Содержание
- 2. History A 62 year old male with a prior MI, ejection fraction of 25% and prior
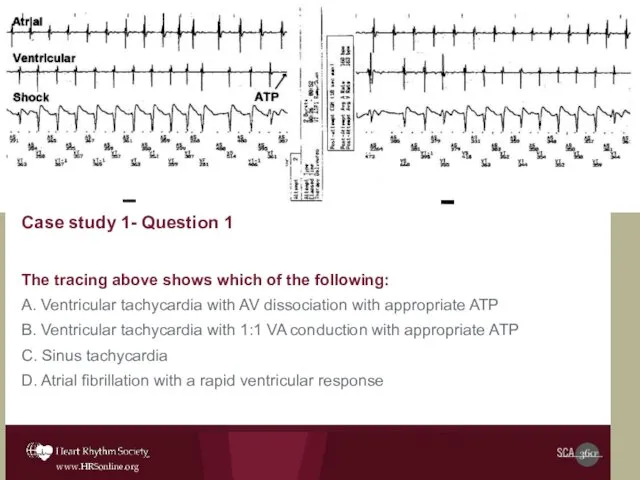
- 3. Case study 1- Question 1 The tracing above shows which of the following: A. Ventricular tachycardia
- 4. Case #1- Question 1 Answer The tracing above shows which of the following: A. Ventricular tachycardia
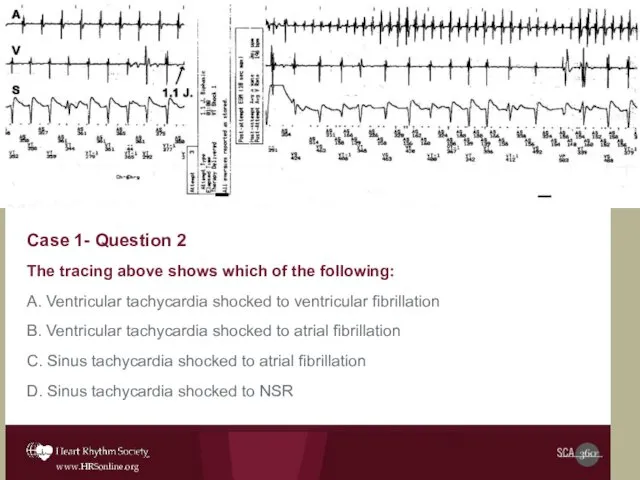
- 5. Case 1- Question 2 The tracing above shows which of the following: A. Ventricular tachycardia shocked
- 6. Case #1- Question 2 Answer The tracing above shows which of the following: A. Ventricular tachycardia
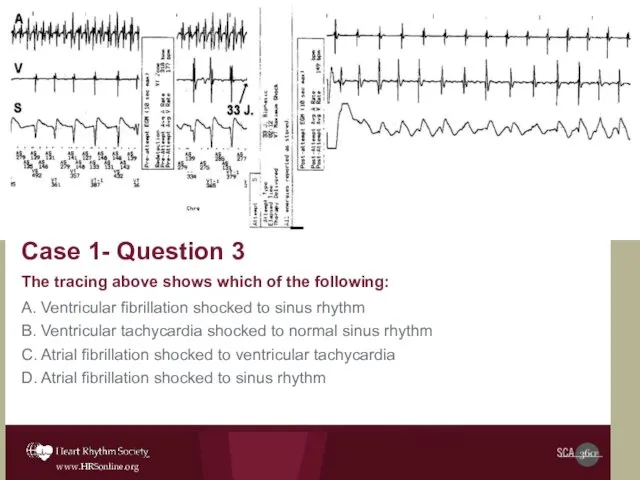
- 7. Case 1- Question 3 The tracing above shows which of the following: A. Ventricular fibrillation shocked
- 8. Case #1- Question 3 Answer The tracing above shows which of the following: A. Ventricular fibrillation
- 9. A. Start amiodarone B. Institute beta blocker therapy to prevent sinus tachycardia C. Program stability criteria
- 10. Case #1 – Question 4 Answer A. Start amiodarone B. Institute beta blocker therapy to prevent
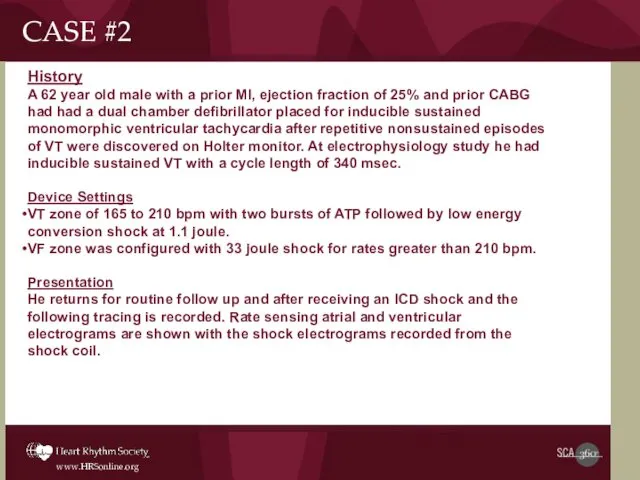
- 11. History A 62 year old male with a prior MI, ejection fraction of 25% and prior
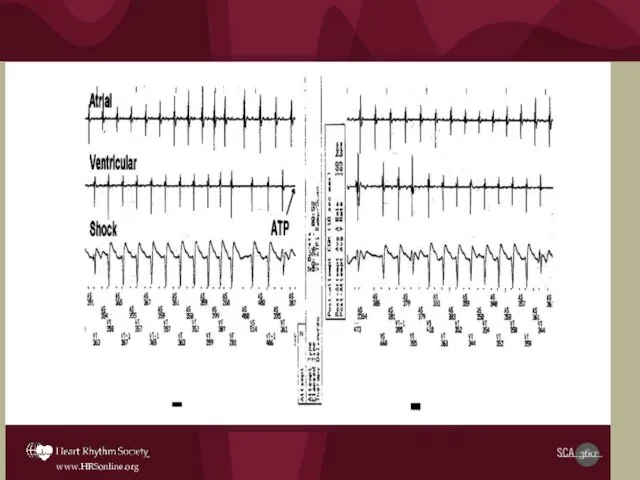
- 13. Initial rhythm in this tracing shows which of the following: Ventricular tachycardia with AV dissociation with
- 14. Initial rhythm in this tracing shows which of the following: A. Ventricular tachycardia with AV dissociation
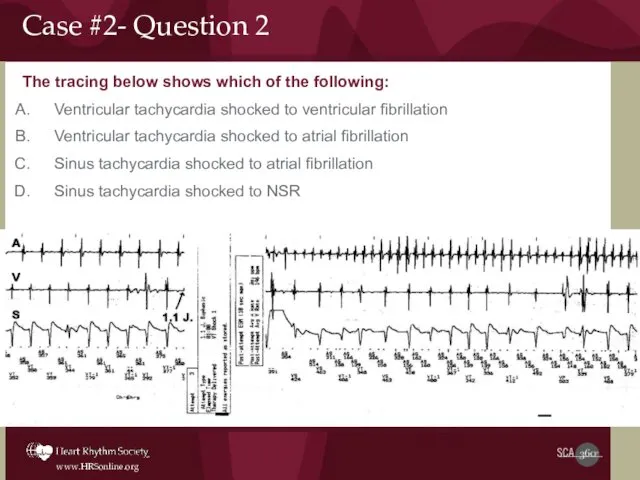
- 15. The tracing below shows which of the following: Ventricular tachycardia shocked to ventricular fibrillation Ventricular tachycardia
- 16. The tracing below shows which of the following: A. Ventricular tachycardia shocked to ventricular fibrillation B.
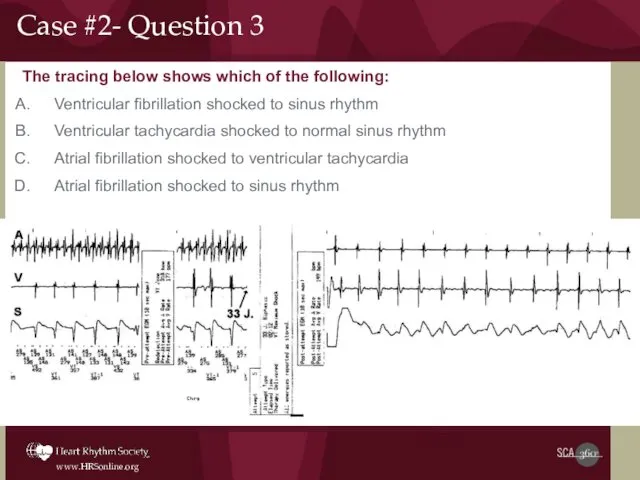
- 17. The tracing below shows which of the following: Ventricular fibrillation shocked to sinus rhythm Ventricular tachycardia
- 18. Case #2- Question 3 Answer The tracing below shows which of the following: Ventricular fibrillation shocked
- 19. The most appropriate therapy based on the available clinical information above would be which of the
- 20. The most appropriate therapy based on the available clinical information above would be which of the
- 21. CASE #3 History A 65-year-old male had prior 3 vessel disease and CABG with congestive heart
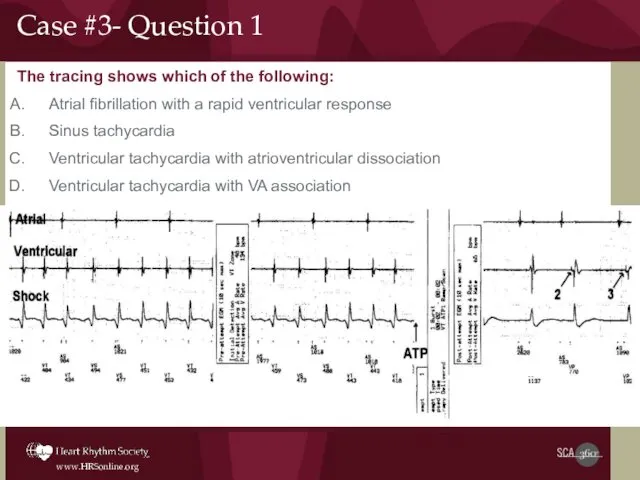
- 22. The tracing shows which of the following: Atrial fibrillation with a rapid ventricular response Sinus tachycardia
- 23. Case #3- Question 1 Answer The tracing shows which of the following: Atrial fibrillation with a
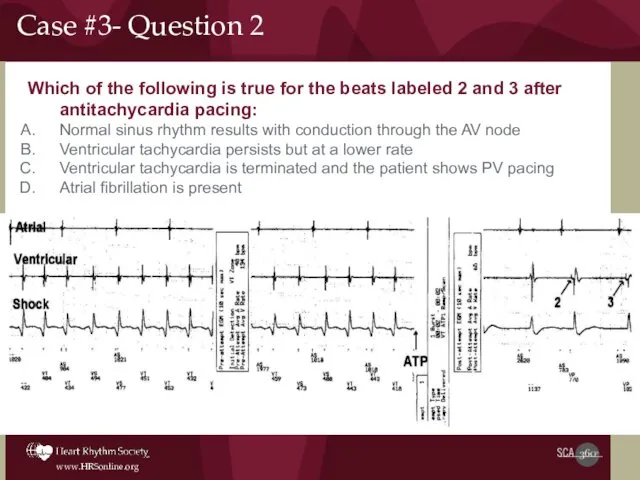
- 24. Which of the following is true for the beats labeled 2 and 3 after antitachycardia pacing:
- 25. Which of the following is true for the beats labeled 2 and 3 after antitachycardia pacing:
- 26. CASE #4 History A 55 year old women with a history of prior myocardial infarction and
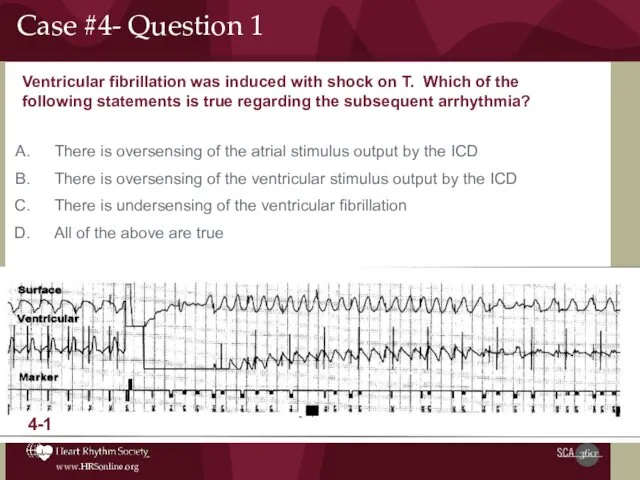
- 27. Ventricular fibrillation was induced with shock on T. Which of the following statements is true regarding
- 28. Ventricular fibrillation was induced with shock on T. Which of the following statements is true regarding
- 29. The most appropriate response to this would be which of the following? Make the ICD ventricular
- 30. The most appropriate response to this would be which of the following? Make the ICD ventricular
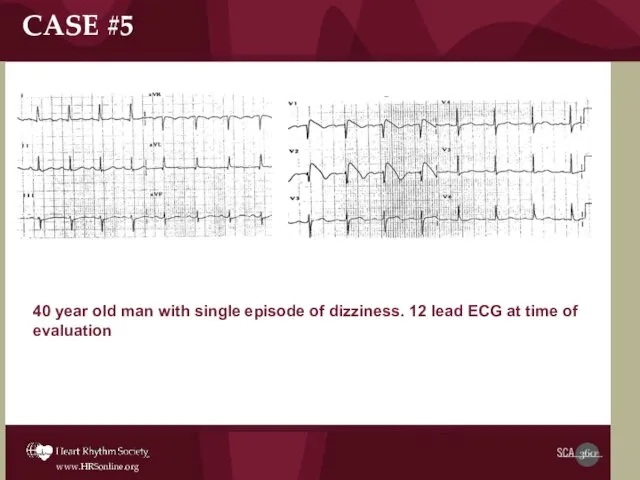
- 31. 40 year old man with single episode of dizziness. 12 lead ECG at time of evaluation
- 32. CASE #5- Question 1 Which of the following is not true related to the patient’s arrhythmia
- 33. Which of the following is not true related to the patient’s arrhythmia syndrome? The patient arrhythmias
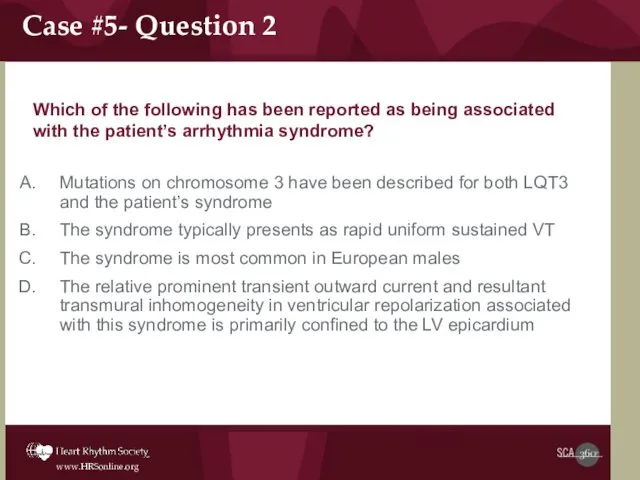
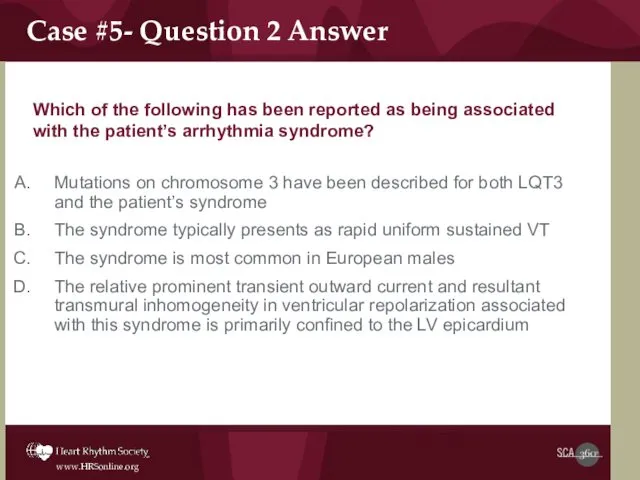
- 34. Which of the following has been reported as being associated with the patient’s arrhythmia syndrome? Mutations
- 35. Which of the following has been reported as being associated with the patient’s arrhythmia syndrome? Mutations
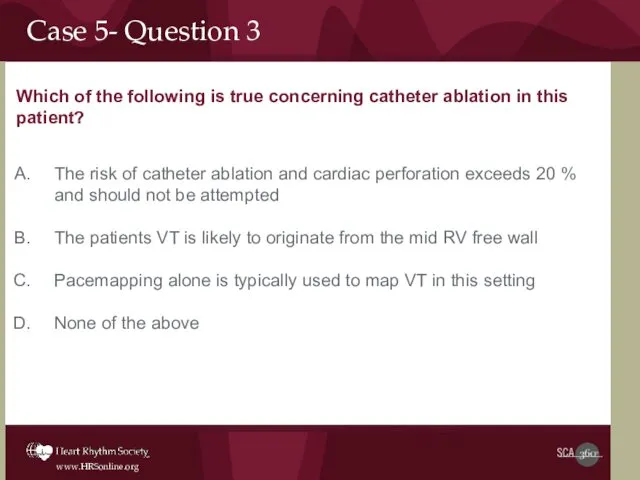
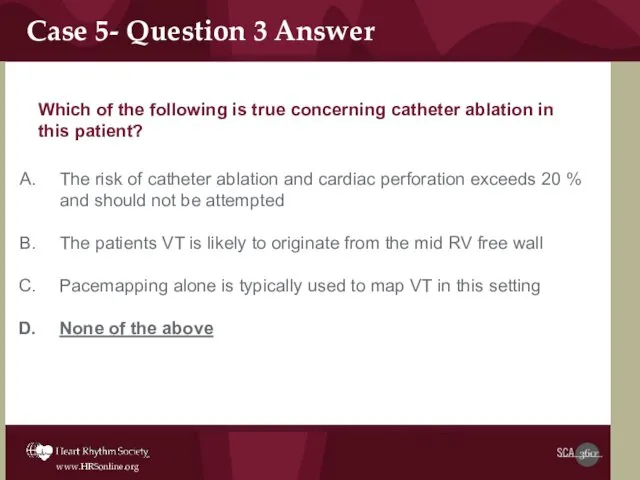
- 36. Case 5- Question 3 Which of the following is true concerning catheter ablation in this patient?
- 37. Which of the following is true concerning catheter ablation in this patient? Case 5- Question 3
- 38. CASE #6- Question 1 A 30 year old Spanish man is referred because of syncope and
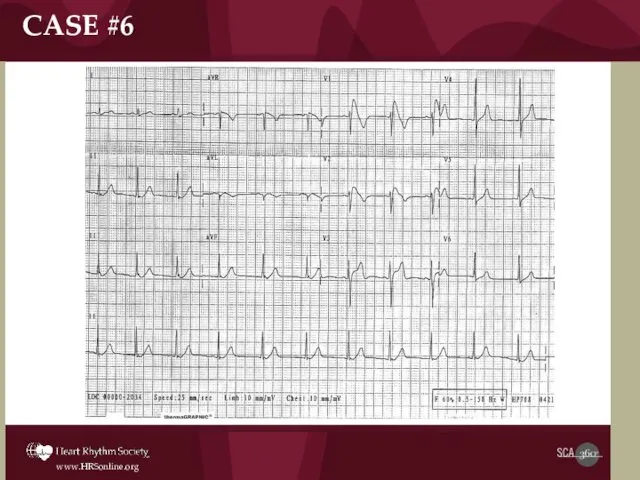
- 39. CASE #6
- 40. Case 6: Question 1 Administration of which of the following drugs would be helpful in the
- 42. Скачать презентацию
 Ауыз қуысының әр түрлі бөлімдерінің кілегей қабатының анатомиялық-топографиялық ерекшеліктері
Ауыз қуысының әр түрлі бөлімдерінің кілегей қабатының анатомиялық-топографиялық ерекшеліктері Выпускная квалификационная работа. Современные методы исследования дифтерии
Выпускная квалификационная работа. Современные методы исследования дифтерии Безопасность пациентов. Лекция 10
Безопасность пациентов. Лекция 10 Гипогонадизм. Ожирение. Лекция 8
Гипогонадизм. Ожирение. Лекция 8 Гипертоническая болезнь
Гипертоническая болезнь Захисні властивості крові. Групи крові. Зсідання крові
Захисні властивості крові. Групи крові. Зсідання крові Қансырау. Уақытша және нақты тоқтату әдістері
Қансырау. Уақытша және нақты тоқтату әдістері Правила гигиенического ухода за новорожденными (уход за кожей, слизистой, обработка пупочной ранки, гигиенические ванны)
Правила гигиенического ухода за новорожденными (уход за кожей, слизистой, обработка пупочной ранки, гигиенические ванны) Синдром синусового узла
Синдром синусового узла Лечение гестозов
Лечение гестозов Биоэтика и безопасность пациента. Биоэтика и защита прав пациента
Биоэтика и безопасность пациента. Биоэтика и защита прав пациента Гормональные препараты стероидного строения. Противовоспалительные средства. Средства, влияющие на миометрий
Гормональные препараты стероидного строения. Противовоспалительные средства. Средства, влияющие на миометрий Оболочки головною мозга
Оболочки головною мозга Заболевания надпочечников. Синдром Иценко-Кушинга. Болезнь Аддисона
Заболевания надпочечников. Синдром Иценко-Кушинга. Болезнь Аддисона Рекомендации ESC по артериальной гипертензии
Рекомендации ESC по артериальной гипертензии Нейропротезирование. История нейропротезирования
Нейропротезирование. История нейропротезирования Описторхоз. Характеристика гельминтов
Описторхоз. Характеристика гельминтов Саңырауқұлақтарға қарсы дз вирусқа қарсы дз
Саңырауқұлақтарға қарсы дз вирусқа қарсы дз Общая фармакология. Фармакодинамика
Общая фармакология. Фармакодинамика Ішектің қабыну ауруларының ажырату диагностикасы
Ішектің қабыну ауруларының ажырату диагностикасы Возбудители вирусных респираторных инфекций. (Лекция 17)
Возбудители вирусных респираторных инфекций. (Лекция 17) Моногенные болезни
Моногенные болезни Врожденный вывих бедра
Врожденный вывих бедра Физиологические роды
Физиологические роды Развитие репродуктивной системы женщины. Нейроэндокринная регуляция менструального цикла
Развитие репродуктивной системы женщины. Нейроэндокринная регуляция менструального цикла Нейропатии рук (локтевой, лучевой, срединый.)
Нейропатии рук (локтевой, лучевой, срединый.) Хронический гастрит и функциональная диспепсия. Киотский протокол. Профессор Е.И. Ткаченко
Хронический гастрит и функциональная диспепсия. Киотский протокол. Профессор Е.И. Ткаченко Методы исследований заболеваний печени и желчного пузыря
Методы исследований заболеваний печени и желчного пузыря