Содержание
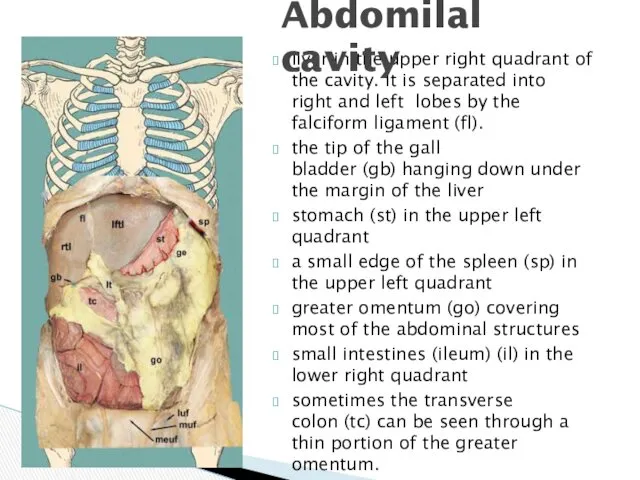
- 2. liver in the upper right quadrant of the cavity. It is separated into right and left
- 3. borders: superior: inferior surface of diaphragm Inferior: mesocolon transversum Contents: hepatic bursa, pregastric bursa, omental bursa,
- 4. Borders: Superior: mesocolon transversum Inferior: inlet of the lesser pelvis contents: Right & left paracolic canals
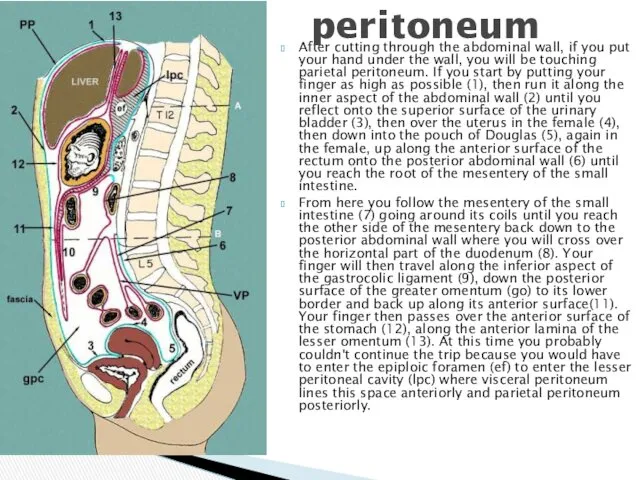
- 5. After cutting through the abdominal wall, if you put your hand under the wall, you will
- 6. lig. falciforme lig. coronarium hepatis lig. triangulare lig. hepatogastricum lig. hepatoduodenale lig. hepatocolicum lig. hepatorenale lig.
- 7. duodenojejunal recess superior ileocaecal recess inferior ileocaecal recess retrocaecal recess intersigmoid recess Recesses - pouches formed
- 8. Plica gastropancreatica Plica ileocecalis Plica duodenalis superior Plica duodenalis inferior Plica umbilicalis mediana Plica umbilicalis medialis
- 9. RIGHT MESENTERIC SINUS borders: medial-root of the mesentry Lateral – ascending colon Superior – transverse colon
- 10. Right paracolic canal communicates with right hepatic bursa Borders: Medial – ascending colon Lateral – parietalperitoneum
- 11. HEPATIC BURSA Borders: Superior – diaphragm Inferior – transverse mesocolon Anterior – anterior abdominal wall Medial
- 12. Pregastric bursa Borders: Anterior – left lobe of the liver and anterior abdominal wall Posterior –
- 13. BORDERS: Superior – lobus caudatus hepatis Inferior – mesocolon transversum Anterior – stomach & lesser omentum
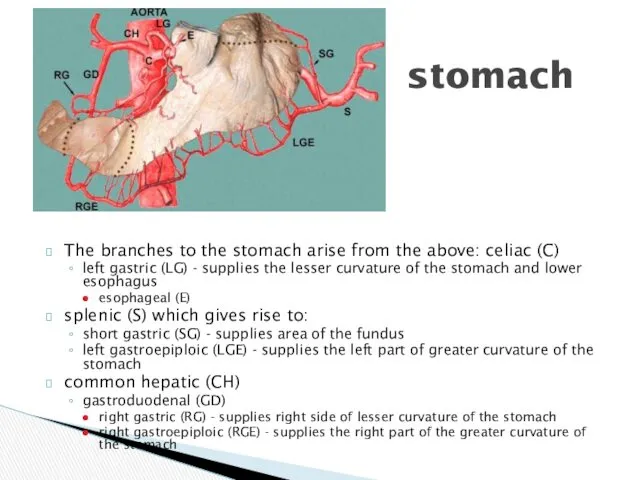
- 14. The branches to the stomach arise from the above: celiac (C) left gastric (LG) - supplies
- 15. The stomach drains either directly or indirectly into the portal vein as follows:short gastric veins (SG)
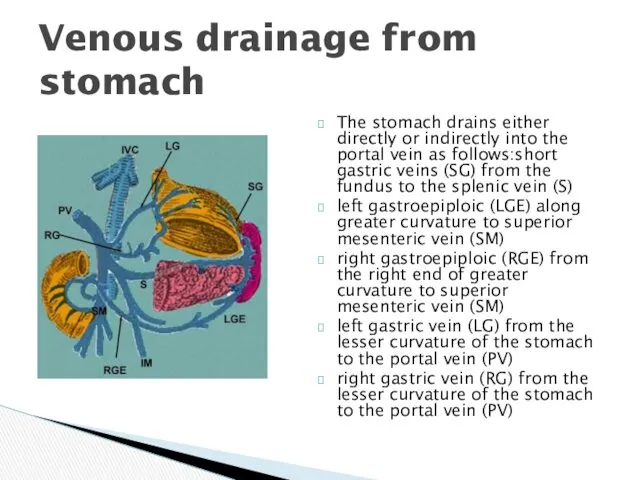
- 16. Nerve supply
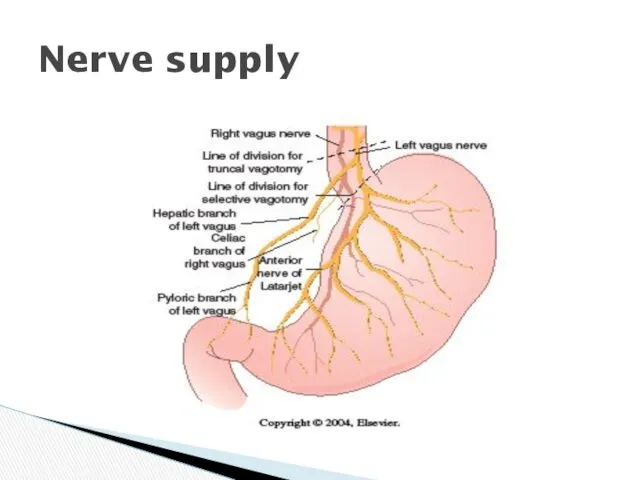
- 18. Gastritis (acute or stress) Produces inflammation of the mucosa. Can be associated with erosions and bleeding.
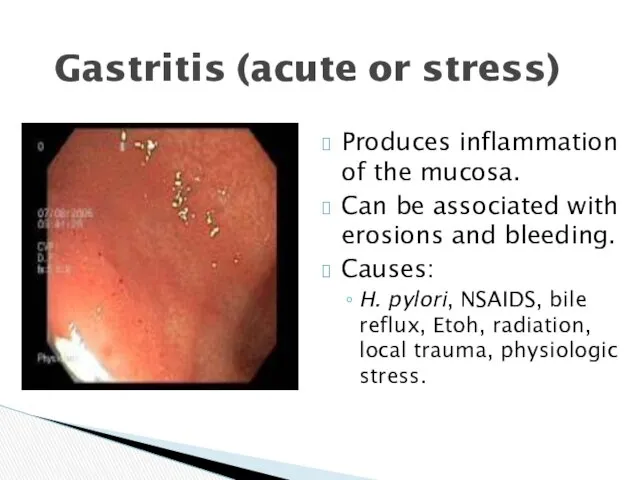
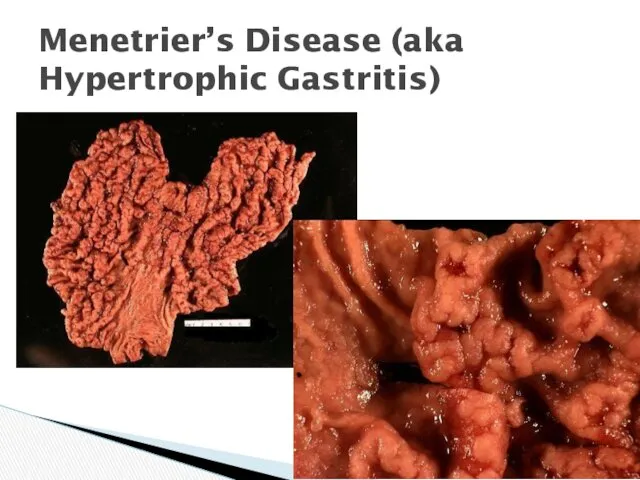
- 19. Menetrier’s Disease (aka Hypertrophic Gastritis)
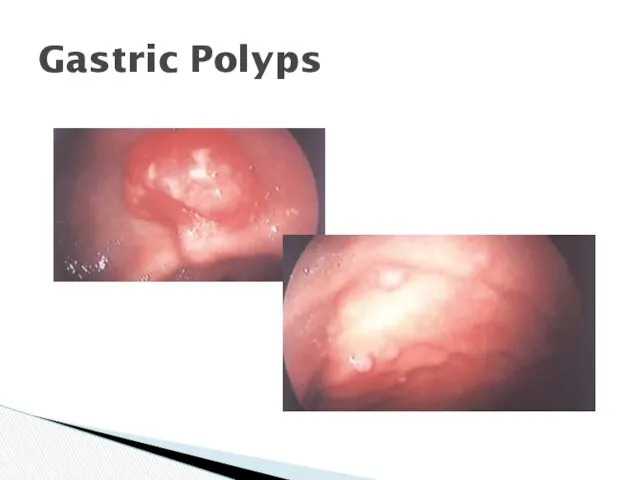
- 20. Gastric Polyps
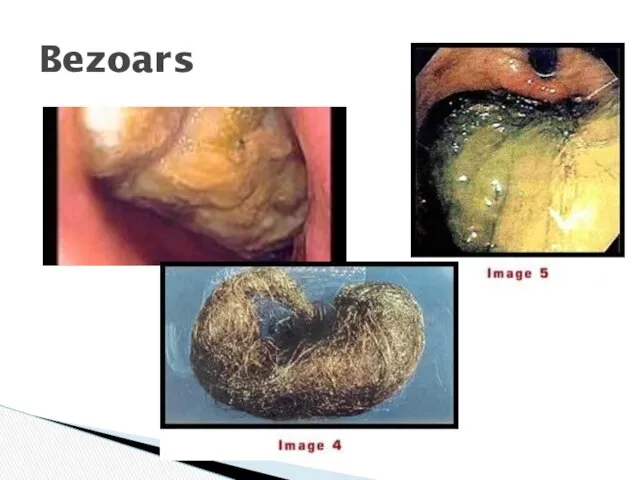
- 21. Bezoars
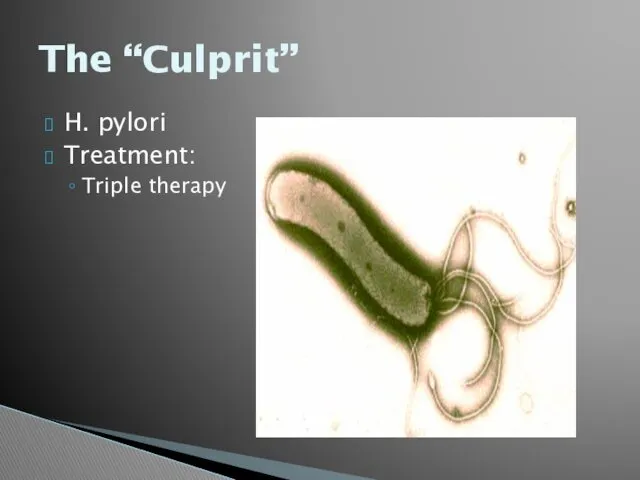
- 22. The “Culprit” H. pylori Treatment: Triple therapy
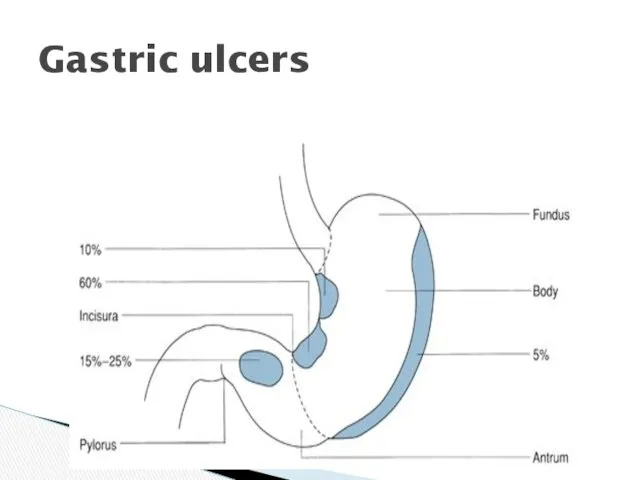
- 23. Gastric ulcers
- 24. Gastric Ulcers
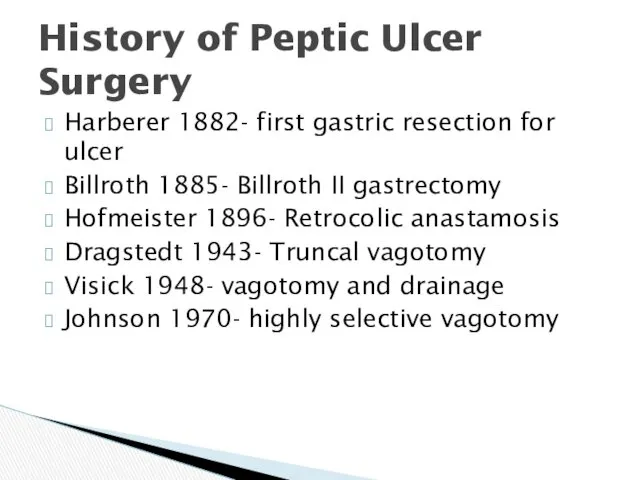
- 25. History of Peptic Ulcer Surgery Harberer 1882- first gastric resection for ulcer Billroth 1885- Billroth II
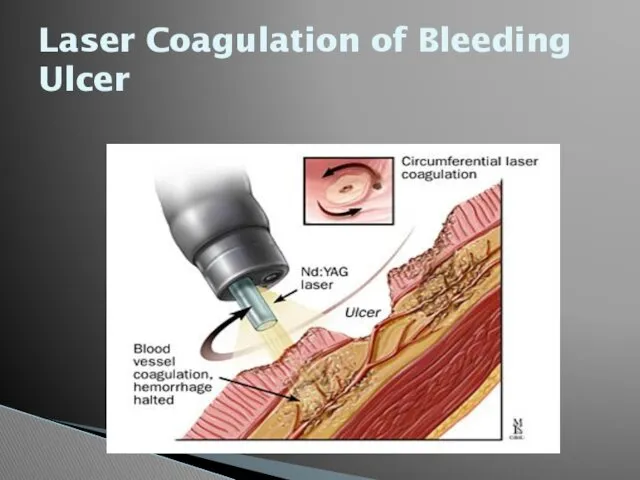
- 26. Laser Coagulation of Bleeding Ulcer
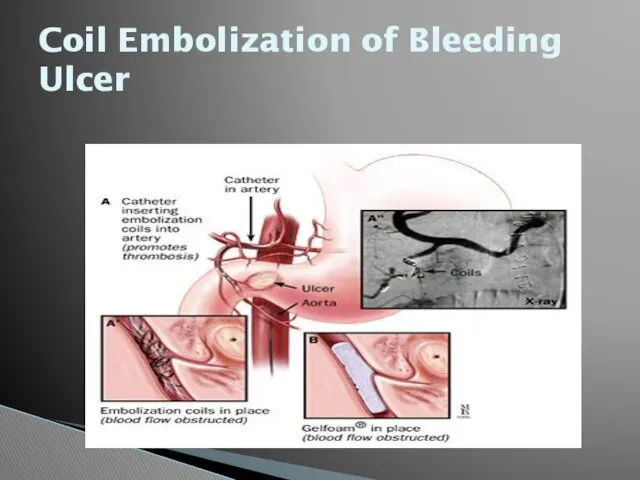
- 27. Coil Embolization of Bleeding Ulcer
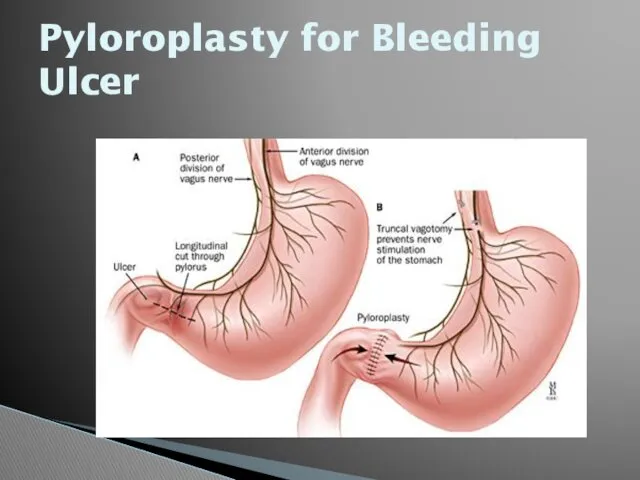
- 28. Pyloroplasty for Bleeding Ulcer
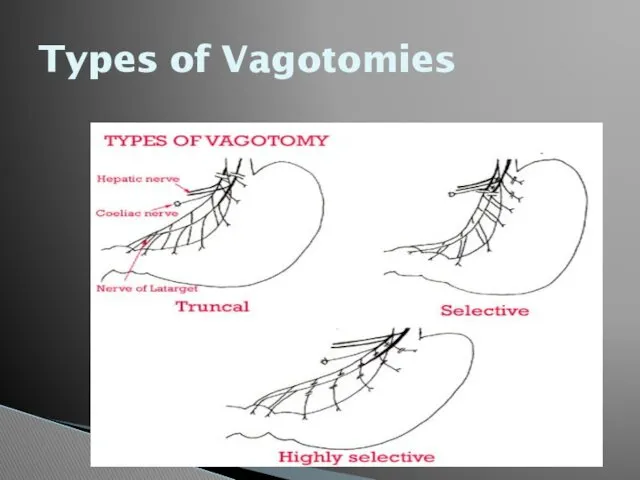
- 29. Open Surgical Procedures Truncal vagotomy and pyloroplasty Truncal vagotomy and gastrojejunostomy Truncal vagotomy and antrectomy Highly
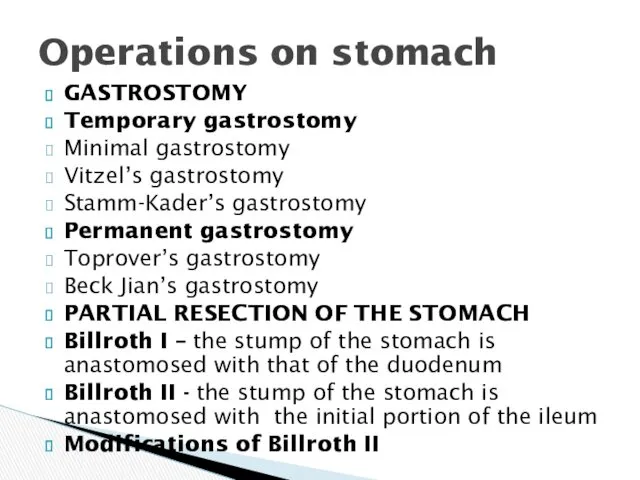
- 30. GASTROSTOMY Temporary gastrostomy Minimal gastrostomy Vitzel’s gastrostomy Stamm-Kader’s gastrostomy Permanent gastrostomy Toprover’s gastrostomy Beck Jian’s gastrostomy
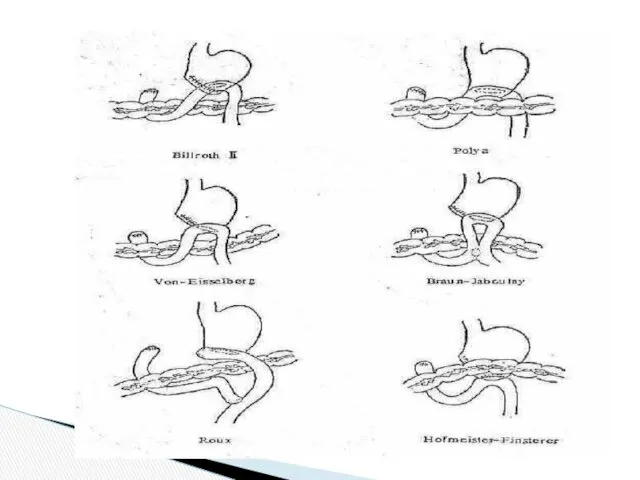
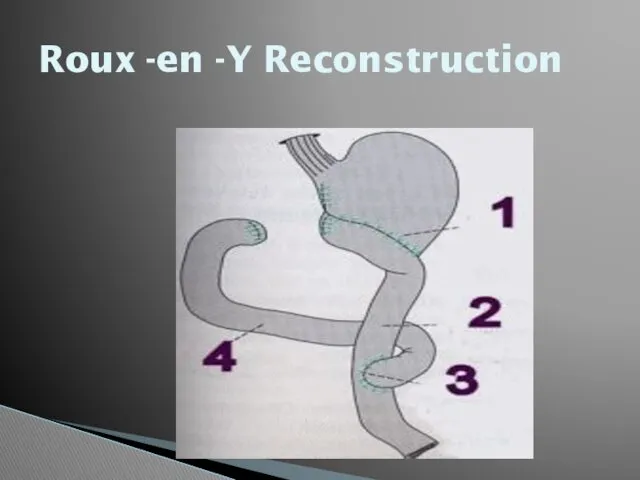
- 32. Roux -en -Y Reconstruction
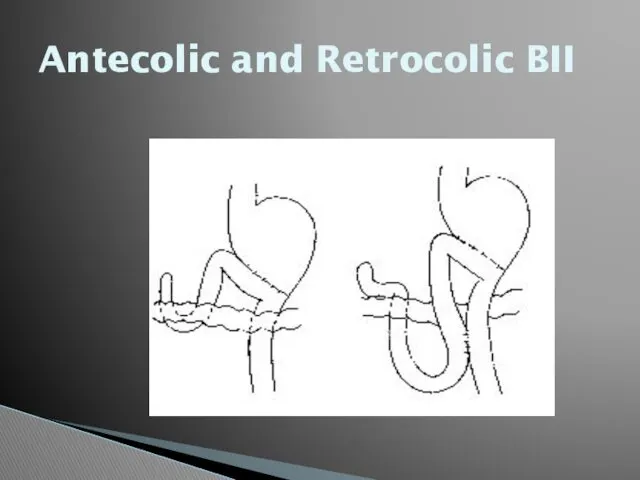
- 33. Antecolic and Retrocolic BII
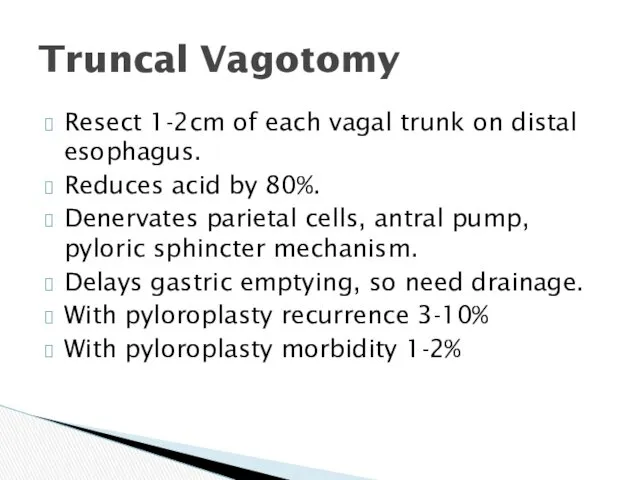
- 34. Truncal Vagotomy Resect 1-2cm of each vagal trunk on distal esophagus. Reduces acid by 80%. Denervates
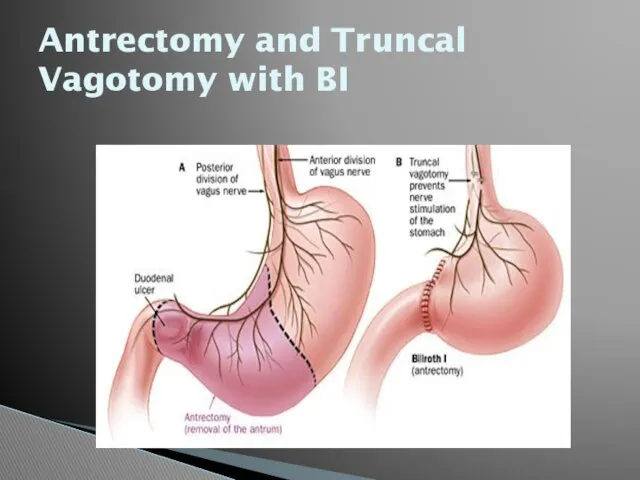
- 35. Antrectomy and Truncal Vagotomy with BI
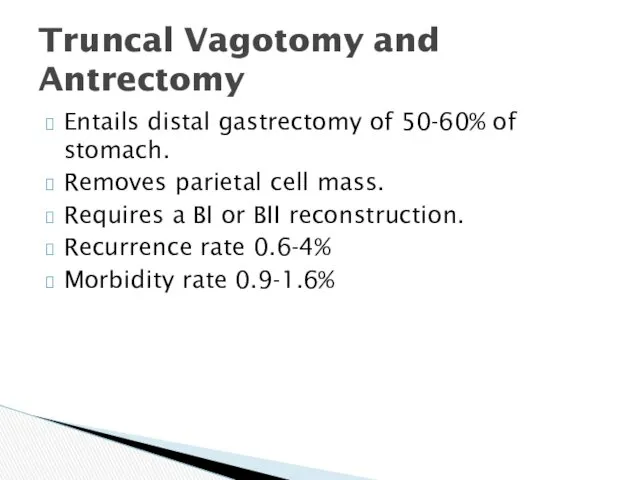
- 36. Truncal Vagotomy and Antrectomy Entails distal gastrectomy of 50-60% of stomach. Removes parietal cell mass. Requires
- 37. Selective Vagotomy Total denervation of the stomach from diaphragmatic crus to pylorus. Procedure still needs drainage,
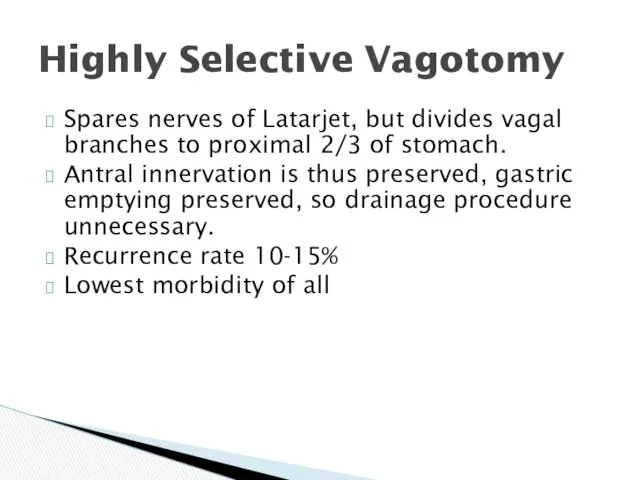
- 38. Highly Selective Vagotomy Spares nerves of Latarjet, but divides vagal branches to proximal 2/3 of stomach.
- 39. Types of Vagotomies
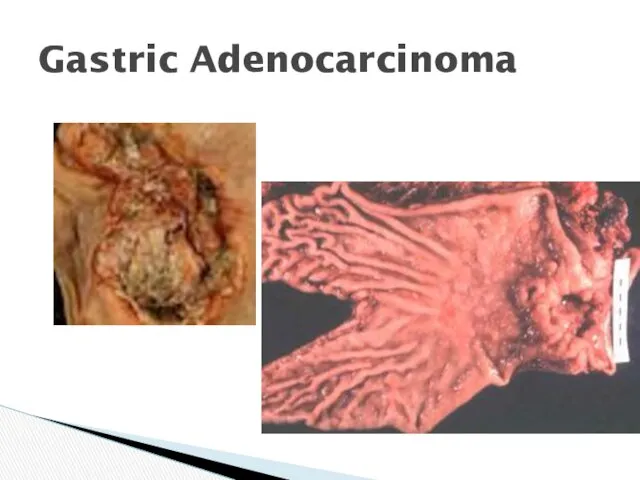
- 40. Gastric Adenocarcinoma
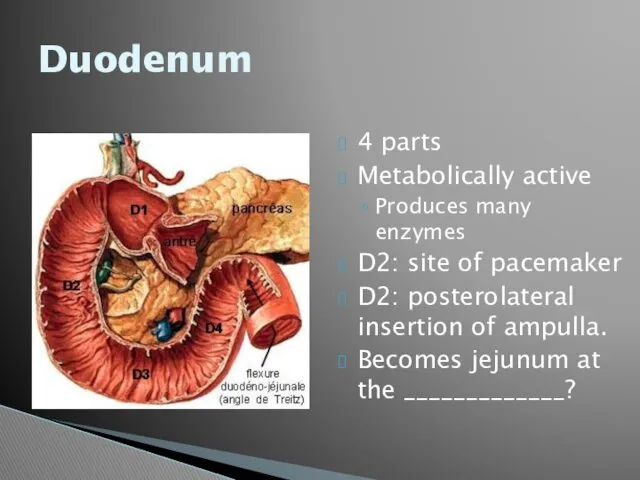
- 41. Duodenum 4 parts Metabolically active Produces many enzymes D2: site of pacemaker D2: posterolateral insertion of
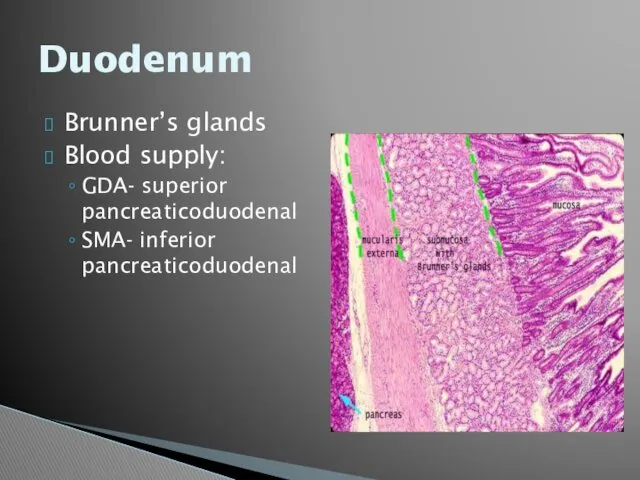
- 42. Duodenum Brunner’s glands Blood supply: GDA- superior pancreaticoduodenal SMA- inferior pancreaticoduodenal
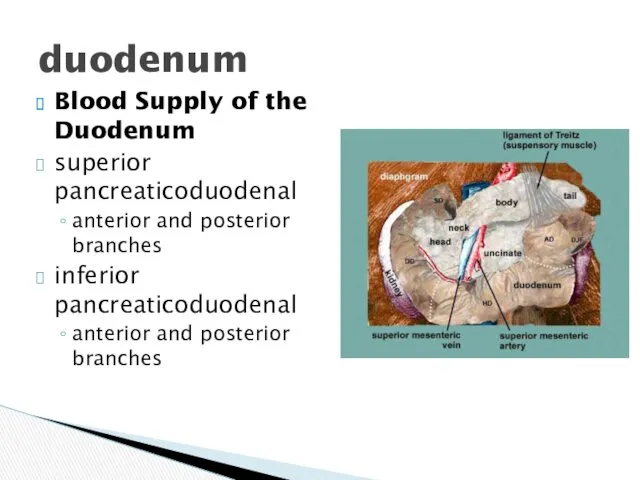
- 43. Blood Supply of the Duodenum superior pancreaticoduodenal anterior and posterior branches inferior pancreaticoduodenal anterior and posterior
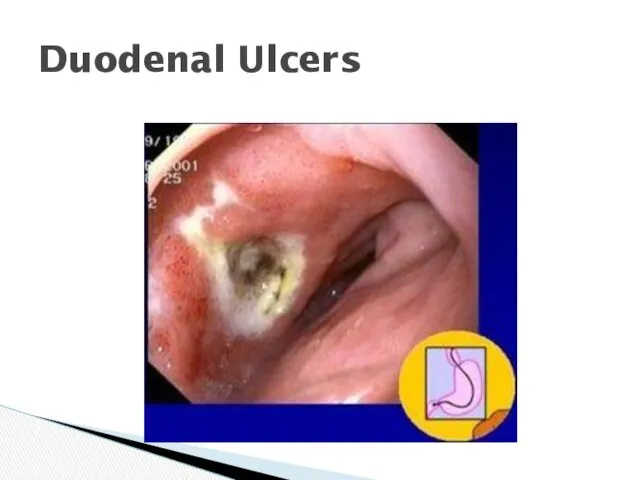
- 44. Duodenal Ulcers
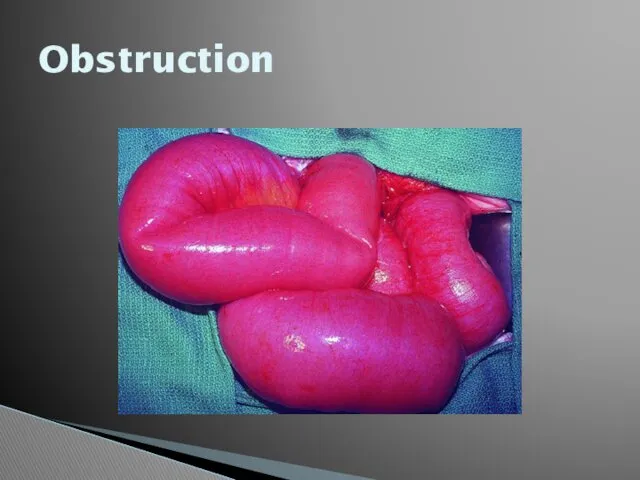
- 45. Obstruction
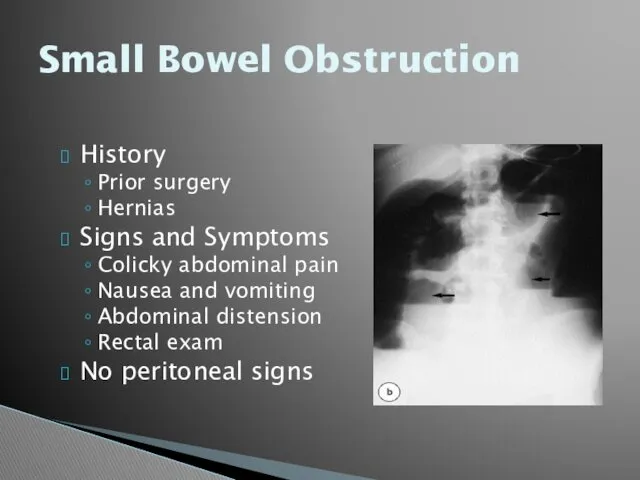
- 46. Small Bowel Obstruction History Prior surgery Hernias Signs and Symptoms Colicky abdominal pain Nausea and vomiting
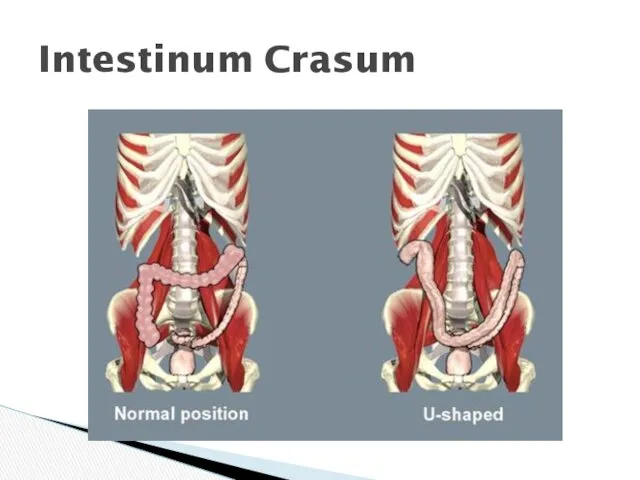
- 47. Intestinum Crasum
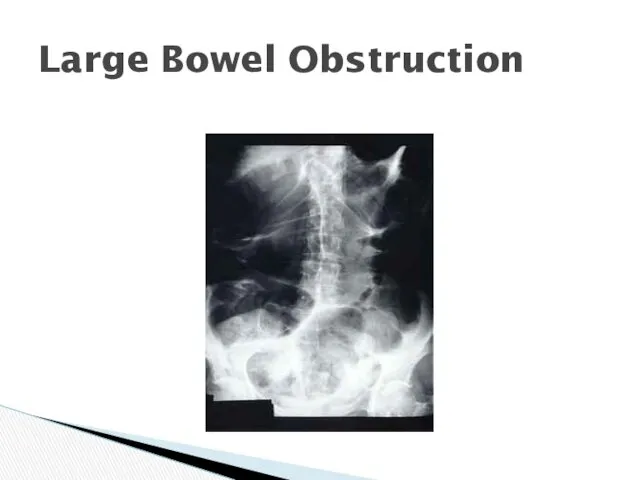
- 48. Large Bowel Obstruction
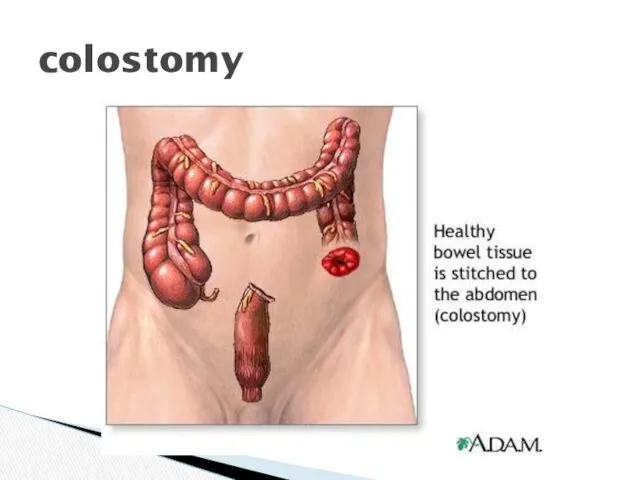
- 49. colostomy
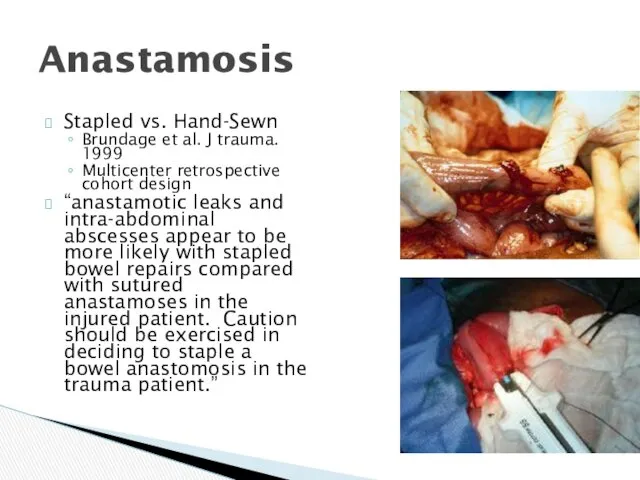
- 50. Anastamosis Stapled vs. Hand-Sewn Brundage et al. J trauma. 1999 Multicenter retrospective cohort design “anastamotic leaks
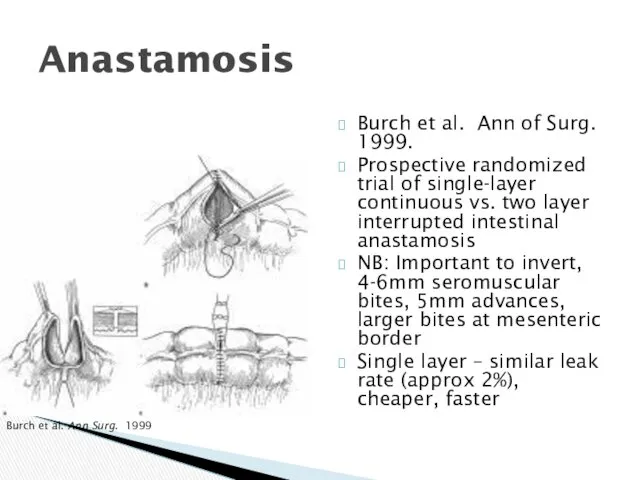
- 51. Anastamosis Burch et al. Ann of Surg. 1999. Prospective randomized trial of single-layer continuous vs. two
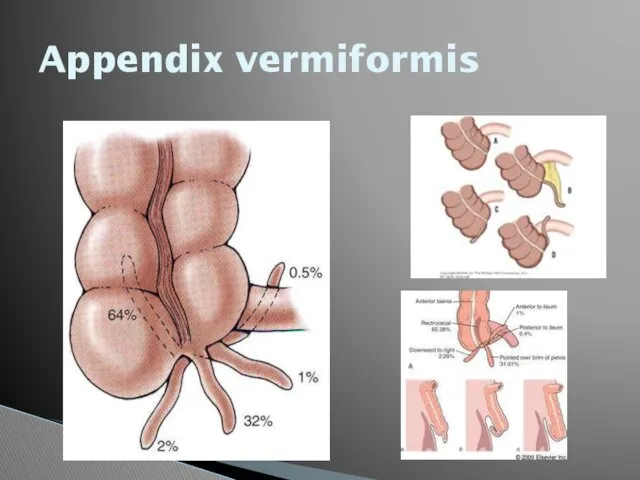
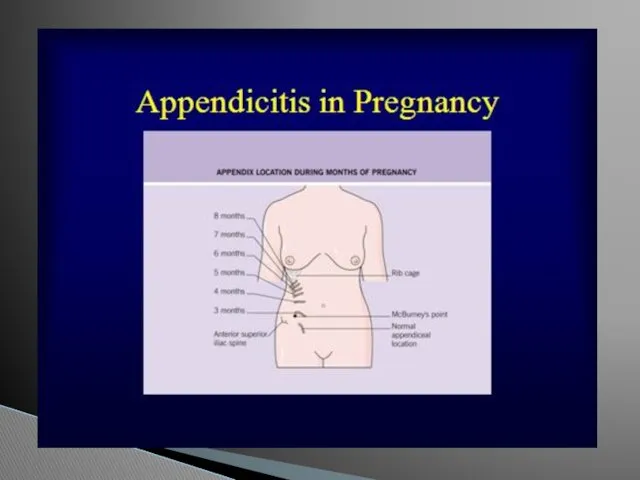
- 52. Appendix vermiformis
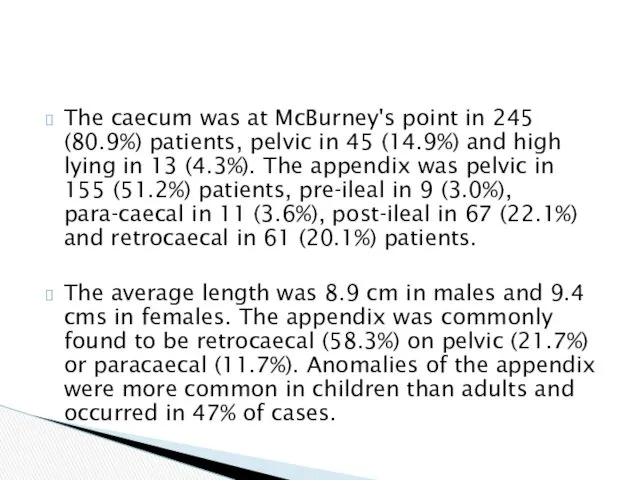
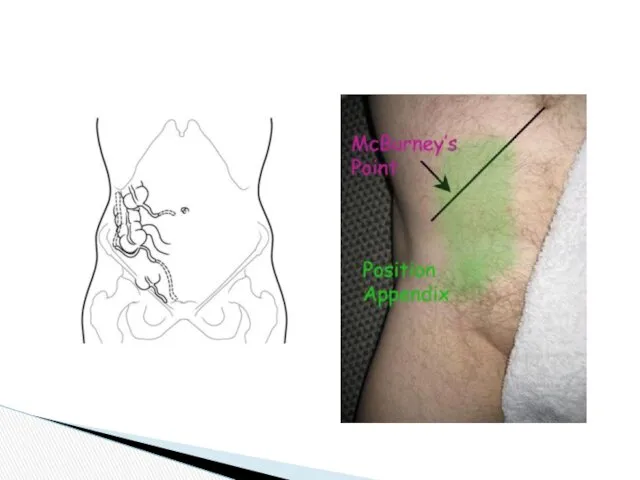
- 54. The caecum was at McBurney's point in 245 (80.9%) patients, pelvic in 45 (14.9%) and high
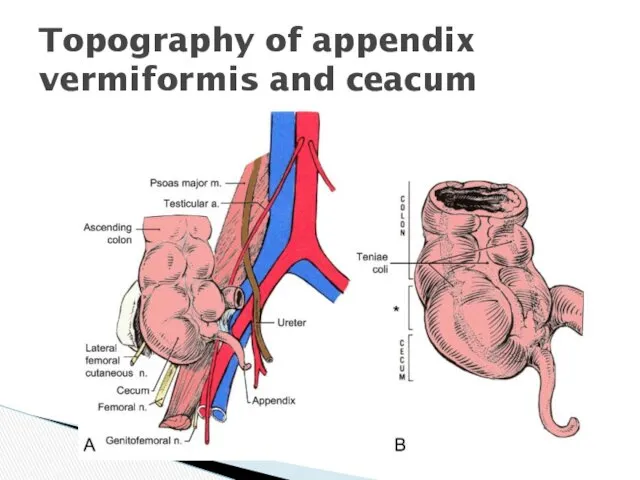
- 55. Topography of appendix vermiformis and ceacum
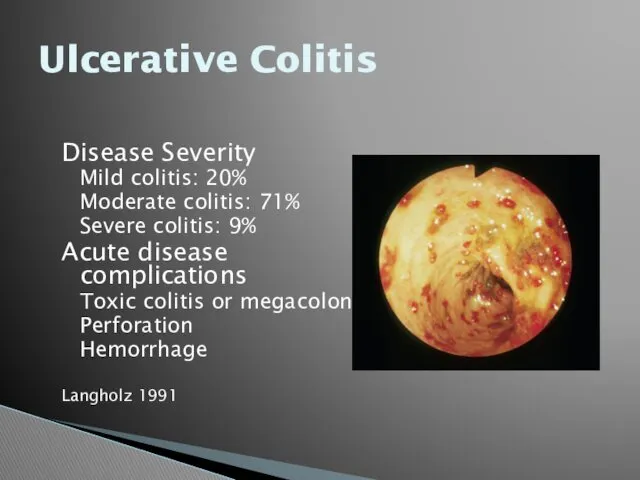
- 57. Ulcerative Colitis Disease Severity Mild colitis: 20% Moderate colitis: 71% Severe colitis: 9% Acute disease complications
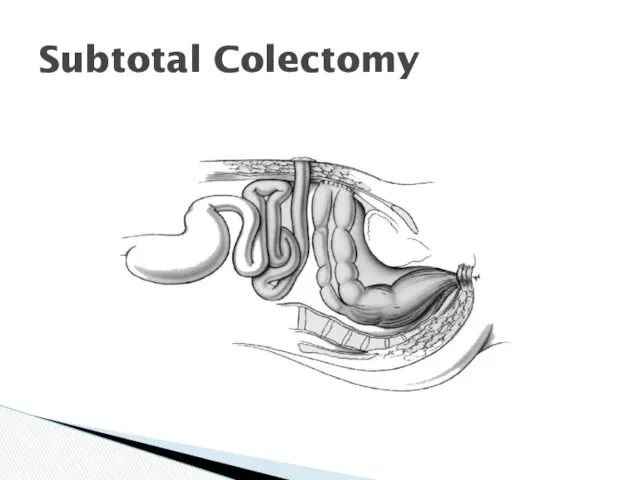
- 58. Subtotal Colectomy
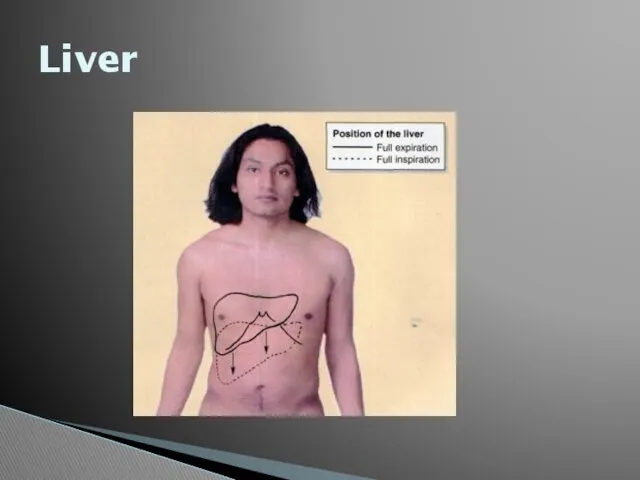
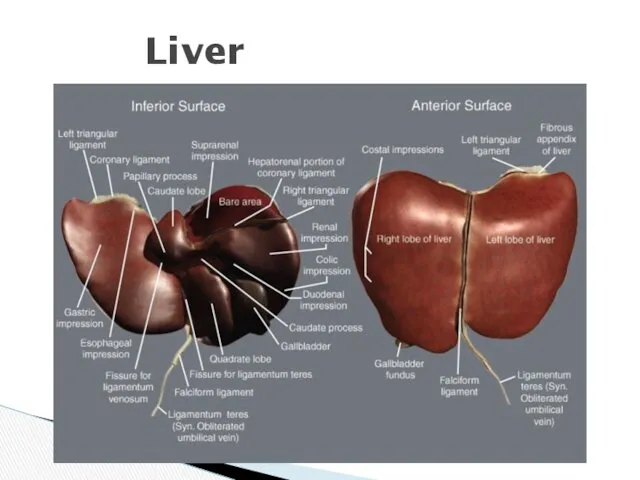
- 59. Liver
- 60. Liver
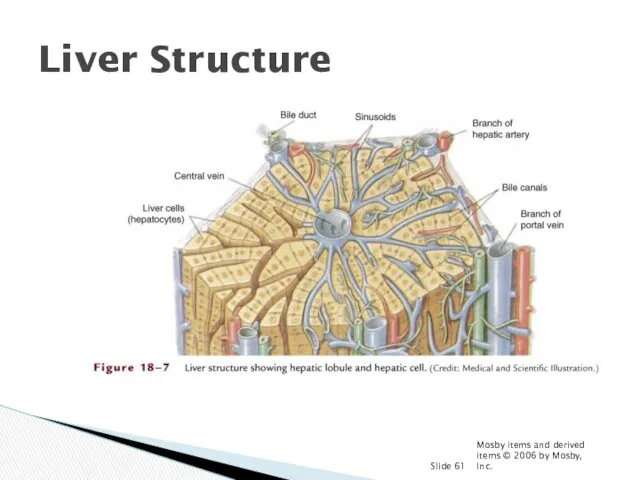
- 61. Mosby items and derived items © 2006 by Mosby, Inc. Slide Liver Structure
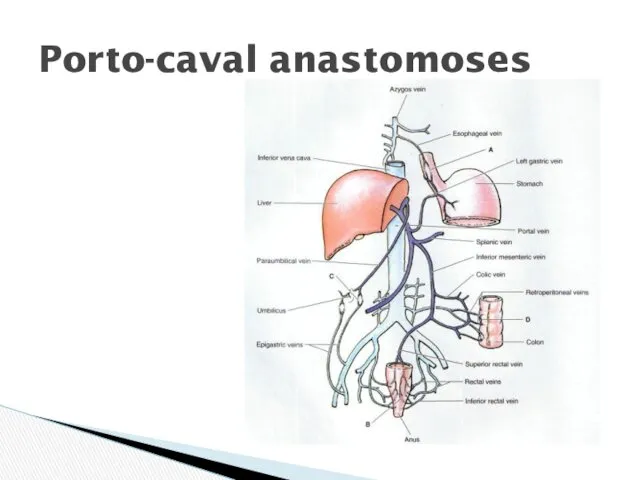
- 62. Porto-caval anastomoses
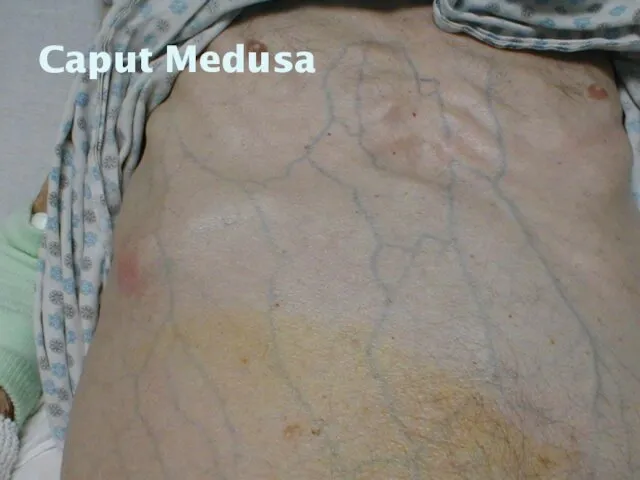
- 63. Caput Medusa
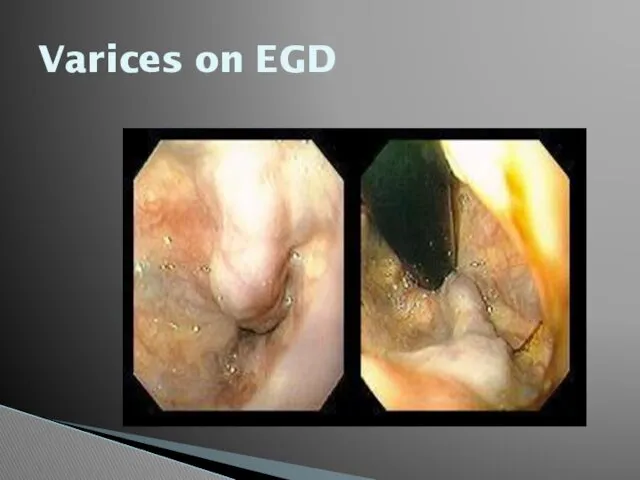
- 65. Varices on EGD
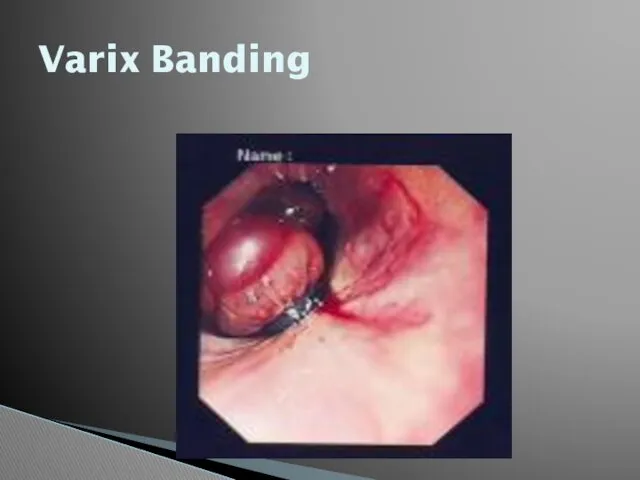
- 66. Varix Banding
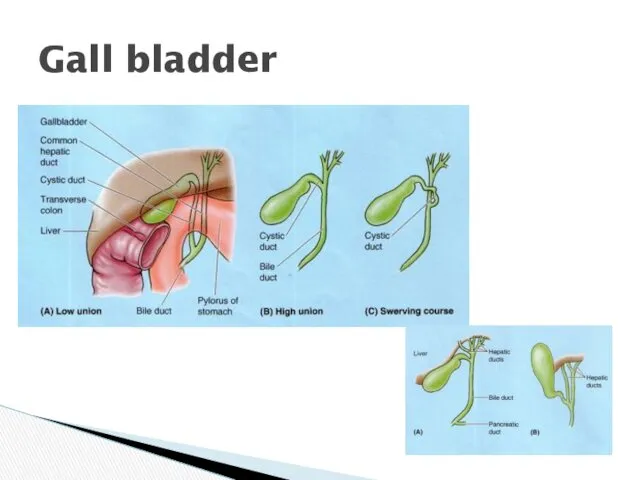
- 67. Gall bladder
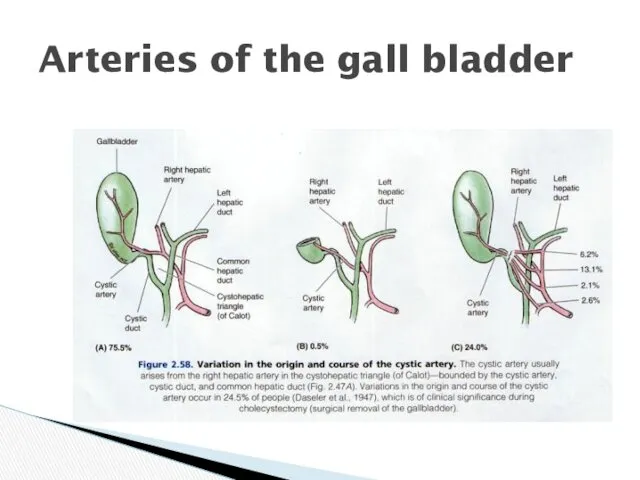
- 68. Arteries of the gall bladder
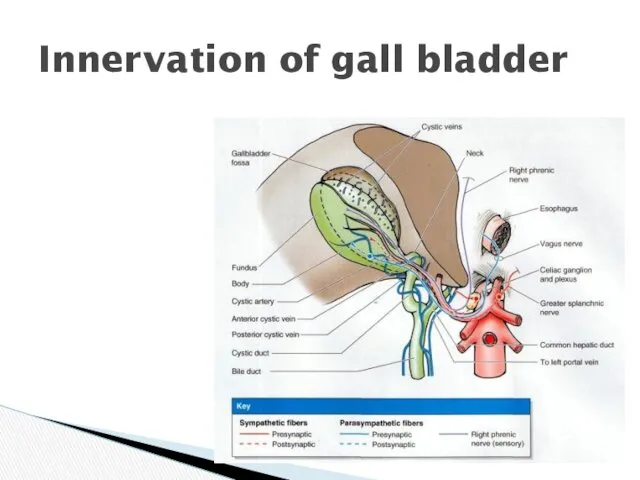
- 69. Innervation of gall bladder
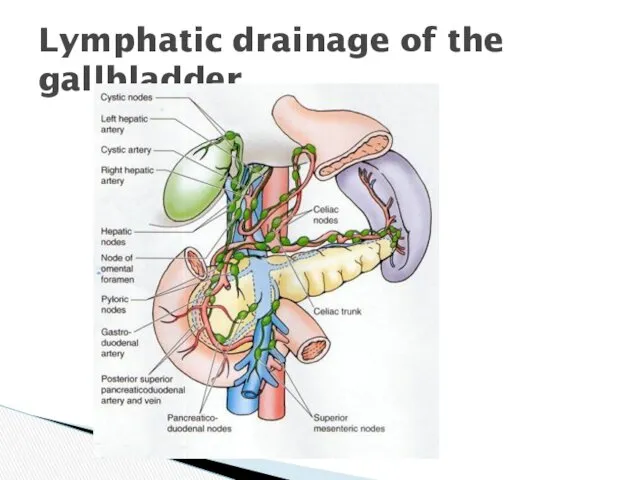
- 70. Lymphatic drainage of the gallbladder
- 71. Harvest Time
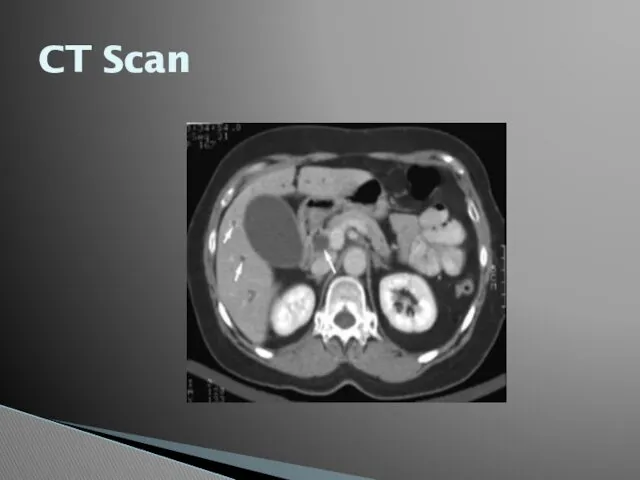
- 72. CT Scan
- 73. Plain Films
- 74. Ultrasound
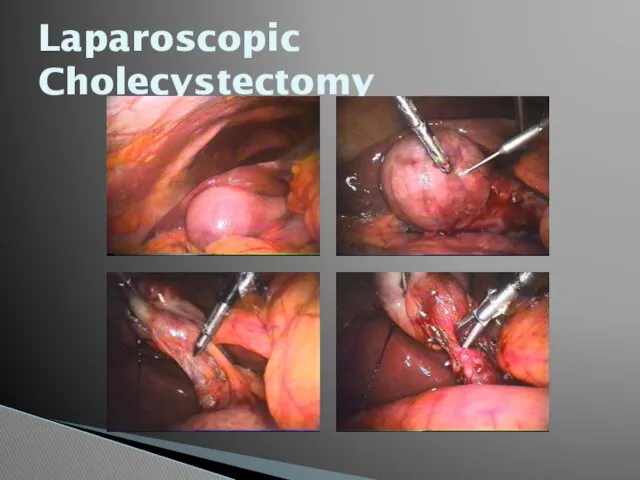
- 75. Laparoscopic Cholecystectomy
- 76. cancer
- 78. Скачать презентацию







 Туберкулез животных
Туберкулез животных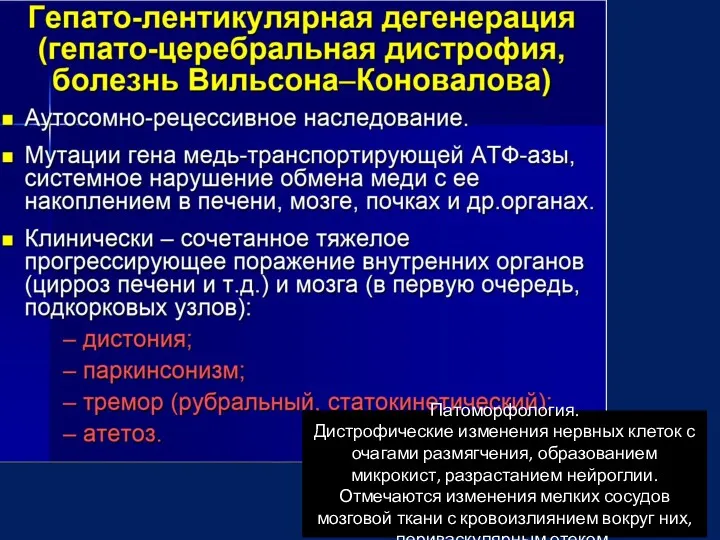 Гепато-лентикулярная дегенерация (гепато-церебральная дистрофия, болезнь Вильсона-Коновалова)
Гепато-лентикулярная дегенерация (гепато-церебральная дистрофия, болезнь Вильсона-Коновалова) Группы крови.. Иммунитет
Группы крови.. Иммунитет Ультразвуковая диапевтика в урологии
Ультразвуковая диапевтика в урологии Равновесные процессы в контроле качества фармацевтической субстанции Silver Nitrate
Равновесные процессы в контроле качества фармацевтической субстанции Silver Nitrate Дивертикулярная болезнь ободочной кишки у пожилых
Дивертикулярная болезнь ободочной кишки у пожилых Презентация ООИБ-ПНД
Презентация ООИБ-ПНД Болезни склеры. Клиника, диагностика, лечение
Болезни склеры. Клиника, диагностика, лечение Basic first aid
Basic first aid Профилактика заболеваний, передающихся половым путем
Профилактика заболеваний, передающихся половым путем Вплив тютюнопаління, алкоголю, наркотиків і токсинів на нервову систему та поведінку людини
Вплив тютюнопаління, алкоголю, наркотиків і токсинів на нервову систему та поведінку людини Женская и мужская стерилизация
Женская и мужская стерилизация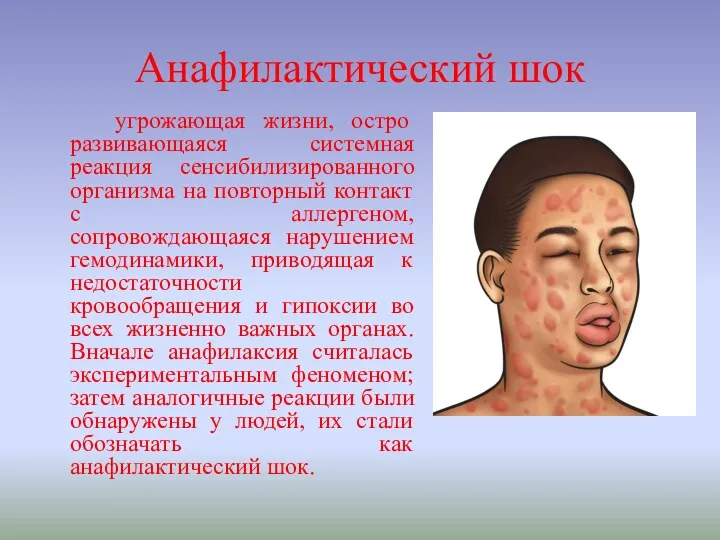 Анафилактический шок
Анафилактический шок Неотложная помощь при гипертоническом кризе, обмороке, коллапсе, шоке у детей
Неотложная помощь при гипертоническом кризе, обмороке, коллапсе, шоке у детей Бауыр эхинококкозы
Бауыр эхинококкозы Применение лекарственных средств, используемых в иммунологии у беременных, в период лактации
Применение лекарственных средств, используемых в иммунологии у беременных, в период лактации Қартаюдың биологиялық,медициналық аспектілері. Қартаю теориялары
Қартаюдың биологиялық,медициналық аспектілері. Қартаю теориялары Паразитарные заболевания печени
Паразитарные заболевания печени Организация питания в ДОУ
Организация питания в ДОУ Строение и развитие периферических органов эндокринной системы
Строение и развитие периферических органов эндокринной системы Изготовление лекарственной формы по прописи, используя теоретические знания в соответствии с требованиями нд
Изготовление лекарственной формы по прописи, используя теоретические знания в соответствии с требованиями нд Ревматоидный артрит
Ревматоидный артрит Тіс анатомиясы
Тіс анатомиясы Особенности косметических средств и процедуры салонного ухода за жирной кожей
Особенности косметических средств и процедуры салонного ухода за жирной кожей Воспаление. Этиология воспаления
Воспаление. Этиология воспаления Ишемическая болезнь сердца. Клинические, лабораторные и инструментальные особенности
Ишемическая болезнь сердца. Клинические, лабораторные и инструментальные особенности Рентгеноанатомия опорно-двигательного аппарата
Рентгеноанатомия опорно-двигательного аппарата Нервная регуляция
Нервная регуляция