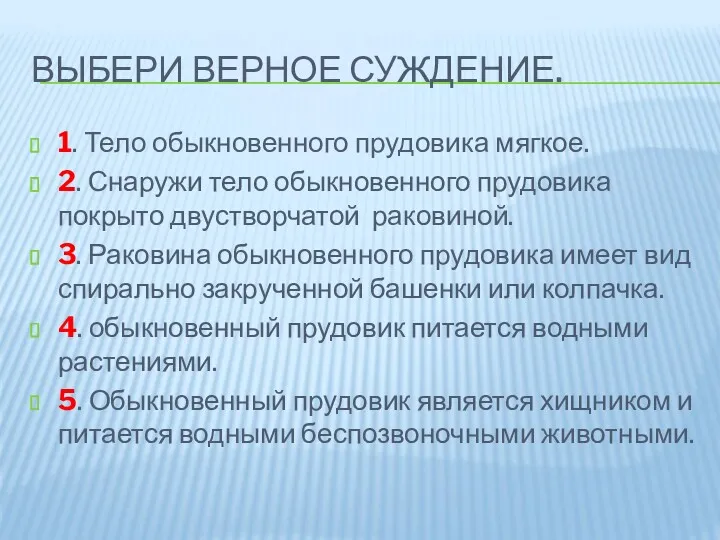 Класс двустворчатые моллюски
Класс двустворчатые моллюски Культивирование красных водорослей
Культивирование красных водорослей