Содержание
- 2. 1. ASTHMA Asthma is a chronic inflammatory disorder of airways with episodic airway obstruction . Many
- 3. Asthma Usually associated with airflow obstruction of variable severity. Airflow obstruction is usually reversible, either spontaneously,
- 4. BURDEN OF ILLNESS Significant cause of school/work absence. Health care expenditures very high. Morbidity and mortality
- 5. Asthma Triggers Early childhood caused by viral Late by : Allergens Dust mites, pollen, indoor and
- 6. May predispose to asthma Childhood infections, e.g. respiratory syncytial virus Allergen exposure, e.g. house dust mite,
- 7. May protect against asthma Living on farm Large families Childhood infections, including parasites Predominance of lactobacilli
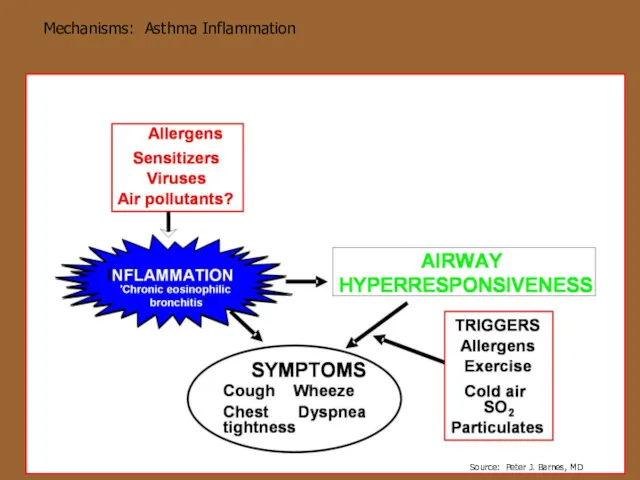
- 8. Mechanisms: Asthma Inflammation
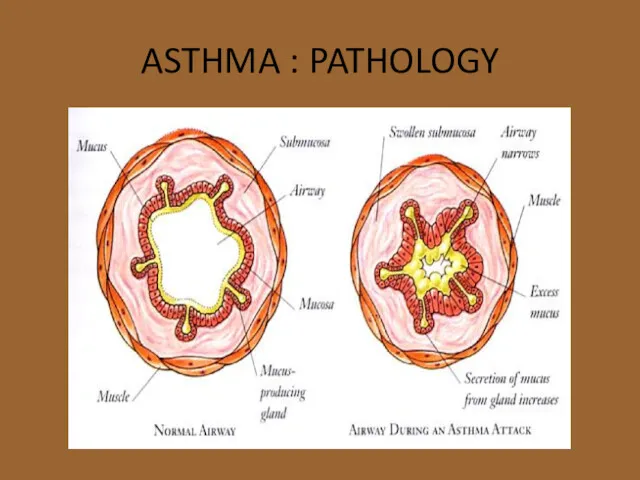
- 9. ASTHMA : PATHOLOGY
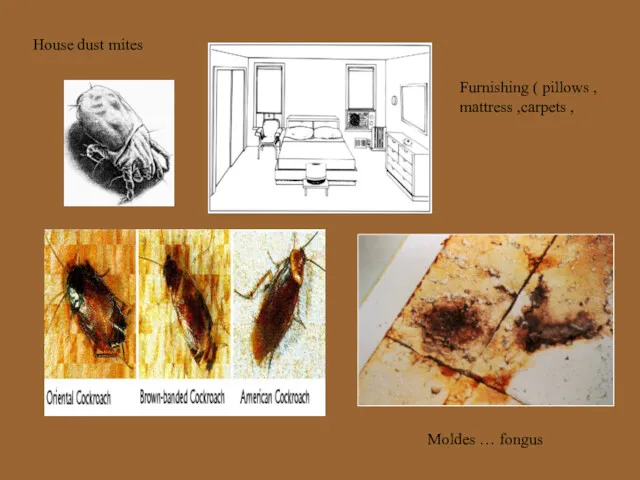
- 10. House dust mites Moldes … fongus Furnishing ( pillows , mattress ,carpets ,
- 11. PETS People allergic to pets should not have them in the house. At a minimum, do
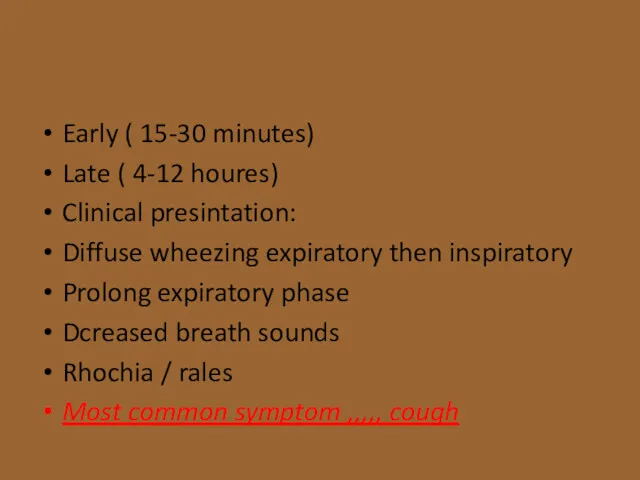
- 12. Early ( 15-30 minutes) Late ( 4-12 houres) Clinical presintation: Diffuse wheezing expiratory then inspiratory Prolong
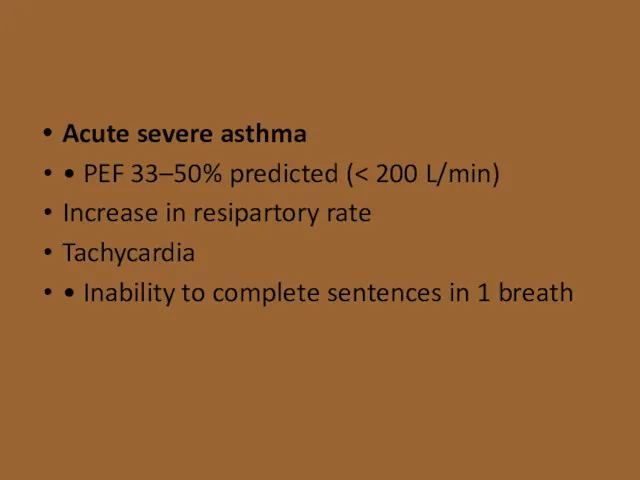
- 13. Acute severe asthma • PEF 33–50% predicted ( Increase in resipartory rate Tachycardia • Inability to
- 14. Life-threatening features • PEF • SpO2 treated with oxygen) • Normal or raised PaCO2 • Silent
- 15. Diagnostic Testing Complete blood count Chest x ray ,,,, hyperinflation chest IgE level Sinus xray not
- 16. PEAK FLOW METER Diagnosis of ASTHMA or COPD can be confirmed by demonstrating the presence of
- 17. Diagnostic Testing Spirometry Recommended to do spirometry pre- and post- use of an albuterol MDI to
- 18. Diagnostic Testing Spirometry Can be used to identify reversible airway obstruction due to triggers Can diagnose
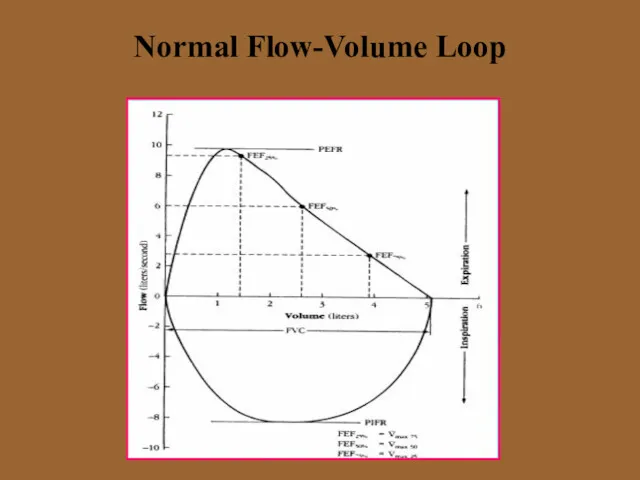
- 20. Normal Flow-Volume Loop
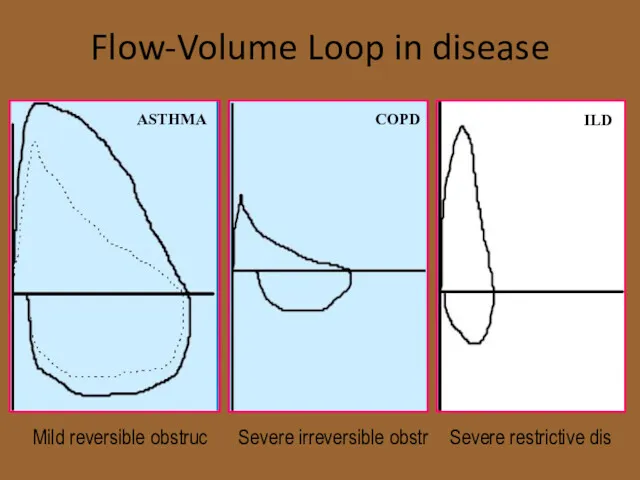
- 21. Flow-Volume Loop in disease Mild reversible obstruc Severe irreversible obstr Severe restrictive dis ASTHMA COPD ILD
- 22. Diagnostic Testing Methacholine challenge Most common bronchoprovocative test Patients breathe in increasing amounts of methacholine and
- 23. Diagnostic testing Diagnostic trial of anti-inflammatory medication (preferably corticosteroids) or an inhaled bronchodilator Especially helpful in
- 24. Goals of Asthma Treatment Control chronic and nocturnal symptoms Maintain normal activity, including exercise Prevent acute
- 25. Pharmacotherapy Albuterol (salbutamol) Short-acting beta2-agonist ATP to cAMP leads to relaxation of bronchial smooth muscle, inhibition
- 26. Pharmacotherapy Long-acting beta2-agonists (LABA) Beta2-receptors are the predominant receptors in bronchial smooth muscle Stimulate ATP- cAMP
- 27. Pharmacotherapy Long-acting beta2-agonists (LABA) Salmeterol (Serevent) , formoterol Salmeterol with fluticasone (seritide) Formoterol with budesonide (symbicort)
- 28. Pharmacotherapy Inhaled Corticosteroids Anti-inflammatory Act locally in lungs Some systemic absorption Risks of possible growth retardation
- 29. Pharmacotherapy Mast cell stabilizers (cromolyn /nedocromil) Inhibits release of mediators from mast cells (degranulation) after exposure
- 30. Pharmacotherapy Leukotriene receptor antagonists Leukotriene - mediated effects include: Airway edema Smooth muscle contraction Altered cellular
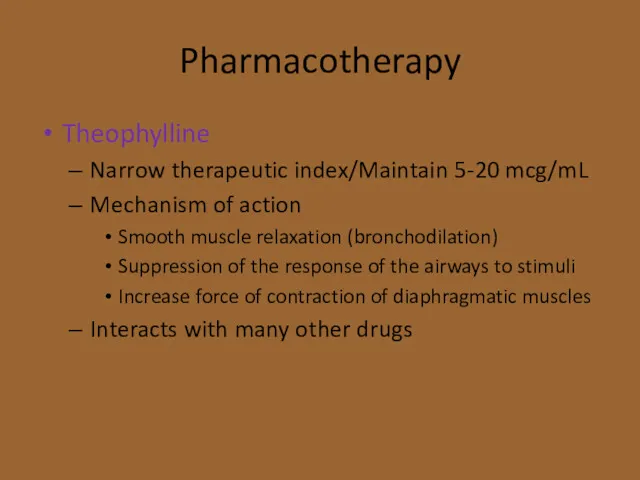
- 31. Pharmacotherapy Theophylline Narrow therapeutic index/Maintain 5-20 mcg/mL Mechanism of action Smooth muscle relaxation (bronchodilation) Suppression of
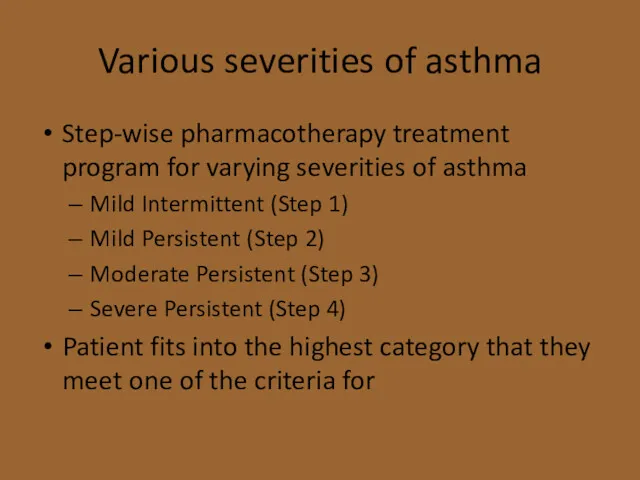
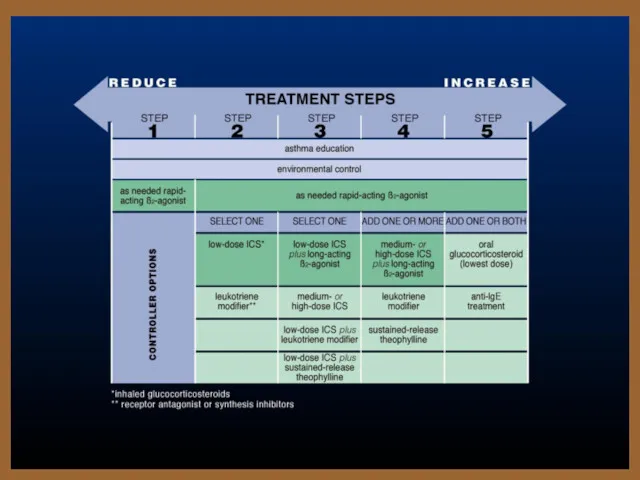
- 32. Various severities of asthma Step-wise pharmacotherapy treatment program for varying severities of asthma Mild Intermittent (Step
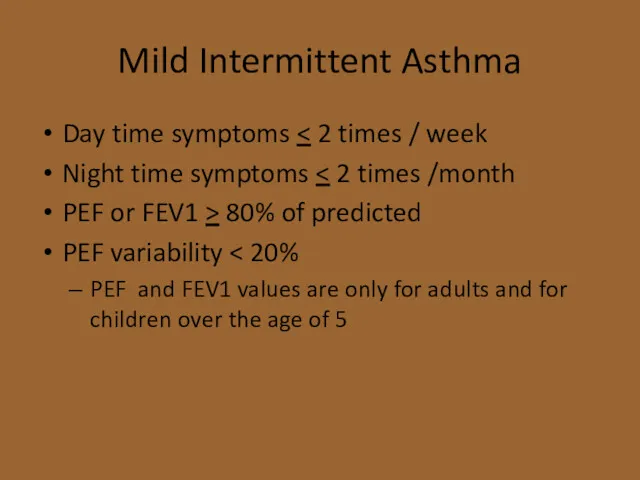
- 33. Mild Intermittent Asthma Day time symptoms Night time symptoms PEF or FEV1 > 80% of predicted
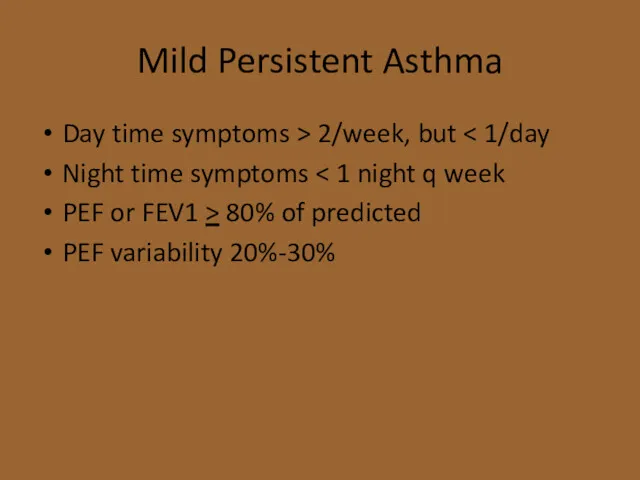
- 34. Mild Persistent Asthma Day time symptoms > 2/week, but Night time symptoms PEF or FEV1 >
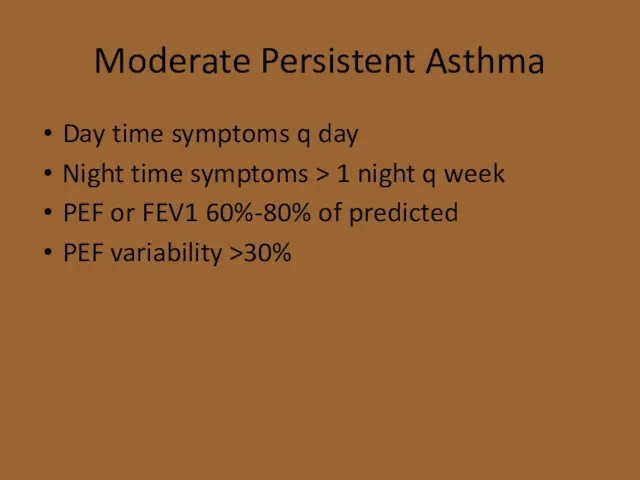
- 35. Moderate Persistent Asthma Day time symptoms q day Night time symptoms > 1 night q week
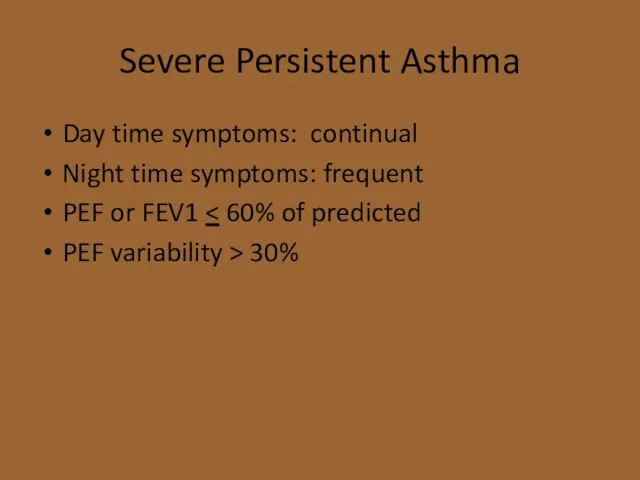
- 36. Severe Persistent Asthma Day time symptoms: continual Night time symptoms: frequent PEF or FEV1 PEF variability
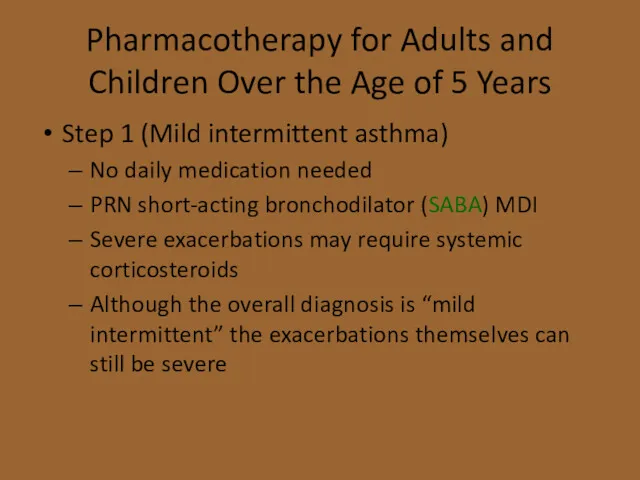
- 37. Pharmacotherapy for Adults and Children Over the Age of 5 Years Step 1 (Mild intermittent asthma)
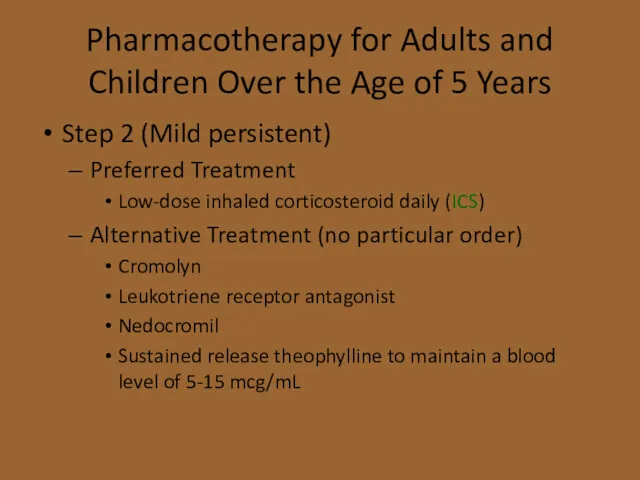
- 38. Pharmacotherapy for Adults and Children Over the Age of 5 Years Step 2 (Mild persistent) Preferred
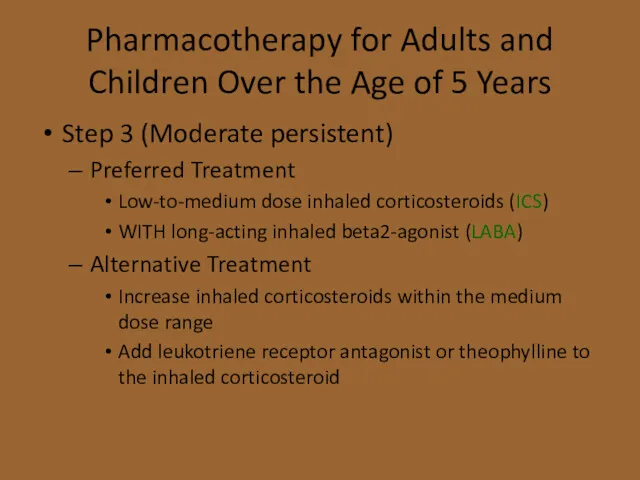
- 39. Pharmacotherapy for Adults and Children Over the Age of 5 Years Step 3 (Moderate persistent) Preferred
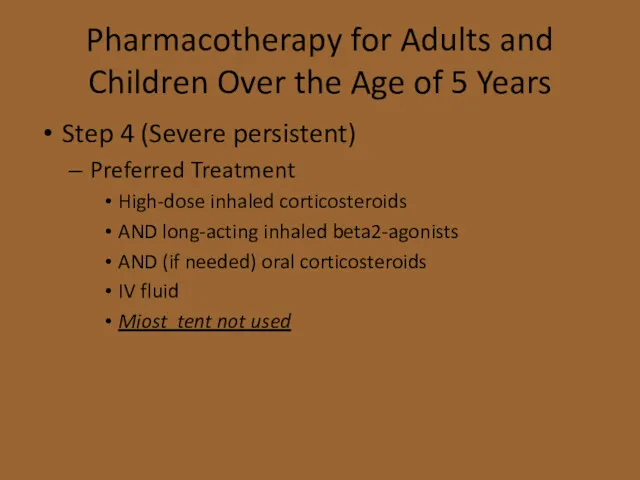
- 40. Pharmacotherapy for Adults and Children Over the Age of 5 Years Step 4 (Severe persistent) Preferred
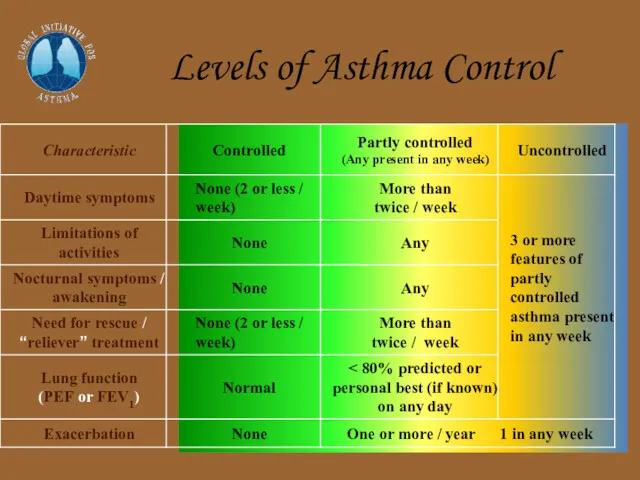
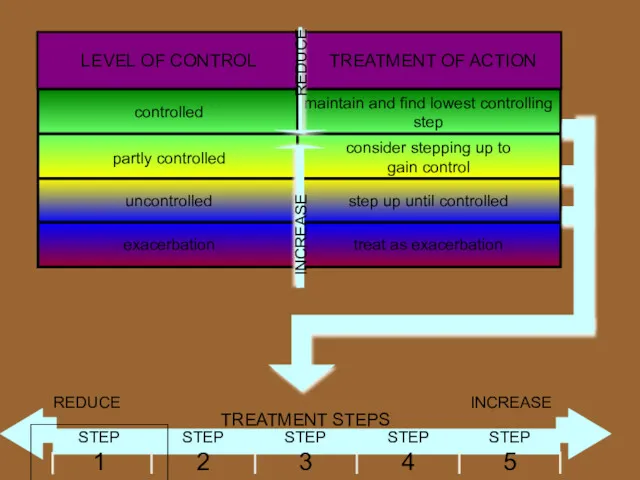
- 42. Levels of Asthma Control
- 44. Short acting and long acting b2-agonist Long acting b2-agonist Short acting b2-agonist
- 46. Combination (ICS)+(LABA) Flixotide (ICS) + Serevent (LABA) Pulmicort (ICS)+ Oxis (LABA)
- 47. Acute Exacerbations Inhaled albuterol is the treatment of choice in absence of impending respiratory failure MDI
- 48. Acute Exacerbations Beneficial Inhaled atrovent added to beta2-agonists High-dose inhaled corticosteroids MDI with spacer as effective
- 49. Exercise-induced Bronchospasm Evaluate for underlying asthma and treat SABA are best pre-treatment Mast cell stabilizers less
- 51. Скачать презентацию




 Раневые инфекции. Этиологическая структура
Раневые инфекции. Этиологическая структура Осложнения чрескожных коронарных вмешательств (ЧКВ)
Осложнения чрескожных коронарных вмешательств (ЧКВ) Reconstruction préprothétique par technique directe. Restaurer la dent deulpe
Reconstruction préprothétique par technique directe. Restaurer la dent deulpe Мышцы и фасции туловища (для массажиста)
Мышцы и фасции туловища (для массажиста) Металлы и сплавы в стоматологии
Металлы и сплавы в стоматологии Отравляющие вещества и АОХВ нервно-паралитического действия. Клиника, диагностика, лечение
Отравляющие вещества и АОХВ нервно-паралитического действия. Клиника, диагностика, лечение Urinary system
Urinary system Нерв жүйесінің тұқым қуалайтын –дегенеративті ауруларың жіктелуі
Нерв жүйесінің тұқым қуалайтын –дегенеративті ауруларың жіктелуі Сестринский процесс при нейрохирургических операциях, операциях на сосудах, урологических операций
Сестринский процесс при нейрохирургических операциях, операциях на сосудах, урологических операций Анализ опыта реализации отечественных и зарубежных программ по раннему вмешательству
Анализ опыта реализации отечественных и зарубежных программ по раннему вмешательству Дитячі інфекційні хвороби
Дитячі інфекційні хвороби Острые вирусные гепатиты
Острые вирусные гепатиты Триаж или медицинская сортировка. Первичный триаж в оборонительных войсках
Триаж или медицинская сортировка. Первичный триаж в оборонительных войсках Акушерлік-гинекологиялық көмекті ұйымдастыру
Акушерлік-гинекологиялық көмекті ұйымдастыру Денсаулық сақтау жүйесі үлгілері: мемлекеттік,жеке меншіктік, медициналық сақтандыру
Денсаулық сақтау жүйесі үлгілері: мемлекеттік,жеке меншіктік, медициналық сақтандыру Дифференциальная диагностика затемнений в легких
Дифференциальная диагностика затемнений в легких Иммунная система человека. Антигены. Антитела
Иммунная система человека. Антигены. Антитела Сосудистые анастомозы РУС
Сосудистые анастомозы РУС Асқорыту органдарының қатерсіз және қатерлі ісіктері
Асқорыту органдарының қатерсіз және қатерлі ісіктері Санаторно-курортное лечение
Санаторно-курортное лечение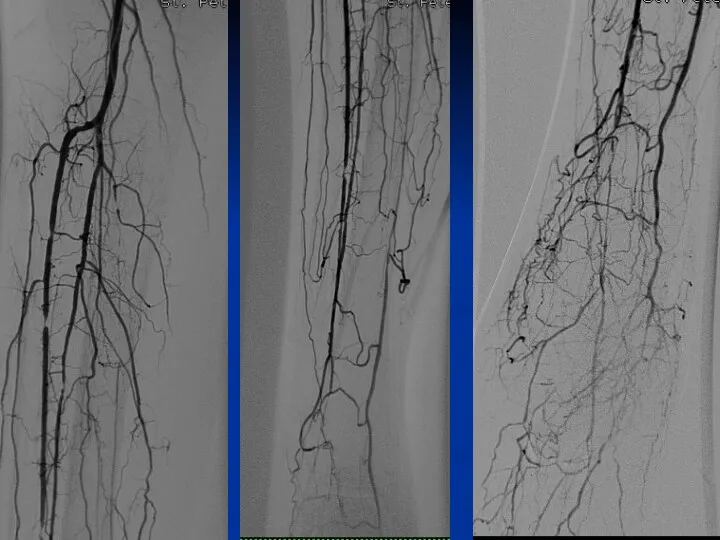 Артериальные доступы, используемые для выполнения ПАП у пациентов с КИНК
Артериальные доступы, используемые для выполнения ПАП у пациентов с КИНК Денсаулық сақтау ұйымдарының бастапқы медициналық құжаттама нысандарын бекіту туралы Қазақстан Республикасы
Денсаулық сақтау ұйымдарының бастапқы медициналық құжаттама нысандарын бекіту туралы Қазақстан Республикасы Жалпы сөйлеу тілінің жетіспеушілігі
Жалпы сөйлеу тілінің жетіспеушілігі Захворювання та профілактика серця
Захворювання та профілактика серця Исследование сердечной деятельности
Исследование сердечной деятельности Холера. Клиническая картина
Холера. Клиническая картина Center of vision correction ASTANA VISION
Center of vision correction ASTANA VISION Операціональна психодинамічна діагностика
Операціональна психодинамічна діагностика