Содержание
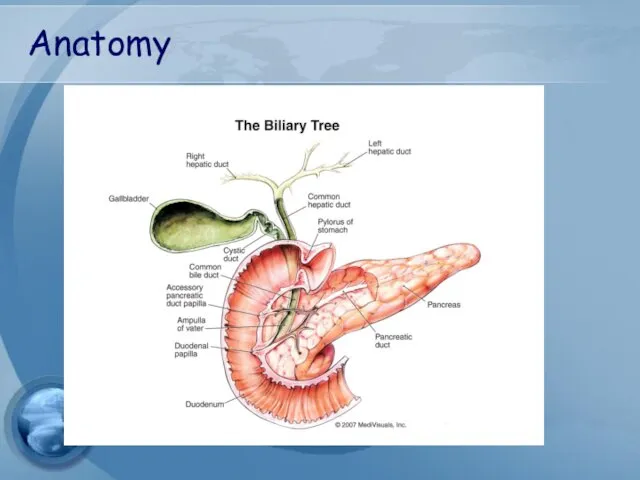
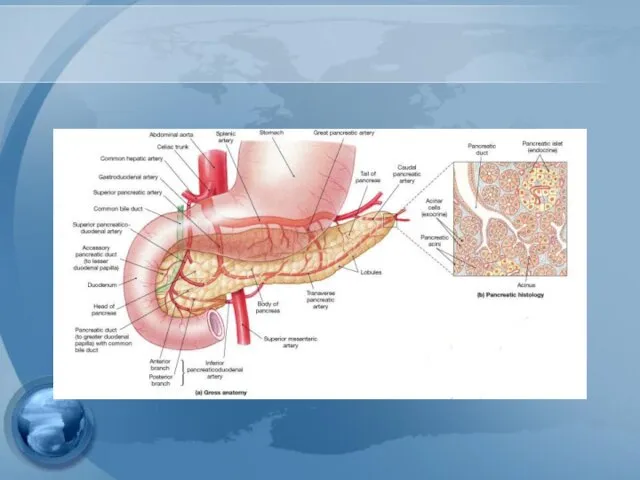
- 2. Anatomy
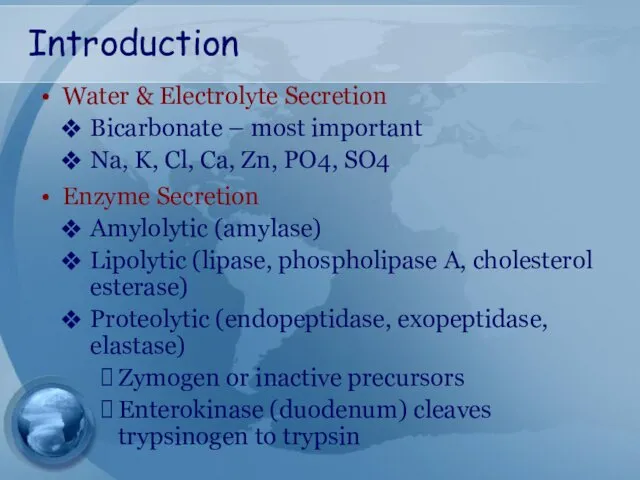
- 4. Introduction Water & Electrolyte Secretion Bicarbonate – most important Na, K, Cl, Ca, Zn, PO4, SO4
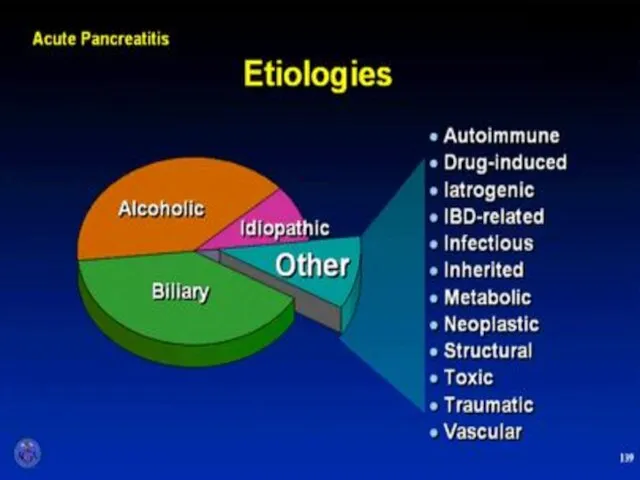
- 5. What are the two most common etiologies for acute pancreatitis in the western civilization? Drugs and
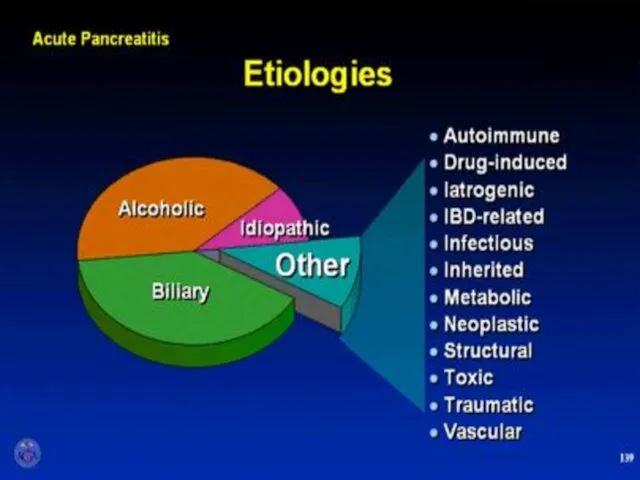
- 6. Etiology
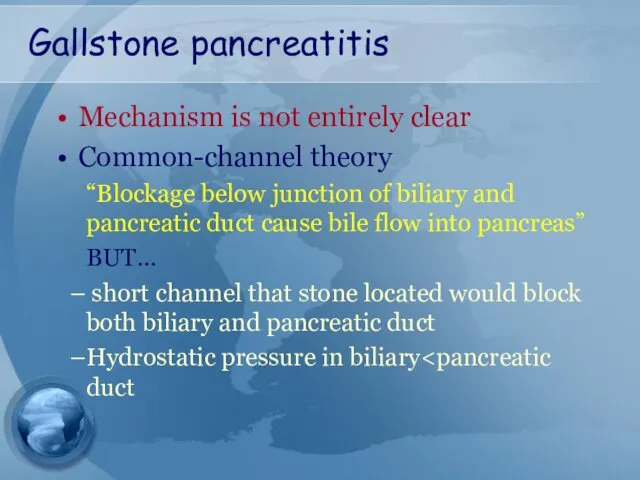
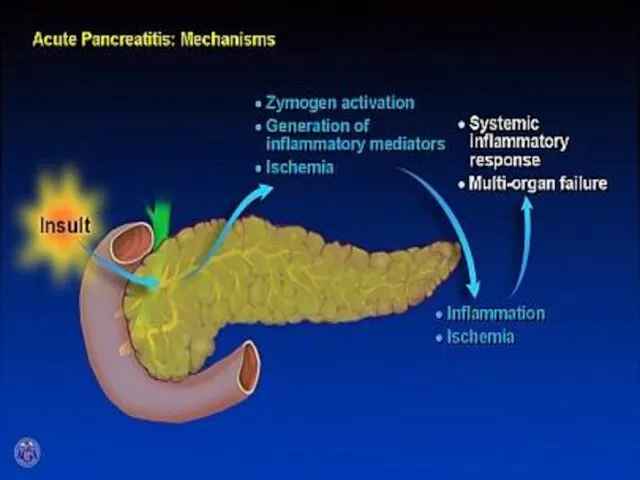
- 8. Gallstone pancreatitis Mechanism is not entirely clear Common-channel theory “Blockage below junction of biliary and pancreatic
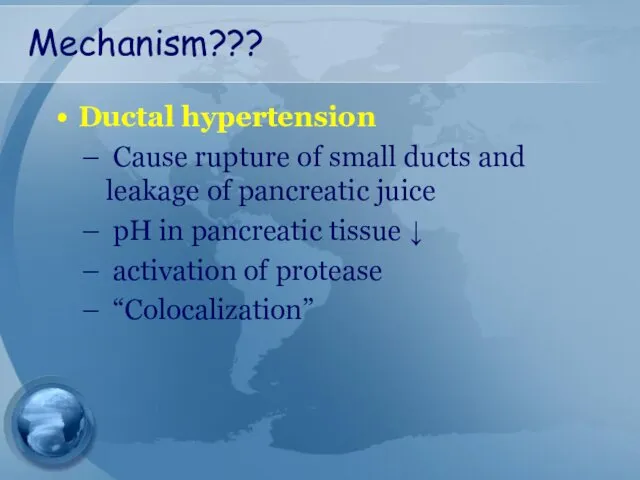
- 9. Mechanism??? Ductal hypertension Cause rupture of small ducts and leakage of pancreatic juice pH in pancreatic
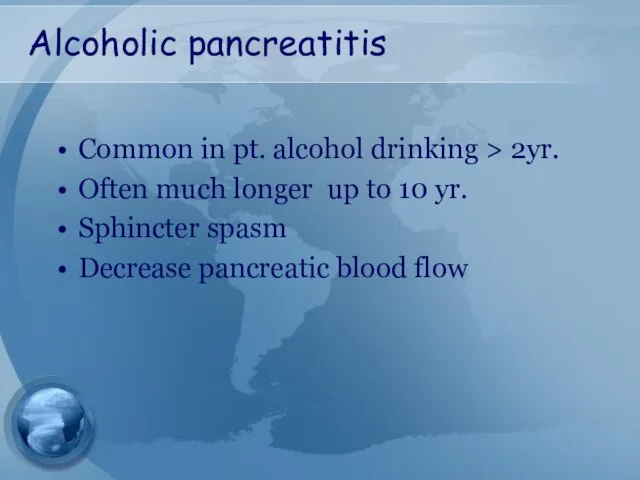
- 10. Alcoholic pancreatitis Common in pt. alcohol drinking > 2yr. Often much longer up to 10 yr.
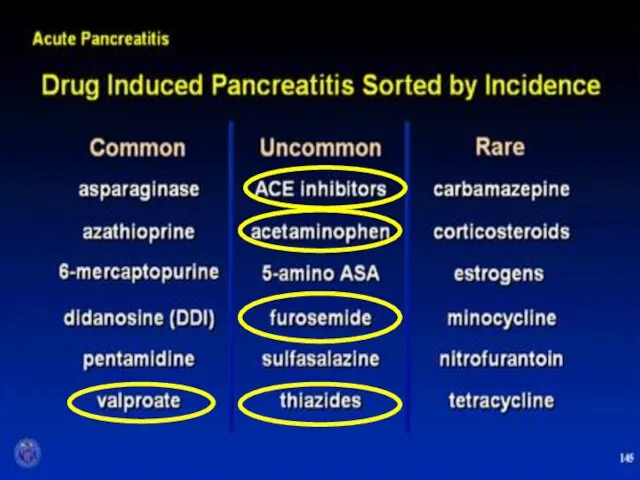
- 12. Which of the following drugs is well known for it’s ability to induce pancreatitis? Propranolol Erythromycin
- 14. AGA Institute
- 15. Diagnosis
- 16. Diagnostic criteria Two of following three features Upper abd. pain of acute onset often radiating to
- 17. Physical exam Grey Turner’s Sign - ecchymosis in 1 or both flanks Cullen’s sign - ecchymosis
- 18. Grey Turner’s Sign
- 19. Cullen’s Sign
- 20. Serum markers
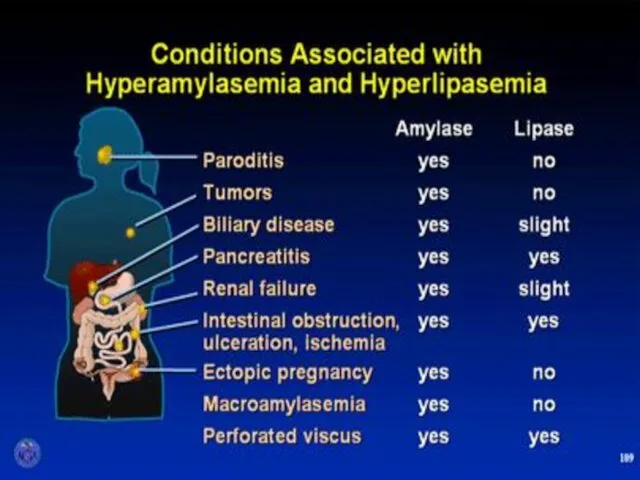
- 21. Serum amylase Elevates within HOURS and can remain elevated for 3-5 days High specificity when level
- 22. Urine amylase urinary levels may be more sensitive than serum levels. Urinary amylase levels usually remain
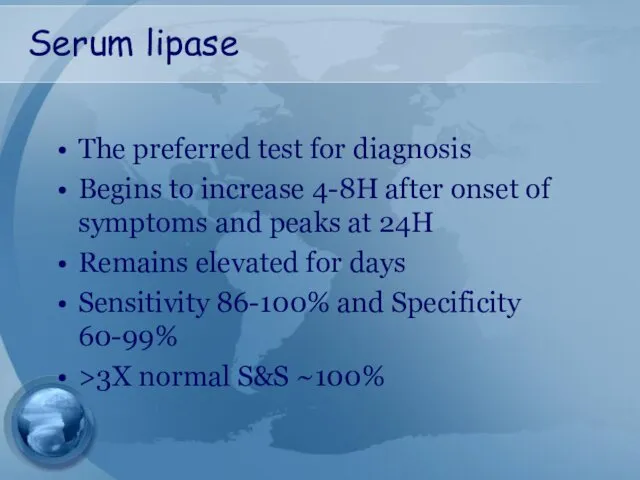
- 23. Serum lipase The preferred test for diagnosis Begins to increase 4-8H after onset of symptoms and
- 25. Plain Abdominal Radiograph
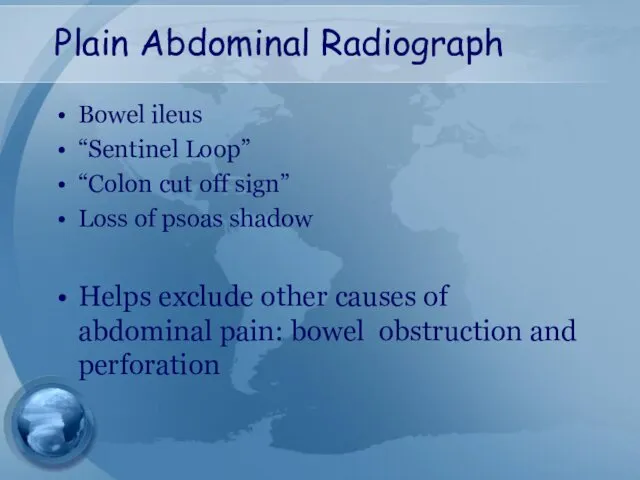
- 26. Plain Abdominal Radiograph Bowel ileus “Sentinel Loop” “Colon cut off sign” Loss of psoas shadow Helps
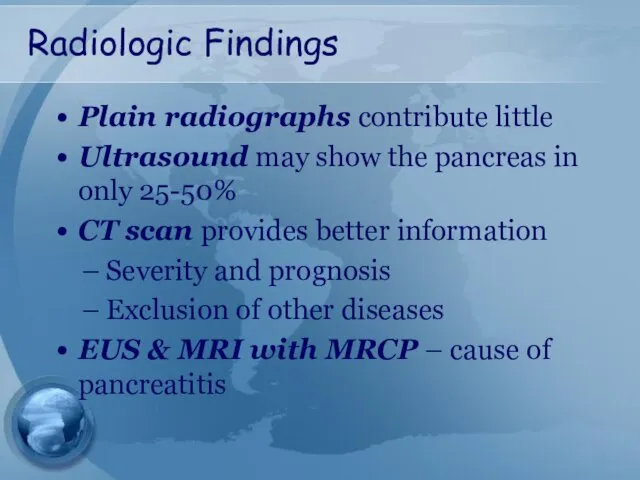
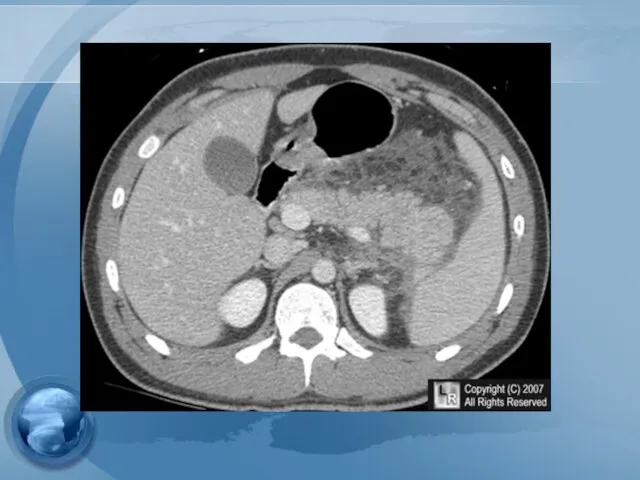
- 27. Radiologic Findings Plain radiographs contribute little Ultrasound may show the pancreas in only 25-50% CT scan
- 28. Assessment of severity
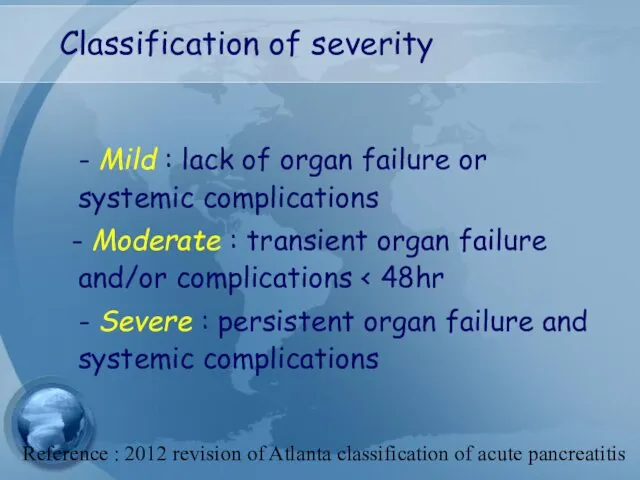
- 29. Classification of severity - Mild : lack of organ failure or systemic complications - Moderate :
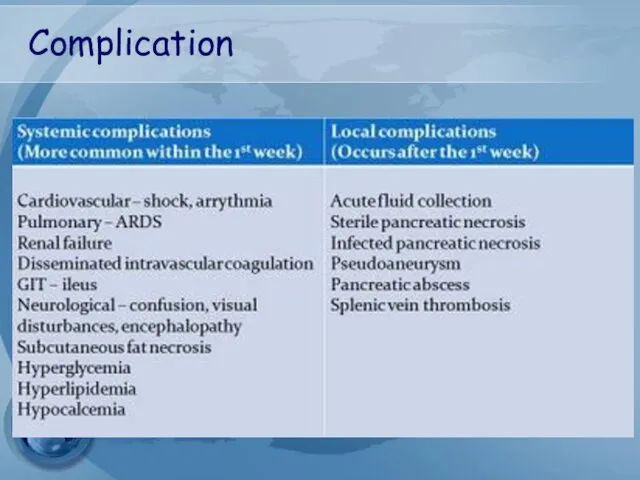
- 30. Complication
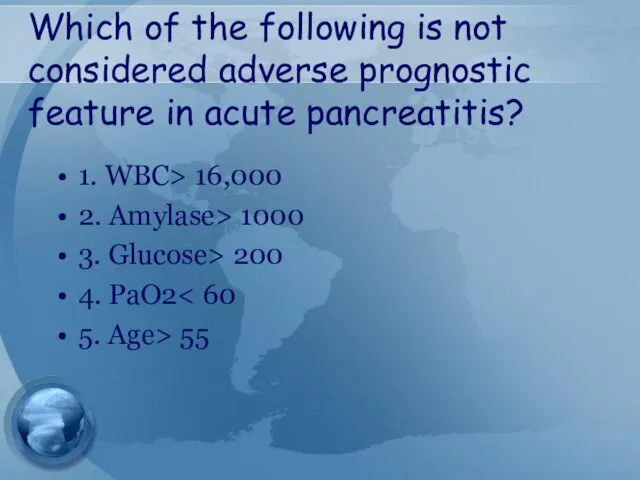
- 31. Which of the following is not considered adverse prognostic feature in acute pancreatitis? 1. WBC> 16,000
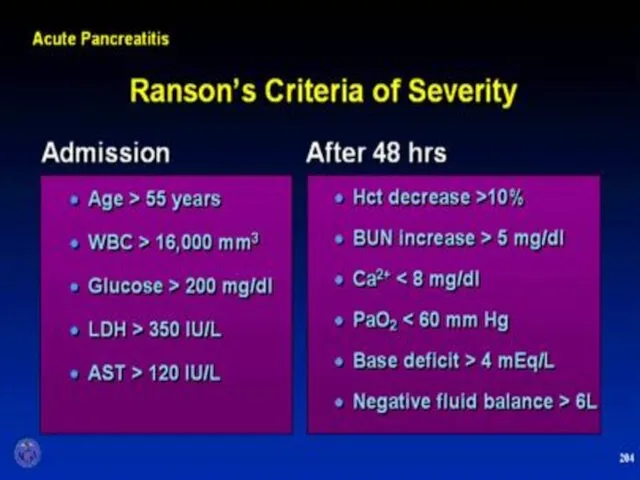
- 32. Early prognostic signs Ranson’s score APACHE II
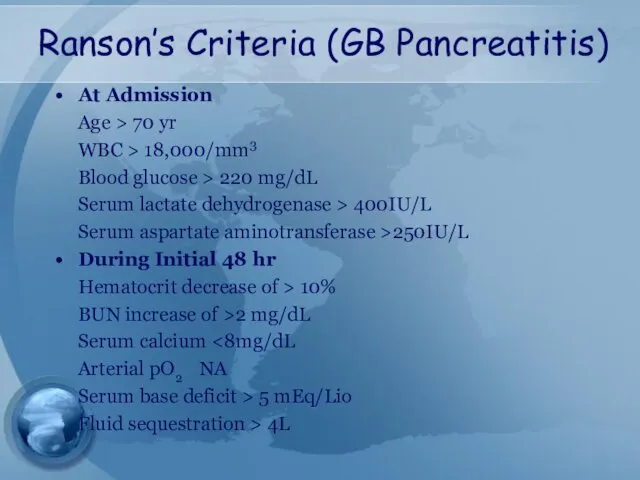
- 34. Ranson’s Criteria (GB Pancreatitis) At Admission Age > 70 yr WBC > 18,000/mm3 Blood glucose >
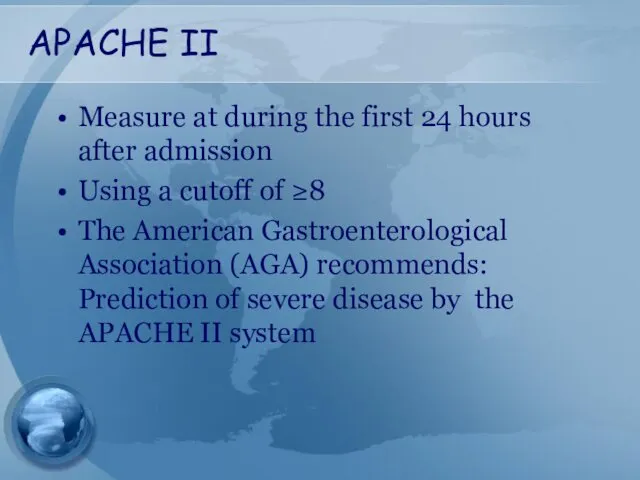
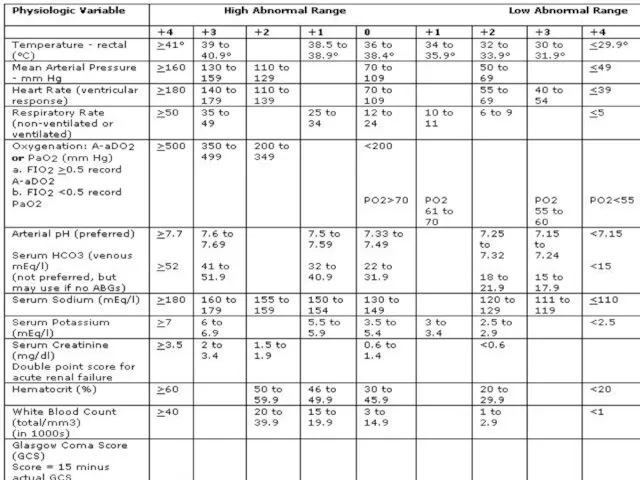
- 35. APACHE II Measure at during the first 24 hours after admission Using a cutoff of ≥8
- 36. APACHE II
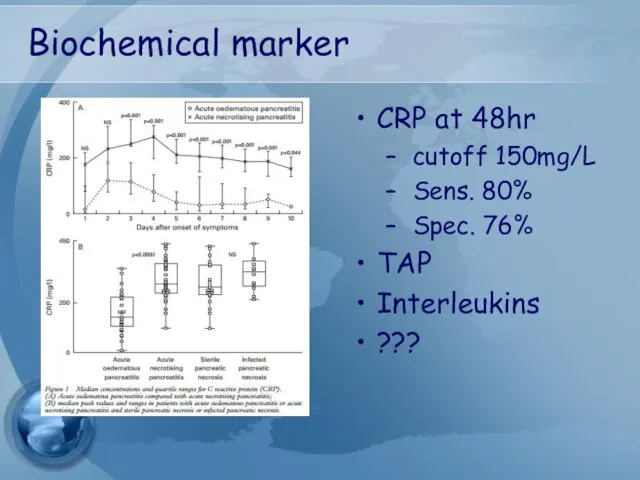
- 37. Biochemical marker CRP at 48hr cutoff 150mg/L Sens. 80% Spec. 76% TAP Interleukins ???
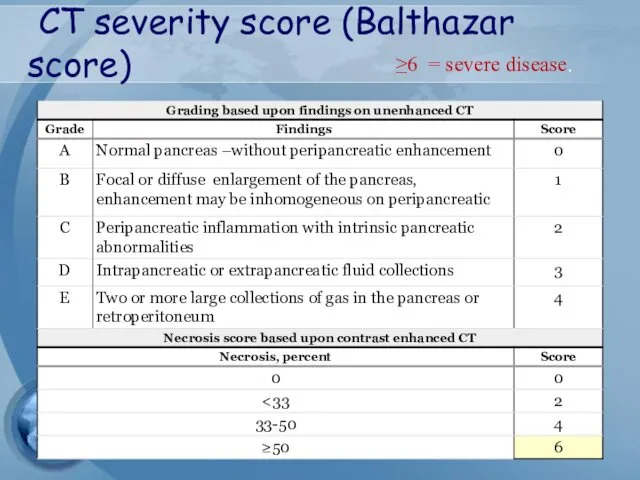
- 38. CT severity score (Balthazar score) ≥6 = severe disease.
- 40. Treatment
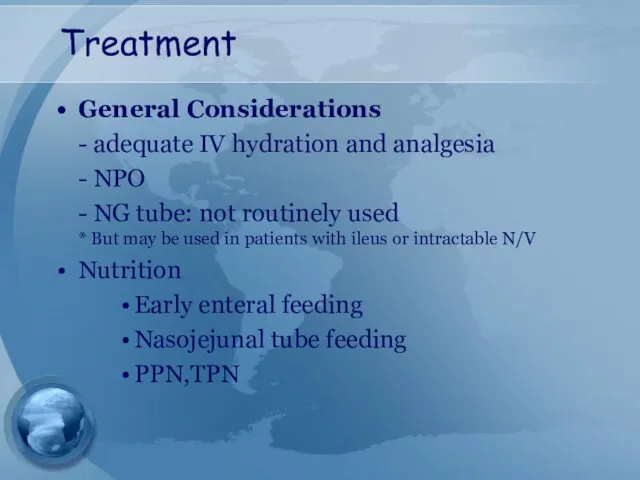
- 41. Treatment General Considerations - adequate IV hydration and analgesia - NPO - NG tube: not routinely
- 42. Treatment Metabolic Complications - Correction of electrolyte imbalance - Ca,Mg - Cautiously for hyperglycemia Cardiovascular Care
- 43. Prophylactic antibiotics Although this is still an area of debate Not indicated for mild attack suggest
- 44. TREATMENT OF ASSOCIATED CONDITIONS Gallstone pancreatitis ERCP should be performed within 72 hours in those with
- 45. Cholecystectomy?? should be performed after recovery in all patient with gallstone pancreatitis Failure to perform a
- 46. Cholecystectomy In mild pancreatitis case, can usually be performed safely within 7 days after recovery In
- 47. Complications
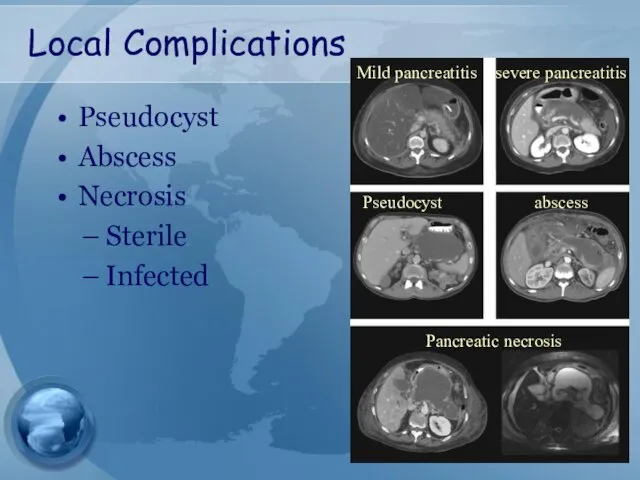
- 48. Local Complications Pseudocyst Abscess Necrosis Sterile Infected Mild pancreatitis severe pancreatitis Pseudocyst abscess Pancreatic necrosis
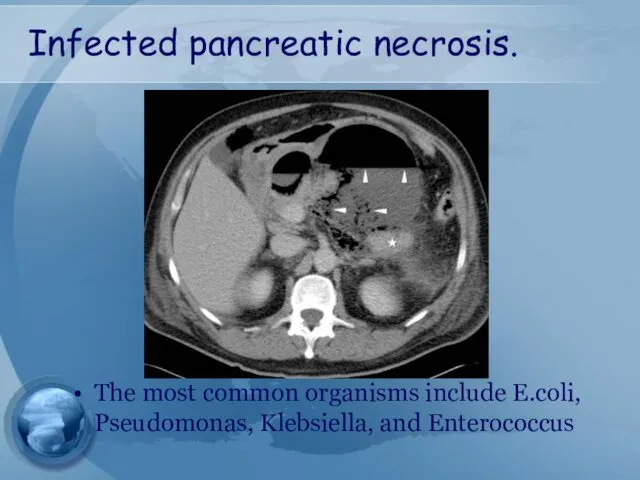
- 49. Infected pancreatic necrosis. The most common organisms include E.coli, Pseudomonas, Klebsiella, and Enterococcus
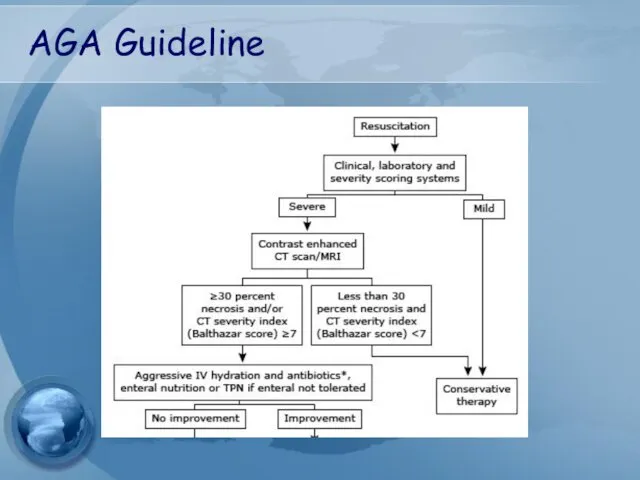
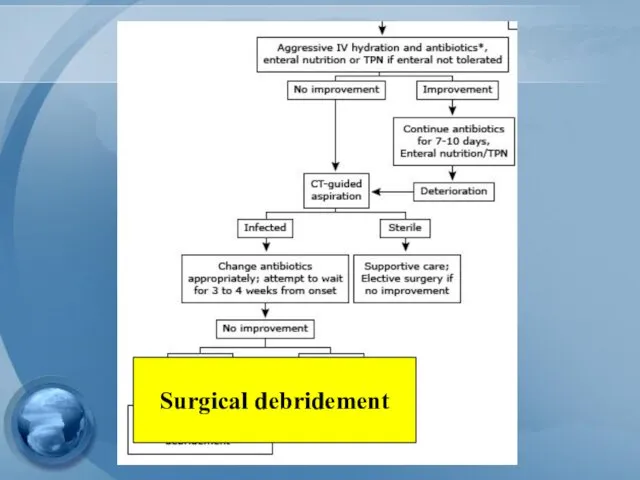
- 50. Guideline management of severe pancreatitis
- 51. AGA Guideline
- 52. Surgical debridement
- 53. Management of pseudocyst
- 54. Management of pseudocyst Watchful waiting: Operative intervention was recommended following an observation period of 6 wks
- 55. Management of pseudocyst Surgical drainage – gold standard Open vs endoscopic cystgastrostomy Cystenterostomy Cystojejunostomy, Cystoduodenostomy Ressection
- 56. Management of pseudocyst Percutaneous catheter drainage As effective as surgery in draining and closing both sterile
- 57. Management of local complication of pancreatitis
- 58. Indication for pancreatic debridement Infected pancreatic necrosis Symptomatic sterile pancreatic necrosis chronic low grade fever Nausea
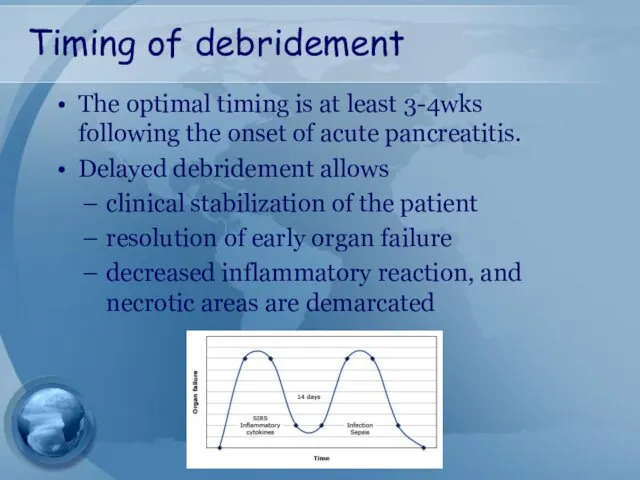
- 59. Timing of debridement The optimal timing is at least 3-4wks following the onset of acute pancreatitis.
- 61. Скачать презентацию










 Общая семиотика экстрапирамидных нарушений
Общая семиотика экстрапирамидных нарушений Лікарські засоби промислового виробництва, що проявляють гепатопротекторну дію
Лікарські засоби промислового виробництва, що проявляють гепатопротекторну дію Гнойные заболевания костей и суставов. (Лекция 26)
Гнойные заболевания костей и суставов. (Лекция 26) Здоровый образ жизни. Медико – профилактическое направление здравоохранения. Виды профилактики
Здоровый образ жизни. Медико – профилактическое направление здравоохранения. Виды профилактики Гинекологиядағы нейроэндокринді синдромдар
Гинекологиядағы нейроэндокринді синдромдар ОМП. Бактериологическое оружие
ОМП. Бактериологическое оружие Болевой синдром
Болевой синдром Федеральный закон Об обращении лекарственные средств. (Лекции 7,8)
Федеральный закон Об обращении лекарственные средств. (Лекции 7,8) Протезирование дефектов зубных рядов пластмассовыми комбинированными и цельнокерамическими коронками
Протезирование дефектов зубных рядов пластмассовыми комбинированными и цельнокерамическими коронками Воспаление. Флогогены
Воспаление. Флогогены Braster pro-иновационная система обследования молочной железы
Braster pro-иновационная система обследования молочной железы Клиническая анатомия головы. Хирургическая анатомия мозгового отдела головы
Клиническая анатомия головы. Хирургическая анатомия мозгового отдела головы Пищевые отравления и их профилактика
Пищевые отравления и их профилактика Легочная гипертензия
Легочная гипертензия Роль питания в профилактике и лечении рака. Клиника иммунопатологии Мира
Роль питания в профилактике и лечении рака. Клиника иммунопатологии Мира Анатомо-фізіологічні особливості шлунково-кишкового тракту. Методика обстеження ШКТ. (Лекція 4)
Анатомо-фізіологічні особливості шлунково-кишкового тракту. Методика обстеження ШКТ. (Лекція 4) Ларинготрахеит у детей
Ларинготрахеит у детей Биоптрон 2014
Биоптрон 2014 Рациональная антибиотикотерапия при бактериальных осложнениях ОРВИ
Рациональная антибиотикотерапия при бактериальных осложнениях ОРВИ Санитарная микробиология
Санитарная микробиология Этика в психиатрии и психотерапии
Этика в психиатрии и психотерапии Концепция здоровья Coral Club
Концепция здоровья Coral Club Гранулематоз Вегенера
Гранулематоз Вегенера Острые гастродуоденальные кровотечения. Принципы диагностики и лечения
Острые гастродуоденальные кровотечения. Принципы диагностики и лечения Аневризма сердца
Аневризма сердца Іріңді-септикалық асқынулар кезіндегі интенсивті терапия
Іріңді-септикалық асқынулар кезіндегі интенсивті терапия Туберкульоз. Історія боротьби
Туберкульоз. Історія боротьби Организация стоматологического терапевтического кабинета
Организация стоматологического терапевтического кабинета