Содержание
- 2. Overview: Trading Places Every organism must exchange materials with its environment. Exchanges ultimately occur at the
- 3. For most cells making up multicellular organisms, direct exchange with the environment is not possible. Gills
- 4. How does a feathery fringe help this animal survive?
- 5. Circulatory systems link exchange surfaces with cells throughout the body In small and/or thin animals, cells
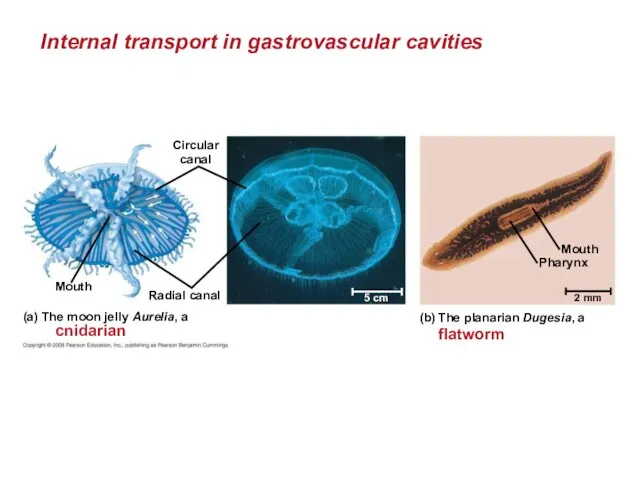
- 6. Gastrovascular Cavities Simple animals, such as cnidarians, have a body wall that is only two cells
- 7. Internal transport in gastrovascular cavities Circular canal Radial canal Mouth (a) The moon jelly Aurelia, a
- 8. Open and Closed Circulatory Systems More complex animals have either open or closed circulatory systems. Both
- 9. In insects, other arthropods, and most molluscs, blood bathes the organs directly in an open circulatory
- 10. In a closed circulatory system, the blood is confined to vessels and is distinct from the
- 11. Open and closed circulatory systems Heart Hemolymph in sinuses surrounding organs Heart Interstitial fluid Small branch
- 12. Organization of Vertebrate Closed Circulatory Systems Humans and other vertebrates have a closed circulatory system, often
- 13. Arteries branch into arterioles and carry blood to capillaries. Networks of capillaries called capillary beds are
- 14. Vertebrate hearts contain two or more chambers. Blood enters through an atrium and is pumped out
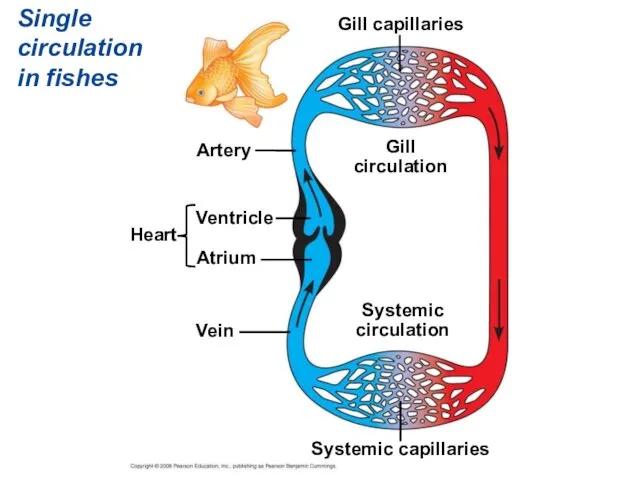
- 15. Single Circulation Bony fishes, rays, and sharks have single circulation with a two-chambered heart. In single
- 16. Single circulation in fishes Artery Ventricle Atrium Heart Vein Systemic capillaries Systemic circulation Gill circulation Gill
- 17. Double Circulation Amphibian, reptiles, and mammals have double circulation. Oxygen-poor and oxygen-rich blood are pumped separately
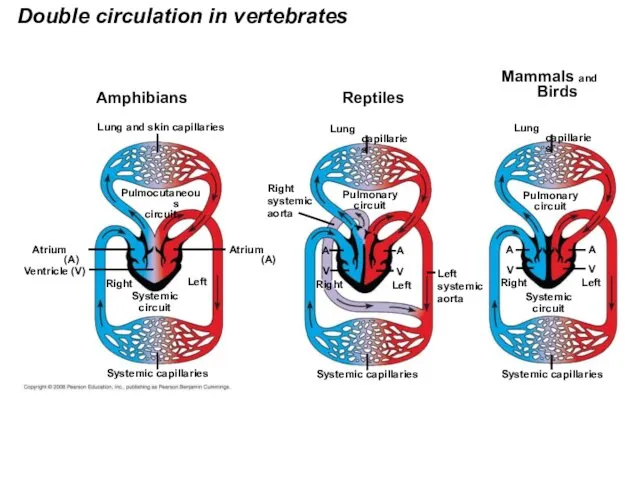
- 18. Double circulation in vertebrates Amphibians Lung and skin capillaries Pulmocutaneous circuit Atrium (A) Ventricle (V) Atrium
- 19. In reptiles and mammals, oxygen-poor blood flows through the pulmonary circuit to pick up oxygen through
- 20. Adaptations of Double Circulatory Systems Amphibians: Frogs / amphibians have a three-chambered heart: 2 atria and
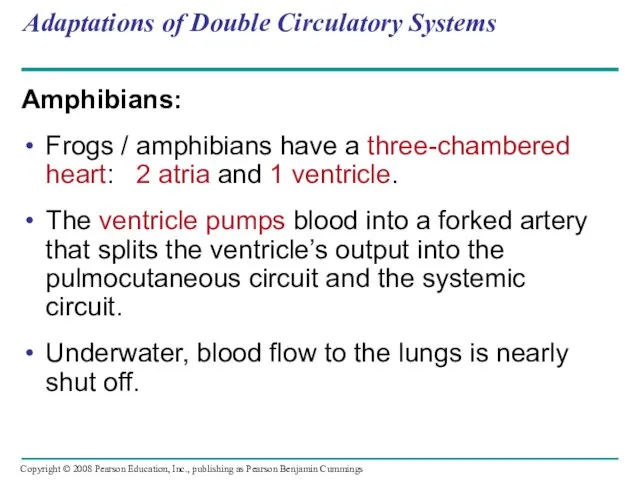
- 21. Reptiles (Except Birds) Turtles, snakes, and lizards have a three-chambered heart: two atria and one ventricle.
- 22. Mammals Mammals and birds have a four-chambered heart with two atria and two ventricles. The left
- 23. Coordinated cycles of heart contraction drive double circulation in mammals Blood begins its flow with the
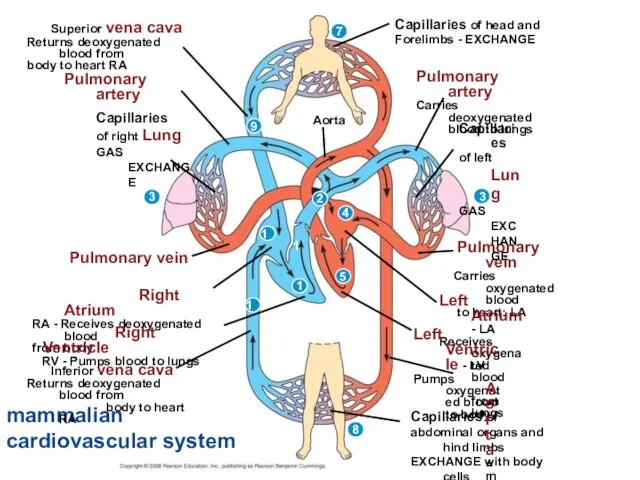
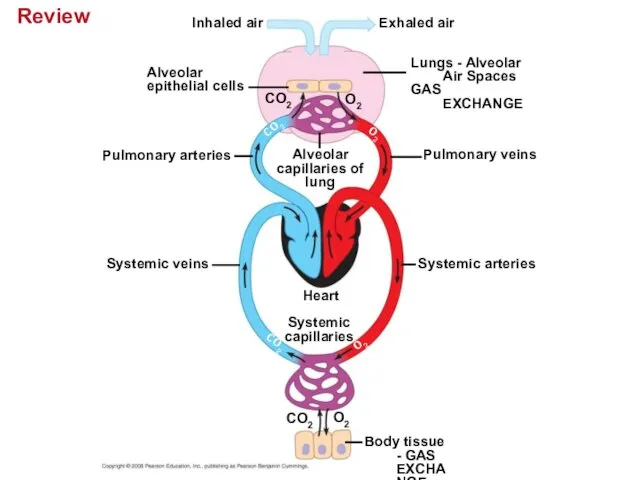
- 24. Blood returns to the heart through the superior vena cava (deoxygenated blood from head, neck, and
- 25. mammalian cardiovascular system Superior vena cava Returns deoxygenated blood from body to heart RA Pulmonary artery
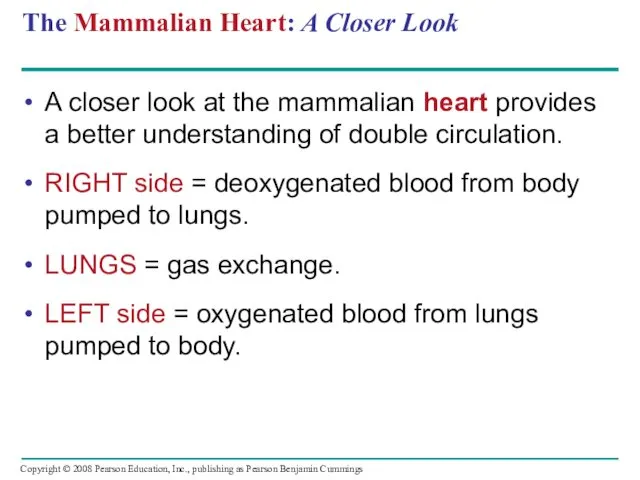
- 26. The Mammalian Heart: A Closer Look A closer look at the mammalian heart provides a better
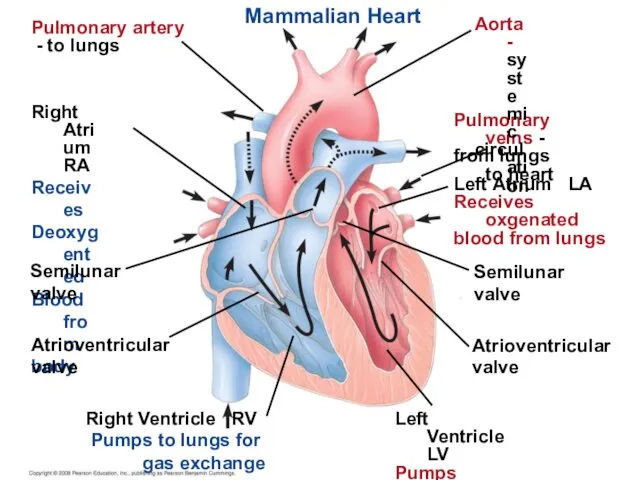
- 27. Mammalian Heart Pulmonary artery - to lungs Right Atrium RA Receives Deoxygented Blood from body Semilunar
- 28. The heart contracts and relaxes in a rhythmic cycle called the cardiac cycle. The contraction, or
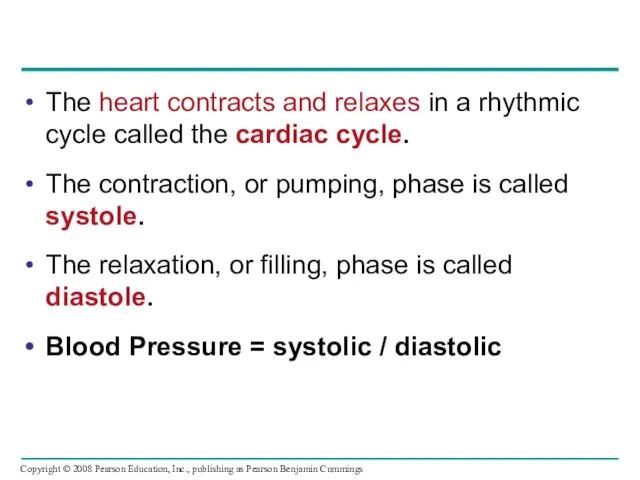
- 29. Cardiac cycle Semilunar valves closed 0.4 sec AV valves open Atrial and ventricular diastole 1 2
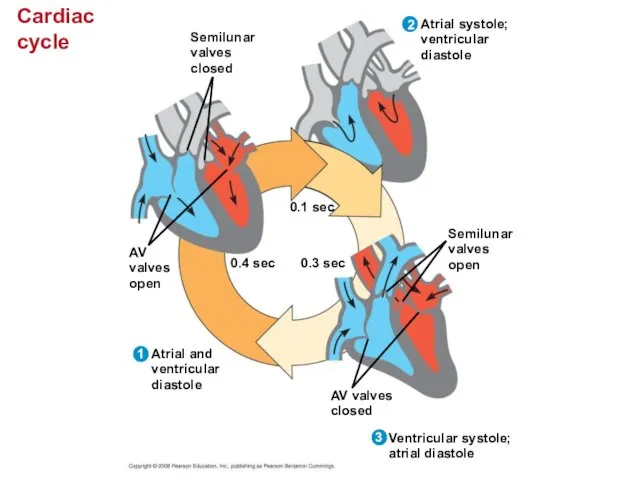
- 30. The heart rate, also called the pulse, is the number of beats per minute. The stroke
- 31. Four valves prevent backflow of blood in the heart: The atrioventricular (AV) valves separate each atrium
- 32. Maintaining the Heart’s Rhythmic Beat Some cardiac muscle cells are self-excitable = they contract without any
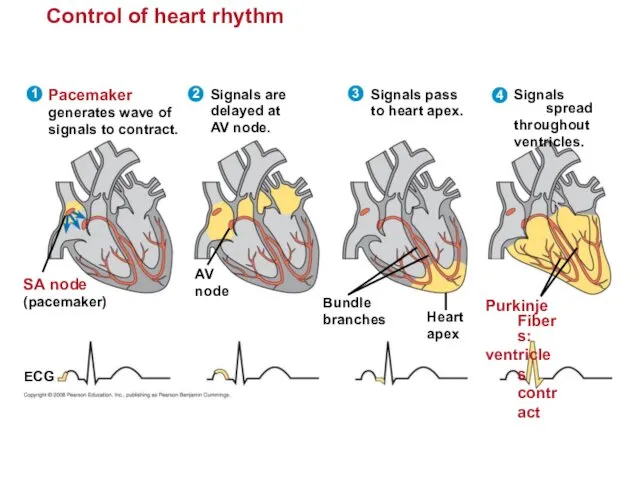
- 33. Control of heart rhythm Signals spread throughout ventricles. 4 Purkinje Fibers: ventricles contract Pacemaker generates wave
- 34. Patterns of blood pressure and flow reflect the structure and arrangement of blood vessels The physical
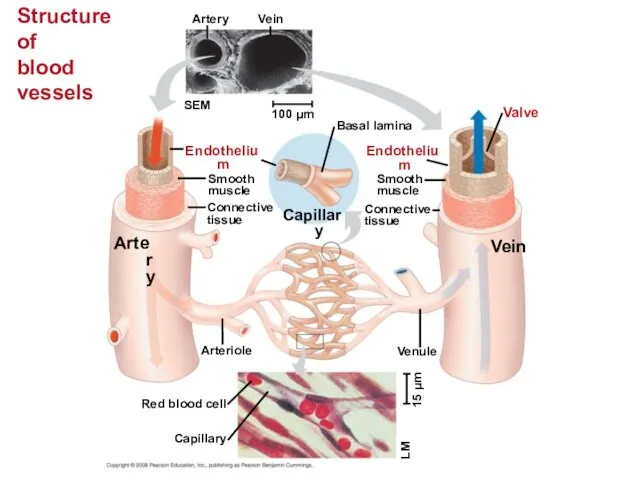
- 35. Structure of blood vessels Artery Vein SEM 100 µm Endothelium Artery Smooth muscle Connective tissue Capillary
- 36. Capillaries have thin walls, the endothelium plus its basement membrane, to facilitate the exchange of materials.
- 37. Blood Flow Velocity Physical laws governing movement of fluids through pipes affect blood flow and blood
- 38. The interrelationship of cross-sectional area of blood vessels, blood flow velocity, and blood pressure. 5,000 4,000
- 39. Blood Pressure Blood pressure is the hydrostatic pressure that blood exerts against the wall of a
- 40. Changes in Blood Pressure During the Cardiac Cycle Systolic pressure is the pressure in the arteries
- 41. Regulation of Blood Pressure Blood pressure is determined by cardiac output and peripheral resistance due to
- 42. Vasoconstriction and vasodilation help maintain adequate blood flow as the body’s demands change. The peptide endothelin
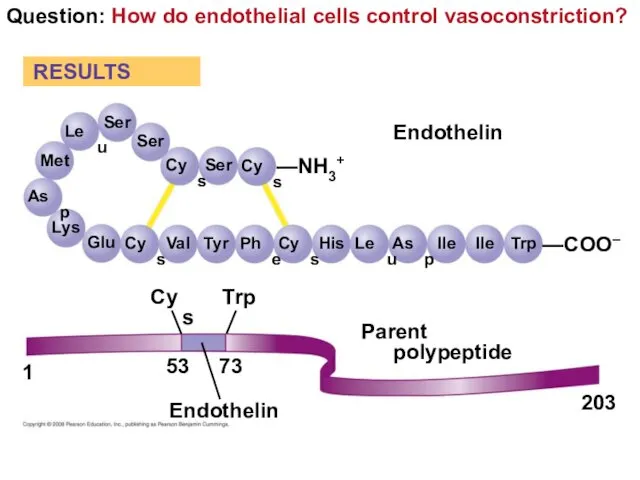
- 43. Question: How do endothelial cells control vasoconstriction? Ser RESULTS Ser Ser Cys Cys —NH3+ Leu Met
- 44. Measurement of blood pressure: sphygmomanometer Pressure in cuff greater than 120 mm Hg Rubber cuff inflated
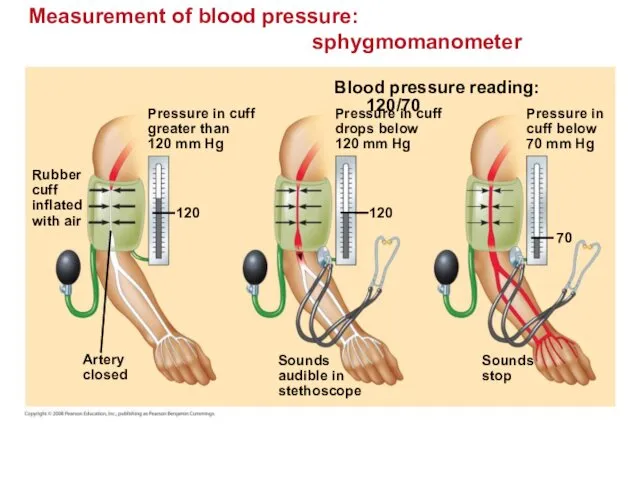
- 45. Fainting is caused by inadequate blood flow to the head. Animals with longer necks require a
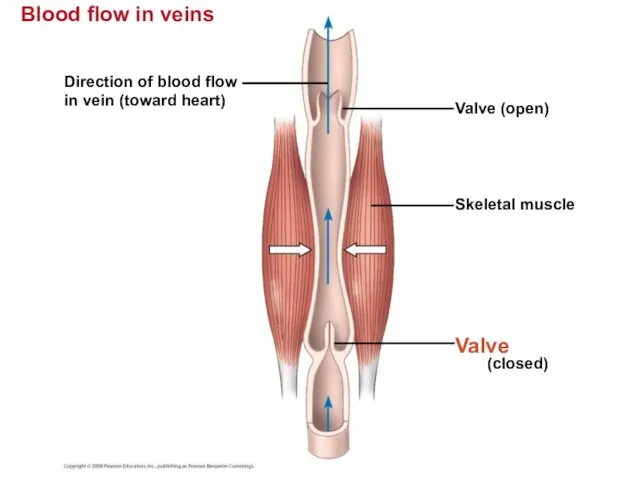
- 46. Blood flow in veins Blood flow in veins Direction of blood flow in vein (toward heart)
- 47. Capillary Function Capillaries in major organs are usually filled to capacity. Blood supply varies in many
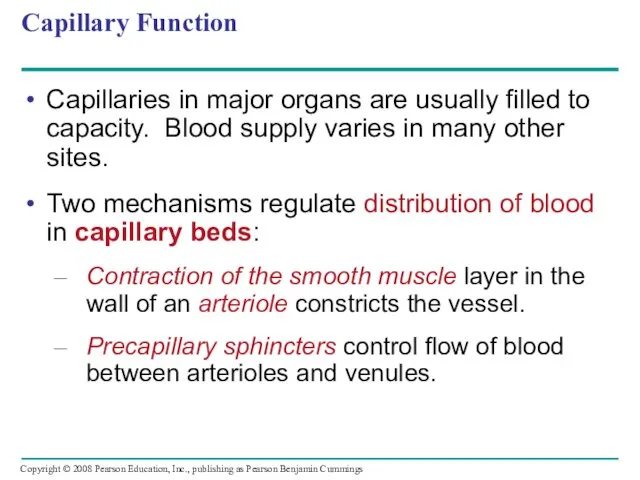
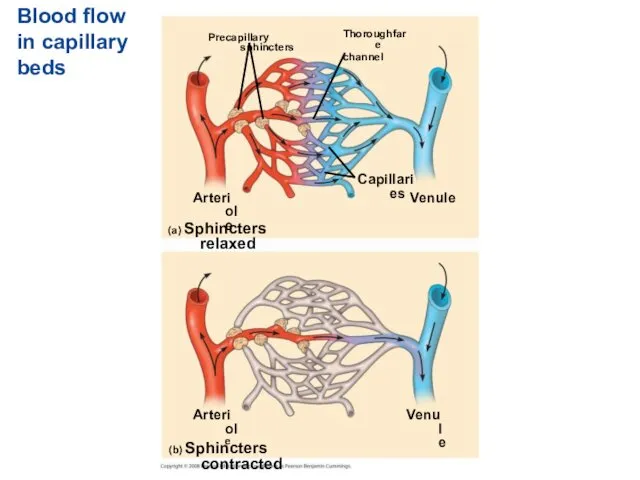
- 48. Blood flow in capillary beds Precapillary sphincters Thoroughfare channel Arteriole Capillaries Venule (a) Sphincters relaxed (b)
- 49. The critical exchange of substances between the blood and interstitial fluid takes place across the thin
- 50. Fluid exchange between capillaries and the interstitial fluid Body tissue Capillary INTERSTITIAL FLUID Net fluid movement
- 51. Fluid Return by the Lymphatic System The lymphatic system - returns fluid that leaks out in
- 52. Lymph nodes are organs that produce phagocytic white blood cells and filter lymph - an important
- 53. Blood Composition and Function Blood consists of several kinds of blood cells suspended in a liquid
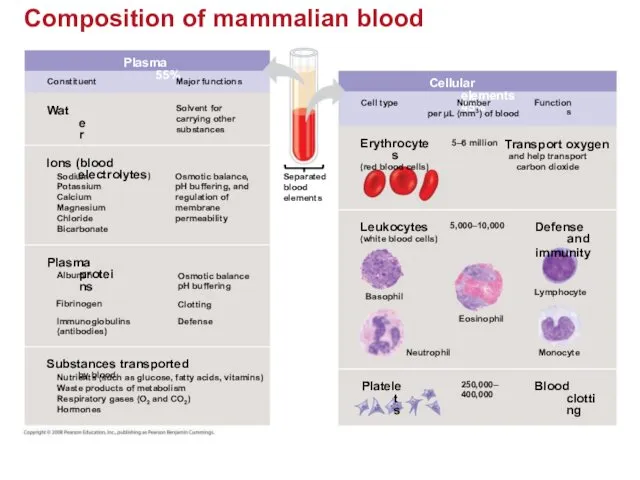
- 54. Composition of mammalian blood Plasma 55% Constituent Major functions Water Solvent for carrying other substances Ions
- 55. Plasma Blood plasma is about 90% water. Among its solutes are inorganic salts in the form
- 56. Cellular Elements Suspended in blood plasma are two types of cells: Red blood cells rbc =
- 57. Red blood cells, or erythrocytes, are by far the most numerous blood cells. They transport oxygen
- 58. Leukocytes - Defense There are five major types of white blood cells, or leukocytes: monocytes, neutrophils,
- 59. Platelets - Blood Clotting Platelets are fragments of cells and function in blood clotting. When the
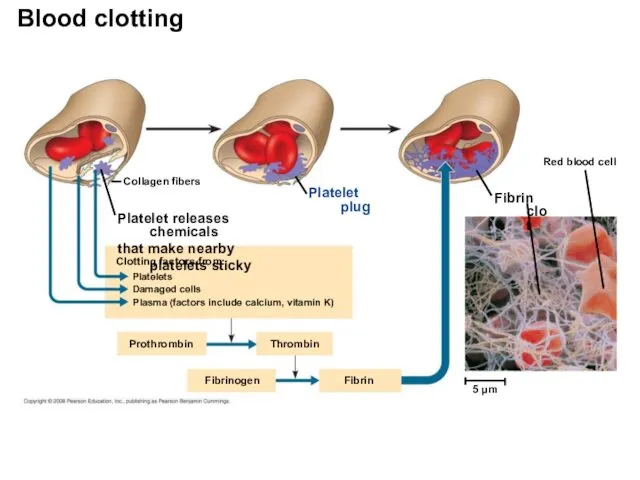
- 60. Collagen fibers Platelet plug Platelet releases chemicals that make nearby platelets sticky Clotting factors from: Platelets
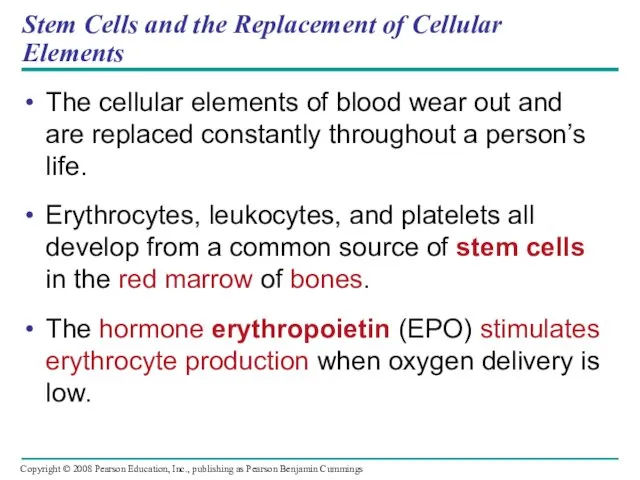
- 61. Stem Cells and the Replacement of Cellular Elements The cellular elements of blood wear out and
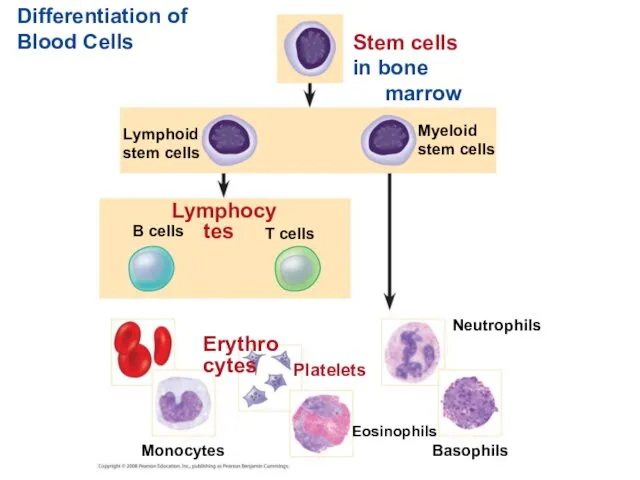
- 62. Differentiation of Blood Cells Stem cells in bone marrow Myeloid stem cells Lymphoid stem cells Lymphocytes
- 63. Cardiovascular Disease = Disorders of the Heart and the Blood Vessels One type of cardiovascular disease,
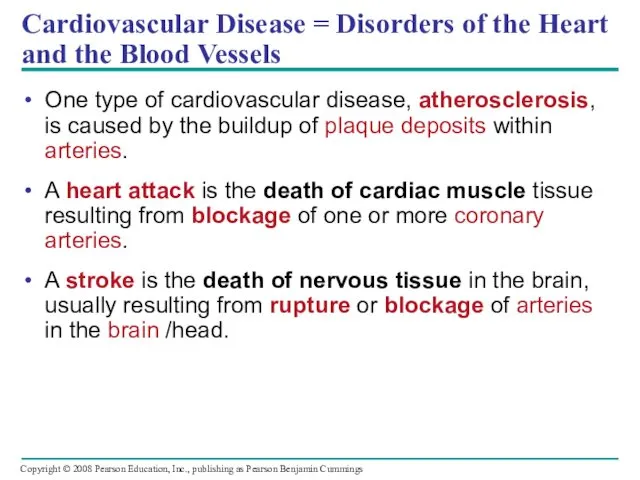
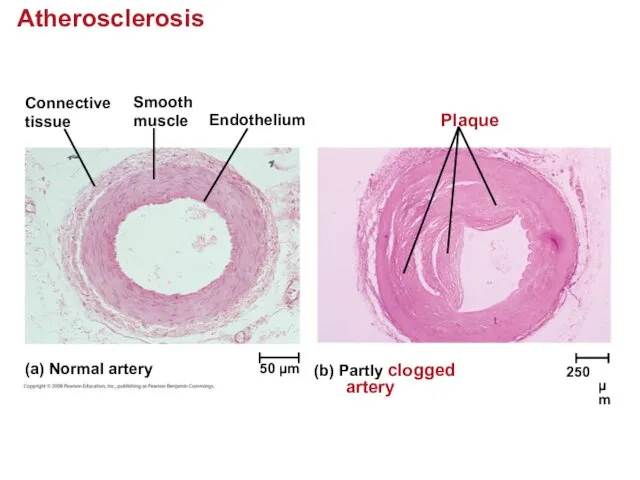
- 64. Atherosclerosis Connective tissue Smooth muscle Endothelium Plaque (a) Normal artery (b) Partly clogged artery 50 µm
- 65. Treatment and Diagnosis of Cardiovascular Disease Cholesterol is a major contributor to atherosclerosis. Low-density lipoproteins (LDLs)
- 66. Gas exchange occurs across specialized respiratory surfaces Gas exchange supplies oxygen for cellular respiration and disposes
- 67. Respiratory Media Animals can use air or water as a source of O2, or respiratory medium.
- 68. Respiratory Surfaces Animals require large, moist respiratory surfaces for exchange of gases between their cells and
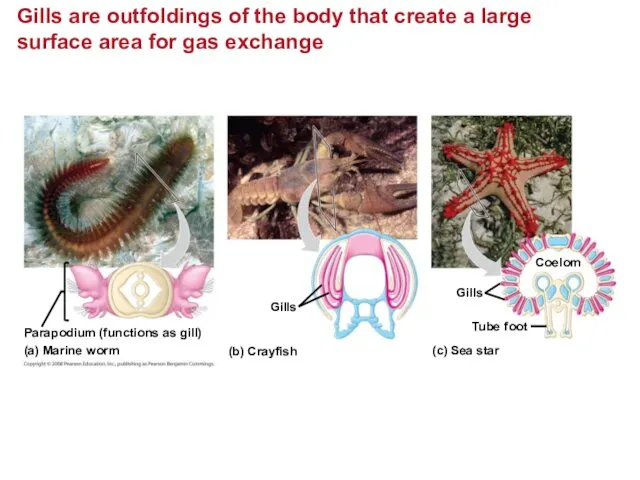
- 69. Gills are outfoldings of the body that create a large surface area for gas exchange Parapodium
- 70. Ventilation moves the respiratory medium over the respiratory surface. Aquatic animals move through water or move
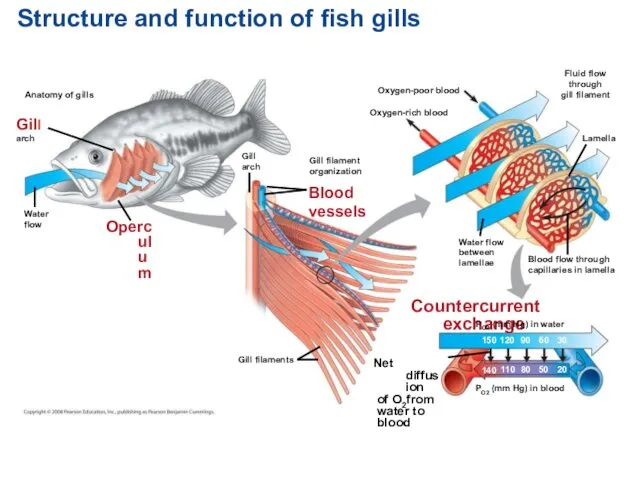
- 71. Structure and function of fish gills Anatomy of gills Gill arch Water flow Operculum Gill arch
- 72. Tracheal Systems in Insects The tracheal system of insects consists of tiny branching tubes that penetrate
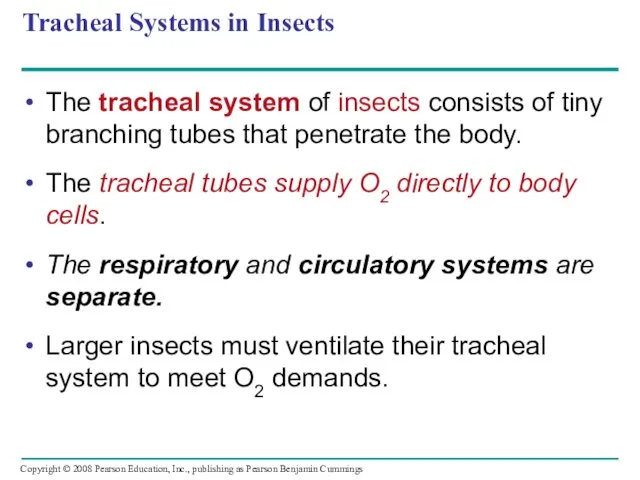
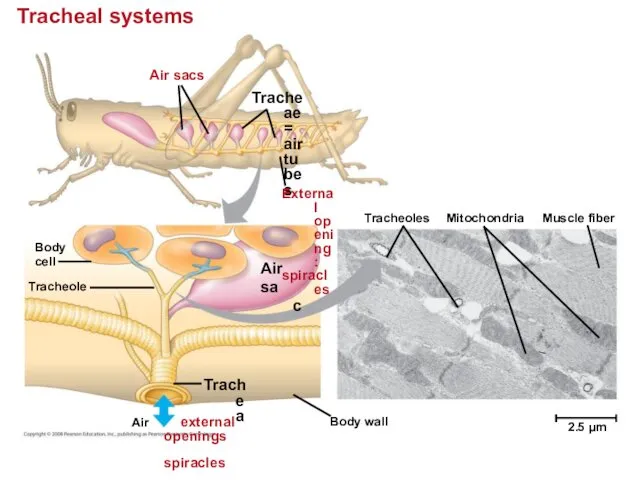
- 73. Tracheal systems Air sacs Tracheae = air tubes External opening: spiracles Body cell Air sac Tracheole
- 74. Lungs = Infoldings of the body surface The circulatory system (open or closed) transports gases between
- 75. Mammalian Respiratory Systems: A Closer Look A system of branching ducts / air tubes conveys air
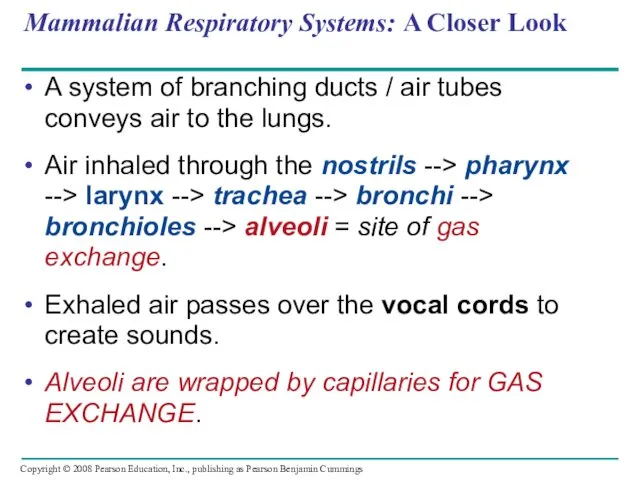
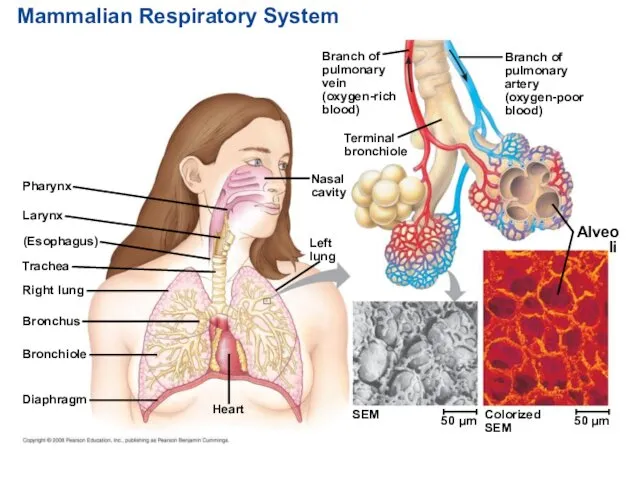
- 76. Mammalian Respiratory System Pharynx Larynx (Esophagus) Trachea Right lung Bronchus Bronchiole Diaphragm Heart SEM Left lung
- 77. Breathing Ventilates the Lungs by Inhalation and Exhalation of Air Amphibians, such as a frog, ventilates
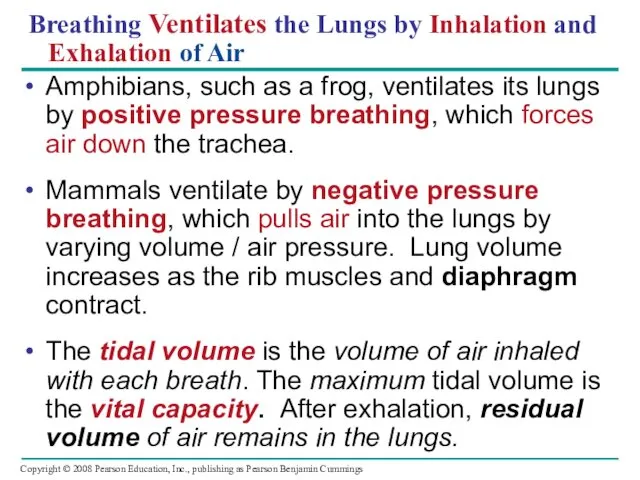
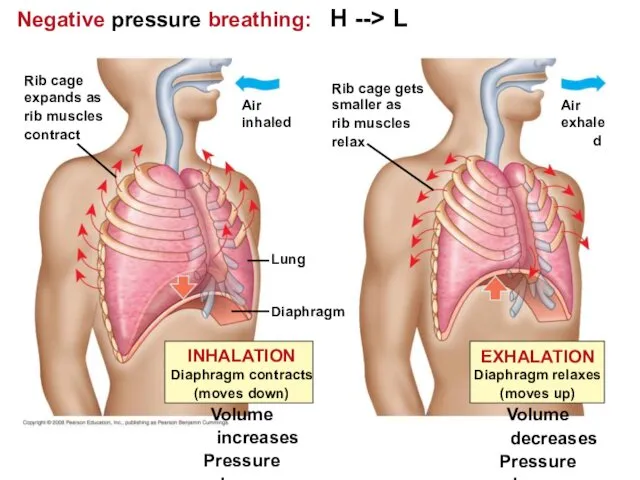
- 78. Negative pressure breathing: H --> L Lung Diaphragm Air inhaled Rib cage expands as rib muscles
- 79. How a Bird Breathes Birds have eight or nine air sacs that function as bellows that
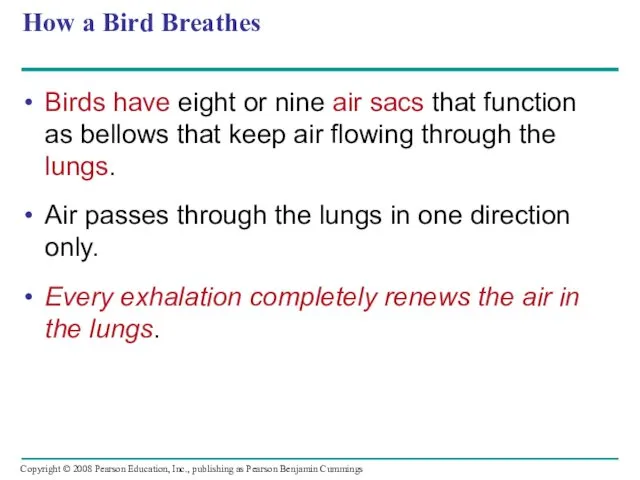
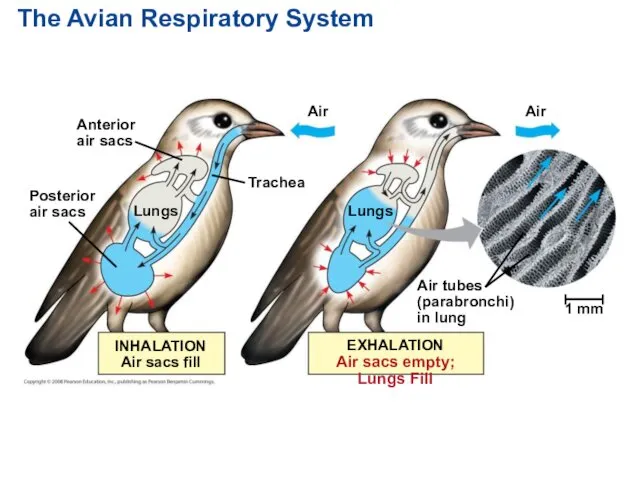
- 80. The Avian Respiratory System Anterior air sacs Posterior air sacs Lungs Air Lungs Air 1 mm
- 81. Control of Breathing in Humans In humans, the main breathing control centers are in two regions
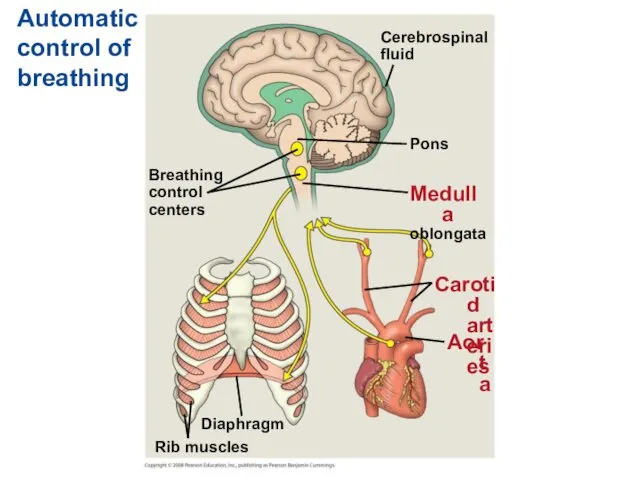
- 82. Sensors in the aorta and carotid arteries monitor O2 and CO2 concentrations in the blood. These
- 83. Automatic control of breathing Breathing control centers Cerebrospinal fluid Pons Medulla oblongata Carotid arteries Aorta Diaphragm
- 84. Adaptations for gas exchange include pigments that bind and transport gases The metabolic demands of many
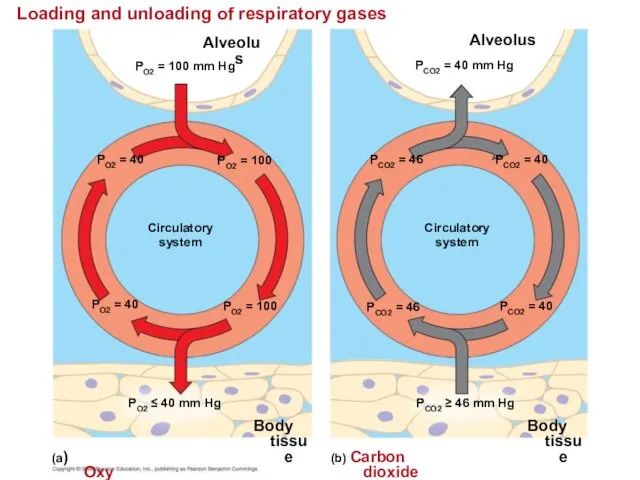
- 85. Loading and unloading of respiratory gases Alveolus PO2 = 100 mm Hg PO2 = 40 PO2
- 86. Respiratory Pigments Respiratory pigments = proteins that transport oxygen, greatly increase the amount of oxygen that
- 87. Hemoglobin A single hemoglobin molecule can carry four molecules of O2 The hemoglobin dissociation curve shows
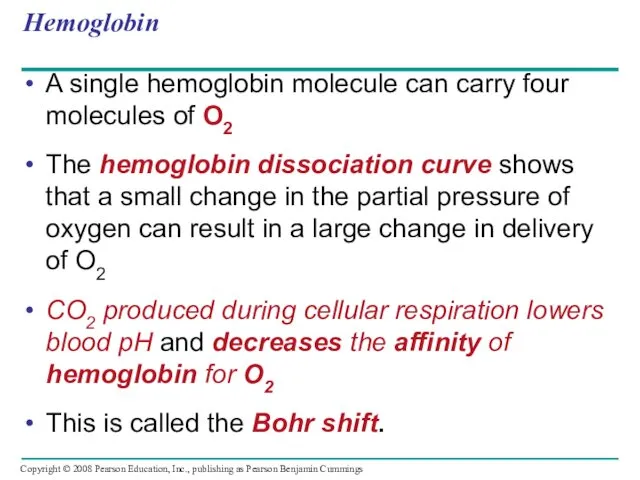
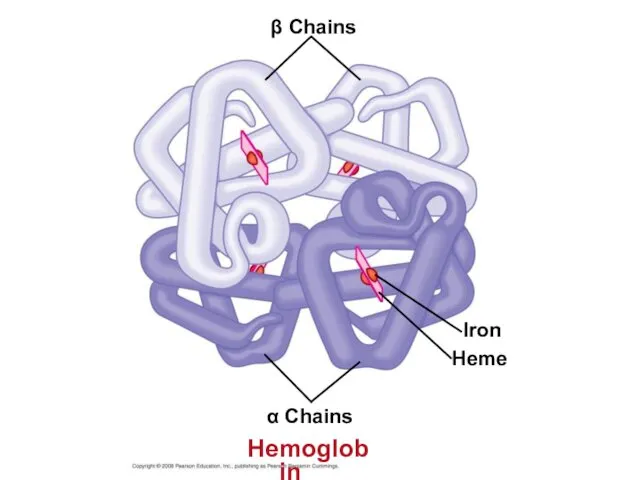
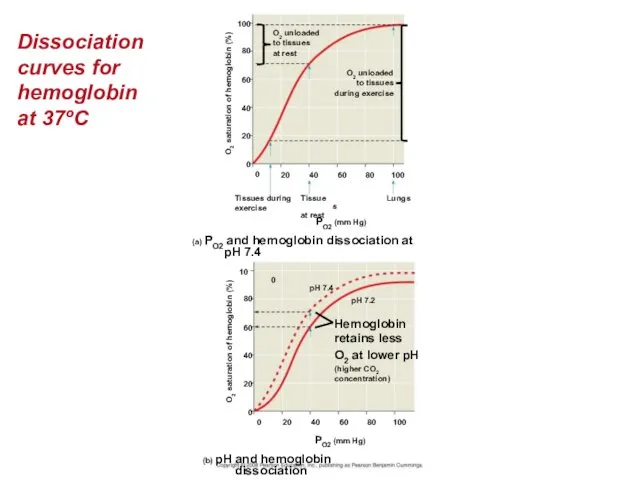
- 88. β Chains Iron Heme α Chains Hemoglobin
- 89. Dissociation curves for hemoglobin at 37ºC O2 unloaded to tissues at rest O2 unloaded to tissues
- 90. Carbon Dioxide Transport Hemoglobin also helps transport CO2 and assists in buffering. CO2 from respiring cells
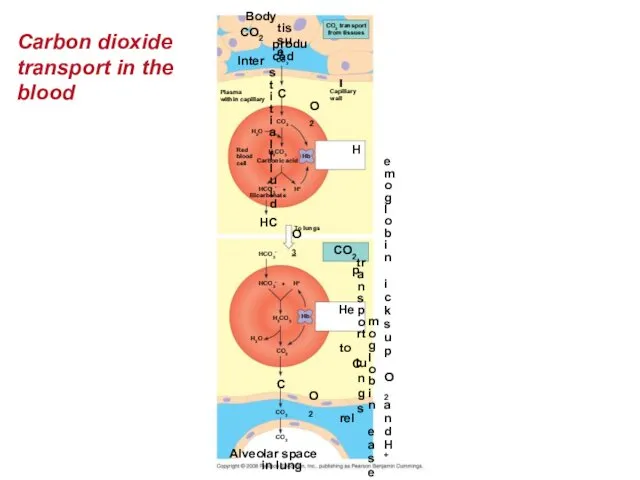
- 91. Carbon dioxide transport in the blood Body tissue CO2 produced CO2 transport from tissues Capillary wall
- 92. Elite Animal Athletes Migratory and diving mammals have evolutionary adaptations that allow them to perform extraordinary
- 93. Review Inhaled air Exhaled air Alveolar epithelial cells Lungs - Alveolar Air Spaces GAS EXCHANGE CO2
- 94. You should now be able to: Compare and contrast open and closed circulatory systems. Compare and
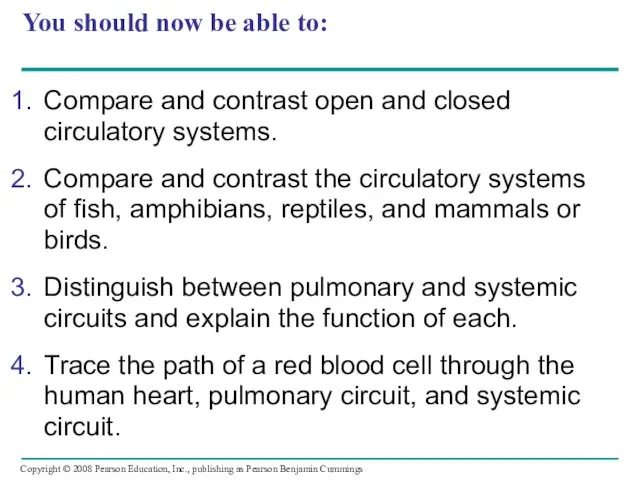
- 95. Define cardiac cycle and explain the role of the sinoatrial node. Relate the structures of capillaries,
- 96. Describe the role played by the lymphatic system in relation to the circulatory system. Describe the
- 98. Скачать презентацию







 Тип Моллюски. Класс Брюхоногие. Класс Двустворчатые. Класс Головоногие
Тип Моллюски. Класс Брюхоногие. Класс Двустворчатые. Класс Головоногие Углерод
Углерод Первичные продуценты, в основе новообразования органического вещества которых лежит хемосинтез
Первичные продуценты, в основе новообразования органического вещества которых лежит хемосинтез Лишайники – симбиотические организмы
Лишайники – симбиотические организмы Ферменттің қасиеті мен құрылысы
Ферменттің қасиеті мен құрылысы Покормите птиц зимой. (5 класс)
Покормите птиц зимой. (5 класс) Популяция. Типы экологических взаимодействий
Популяция. Типы экологических взаимодействий Митоз и мейоз
Митоз и мейоз Как стать городским фермером. Вертикальные фермы
Как стать городским фермером. Вертикальные фермы Хрящевые рыбы
Хрящевые рыбы Запилення квіткових рослин
Запилення квіткових рослин Ритмы мозга
Ритмы мозга Характеристика костной системы
Характеристика костной системы Эндокринная система человека
Эндокринная система человека Энзимопатия. Энзимотерапия. Энзимодиагностика
Энзимопатия. Энзимотерапия. Энзимодиагностика Почему дети похожи на родителей
Почему дети похожи на родителей Анатомо-физиологические особенности человека в подростковом возрасте
Анатомо-физиологические особенности человека в подростковом возрасте Жизнедеятельность клетки
Жизнедеятельность клетки Овощи
Овощи Экология микроорганизмов
Экология микроорганизмов Пищеварение в желудке и кишечнике
Пищеварение в желудке и кишечнике Деревья и кустарники
Деревья и кустарники Строение и функции кожи
Строение и функции кожи Актиномицеты (actinomycetes)
Актиномицеты (actinomycetes) Кожные покровы хордовых
Кожные покровы хордовых Презентация к уроку биологии в 7 классе Особенности организации одноклеточных, их классификация
Презентация к уроку биологии в 7 классе Особенности организации одноклеточных, их классификация растения
растения Интересные факты о коже. Презентация.
Интересные факты о коже. Презентация.