Содержание
- 2. Plan of the lecture 1. Definition, etiologic factors, diagnostics, treatment of urticaria and allergic edema 2.
- 3. Urticaria – is a disease manifested by itching skin rash like spots, papule, vesicle with clear
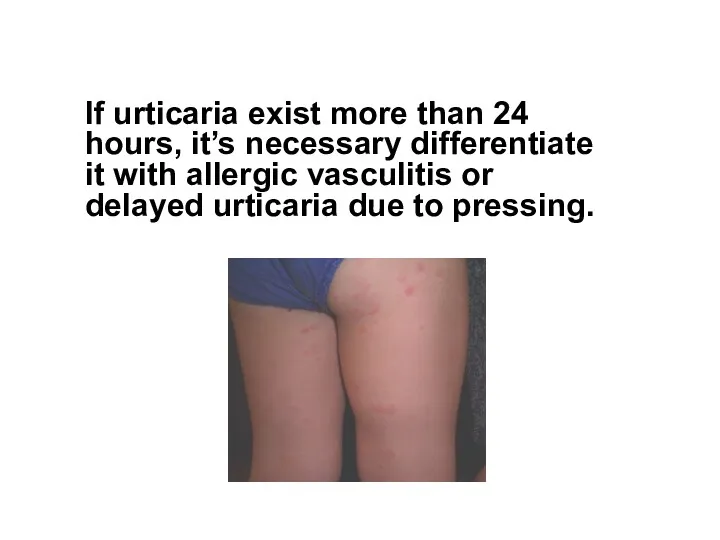
- 4. If urticaria exist more than 24 hours, it’s necessary differentiate it with allergic vasculitis or delayed
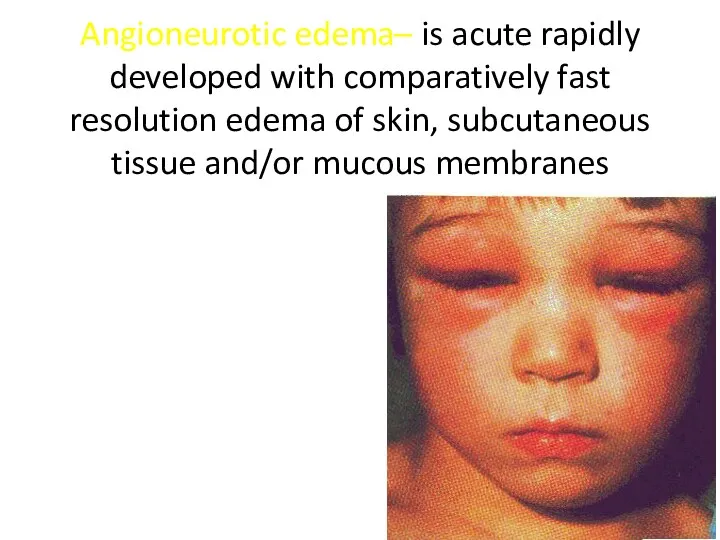
- 5. Angioneurotic edema– is acute rapidly developed with comparatively fast resolution edema of skin, subcutaneous tissue and/or
- 6. Etiologic factors of urticaria (U) and allergic edema (AE) are: IgE-mediated factors Food or injected allergens
- 7. Substances of direct action on mastocytes opiates Contrast remedies for X-ray curare, tobaccocurine chloride Substances that
- 8. Autoimmune disease of mastocytes IgG- antibodies IgE IgG- antibodies against Fc ( highly adapted receptor for
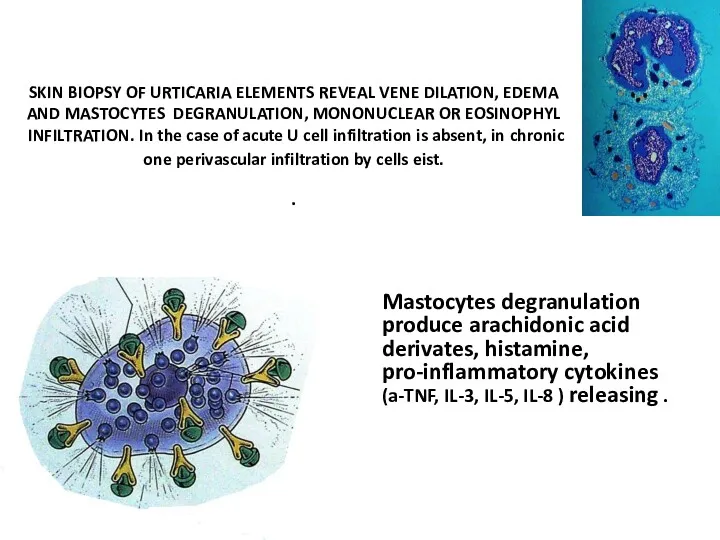
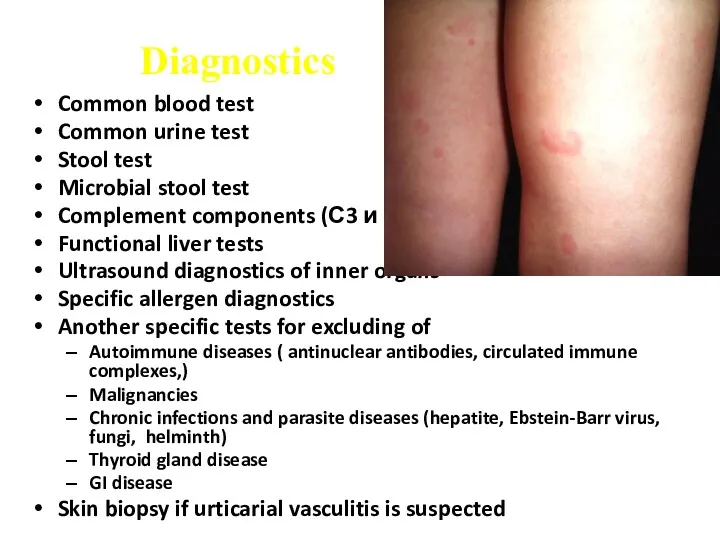
- 9. SKIN BIOPSY OF URTICARIA ELEMENTS REVEAL VENE DILATION, EDEMA AND MASTOCYTES DEGRANULATION, MONONUCLEAR OR EOSINOPHYL INFILTRATION.
- 10. Diagnostics Common blood test Common urine test Stool test Microbial stool test Complement components (С3 и
- 11. Treatment Main goal is acute urticaria complete resolution and choice of proper therapy Hospitalization indications– severe
- 12. Medications Antihistamine drugs Н1-blockers of 1, 2 and 3 generation Corticosteroids: prednisone 2-3-5 mg/кg Sorbents
- 13. Layel syndrome (toxic- allergic bullous epidermal necrolysis) The most severe form of allergic skin disorders More
- 14. Clinical presentation Disease develops several hours or days later medication intake Prodromal period presents with fever,
- 15. Positive Nickolsky sumptom Very painful erosions and affected sites of skin Progressive condition worsening, dehydration symptoms
- 17. Treatment In emergency department The main task is sustain normal fluid-electrolite and protein balance, topical therapy
- 18. Stevens-Jones syndrome The most severe form of polymorphic exudative erythema with affection of mucous membrains together
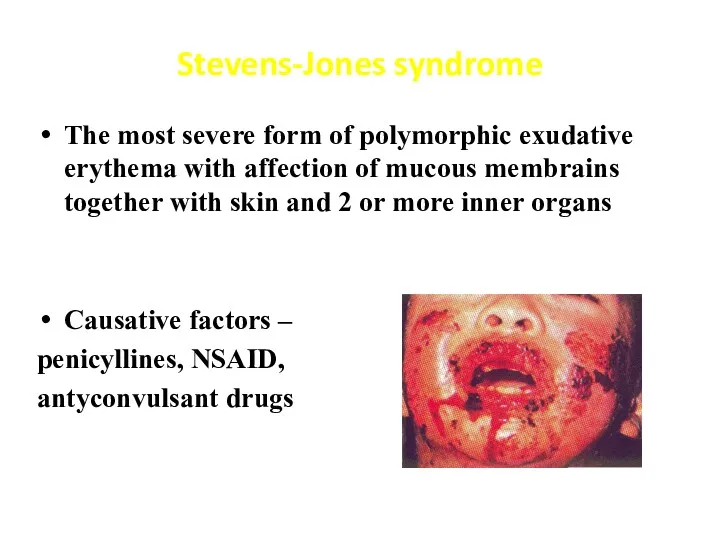
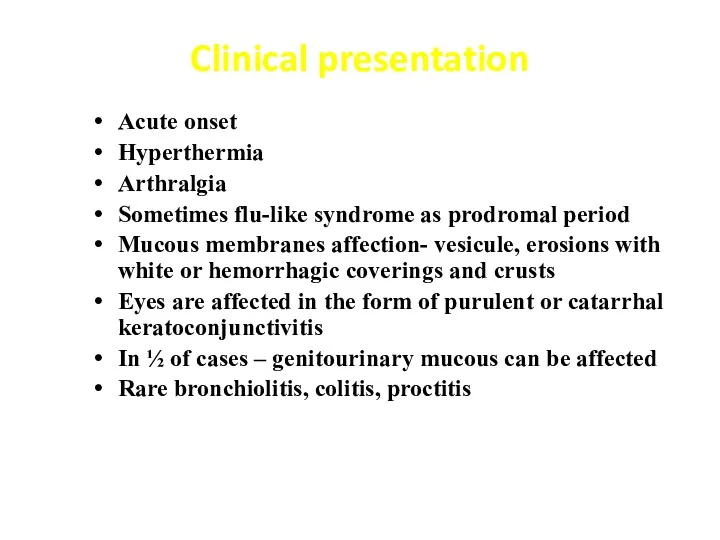
- 19. Clinical presentation Acute onset Hyperthermia Arthralgia Sometimes flu-like syndrome as prodromal period Mucous membranes affection- vesicule,
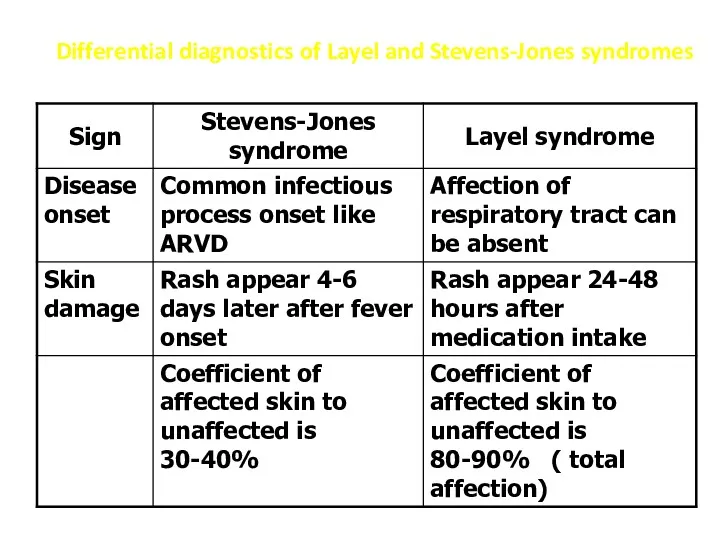
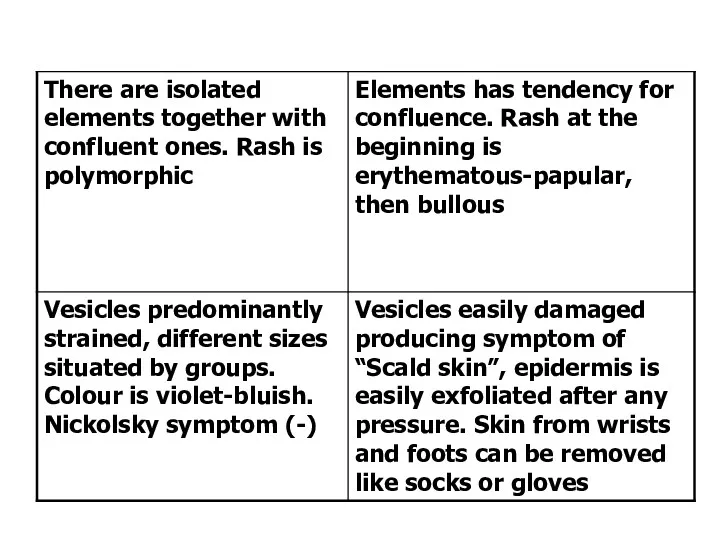
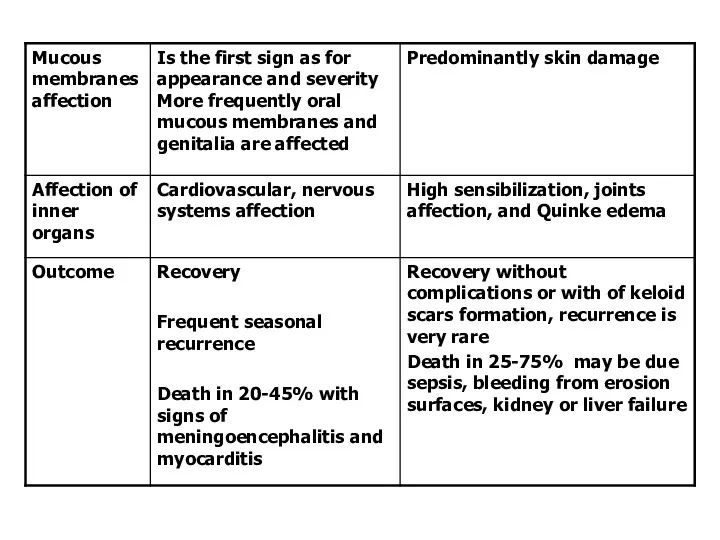
- 20. Differential diagnostics of Layel and Stevens-Jones syndromes
- 23. Serum disease Serum disease is allergic disease caused by heterogeneous or homogeneous serum or medications injections
- 24. Predominantly immune complex mechanisms are responsible for inflammatory process in vessels and connective tissue Main serum
- 25. Clinical signs Different symptoms due to difference of antibodies types and quantities Incubative period after initial
- 26. Acute period: fever , hyperthermia to 39-40С; polyarthralgia, articular stiffness Rash like urticaria or maculo-papular type,
- 27. Anaphylactic shock Asphyxia Circulatory Abdominal Cerebral Mixed Course Acute benign Acute malignant Lingering Recurrent Abortive
- 28. Emergency Stop medication injection Lay down patient, turn his head to the side, pull mandibular forward,
- 29. In the case of parenteral allergen penetration: to inject the site of allergen injection ( or
- 30. If anaphylactic reaction is due to instillation into nose or eyes it’s necessary wash out mucous
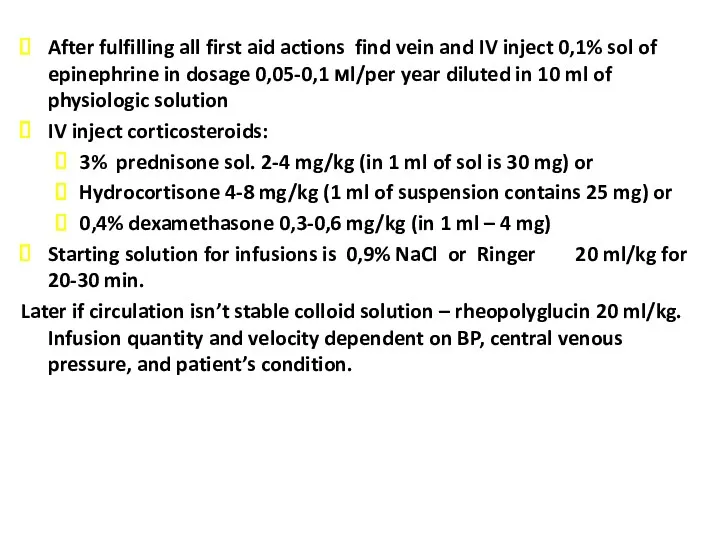
- 31. After fulfilling all first aid actions find vein and IV inject 0,1% sol of epinephrine in
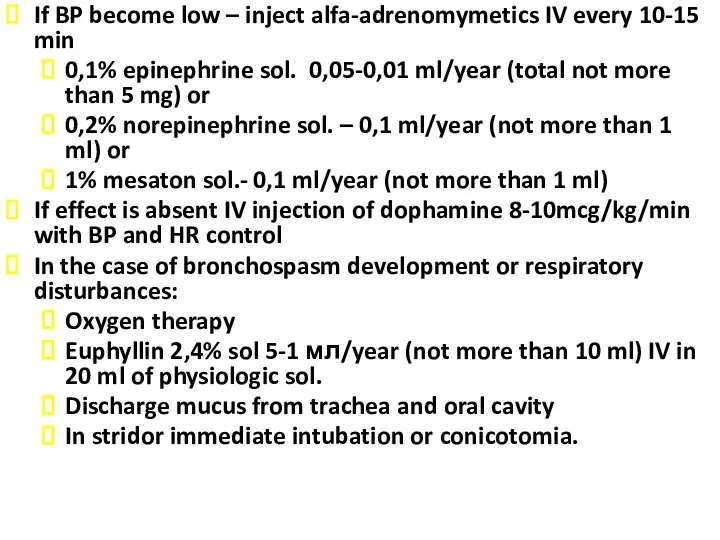
- 32. If BP become low – inject alfa-adrenomymetics IV every 10-15 min 0,1% epinephrine sol. 0,05-0,01 ml/year
- 33. If necessary provide cardio-pulmonary emergency rehabilitation Symptomatic treatment Hospitalization after providing all emergencies Elimination of acute
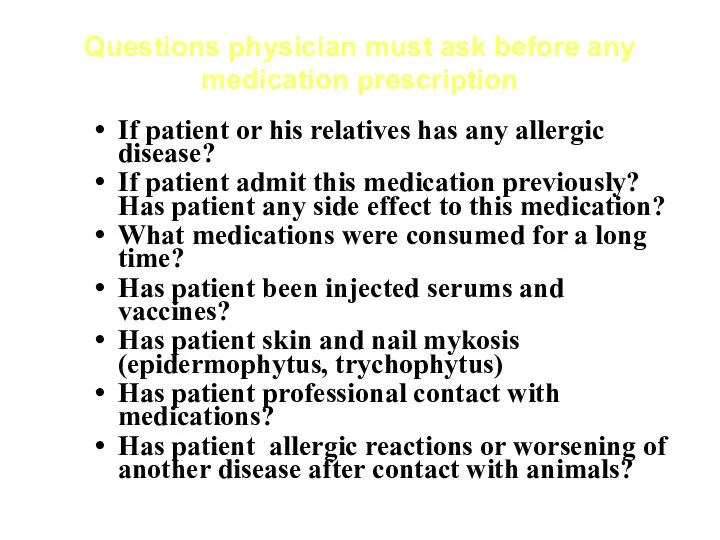
- 34. Questions physician must ask before any medication prescription If patient or his relatives has any allergic
- 35. Main approach for medication allergy Hypoallergic diet, parenteral feeding Stop intake of all medications ( leave
- 36. Medication allergy prevention Before prescribing any medication doctor must answer to questions : if really this
- 37. Primary prophylaxis of medication allergy: Avoid polypragmasia, medication doses must be correct for age and weight,
- 39. Скачать презентацию

 Эндокринная система
Эндокринная система Кандидозы
Кандидозы Остеоартроз (остеоартрит)
Остеоартроз (остеоартрит) Пневмокониозы
Пневмокониозы Травма живота
Травма живота Променева діагностика невідкладних станів
Променева діагностика невідкладних станів Учебная практика. Санитарные правила и нормы, применяемые при оказании услуг по коррекции бровей и окрашивании бровей и ресниц
Учебная практика. Санитарные правила и нормы, применяемые при оказании услуг по коррекции бровей и окрашивании бровей и ресниц Твердые лекарственные формы. Общая рецептура
Твердые лекарственные формы. Общая рецептура Лучевая диагностика болезни Ходжкина. Лимфагранулематоз
Лучевая диагностика болезни Ходжкина. Лимфагранулематоз Заманауи контрацепциямен өзіңді тап
Заманауи контрацепциямен өзіңді тап Тәуліктік PH-метрия
Тәуліктік PH-метрия Группа лекарственных средств антациды
Группа лекарственных средств антациды Предварительные и периодические медицинские осмотры работников
Предварительные и периодические медицинские осмотры работников Клинико-психологическая характеристика акалькулии
Клинико-психологическая характеристика акалькулии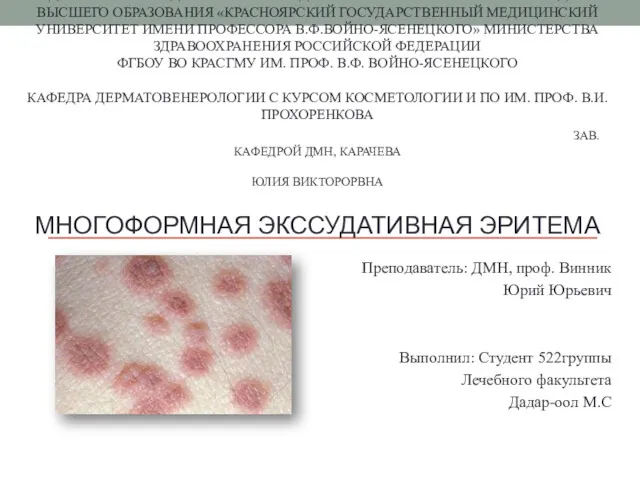 Многоформная экссудативная эритема
Многоформная экссудативная эритема Гепатиты. Хронический вирусный гепатит
Гепатиты. Хронический вирусный гепатит Acute myeloid leukemia
Acute myeloid leukemia Миславский А.А (1828-1914)
Миславский А.А (1828-1914) Этико-правовые проблемы наркологии и психиатрии
Этико-правовые проблемы наркологии и психиатрии Наследственные болезни обмена веществ: клиника, диагностика, лечение
Наследственные болезни обмена веществ: клиника, диагностика, лечение Блокируемый интрамедуллярный остеосинтез (БИОС)
Блокируемый интрамедуллярный остеосинтез (БИОС) Спинной мозг. Кровоснабжение, ликвородинамика
Спинной мозг. Кровоснабжение, ликвородинамика Экзогенный аллергический альвеолит
Экзогенный аллергический альвеолит Тұқым қуалайтын өзгергіштіктегі ұқсас қатарлар заңы
Тұқым қуалайтын өзгергіштіктегі ұқсас қатарлар заңы Обследование фонетико-фонематической стороны речи
Обследование фонетико-фонематической стороны речи Грипп. Что такое вирусы?
Грипп. Что такое вирусы? Мутагендік факторлар
Мутагендік факторлар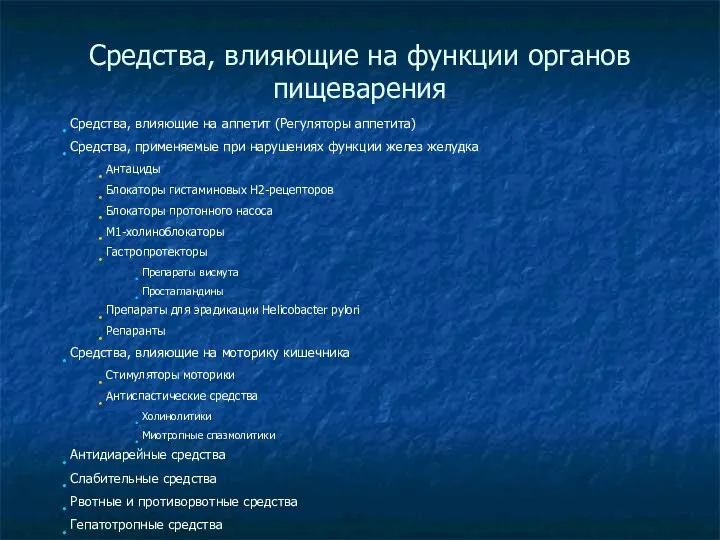 Средства, влияющие на функции органов пищеварения
Средства, влияющие на функции органов пищеварения