Содержание
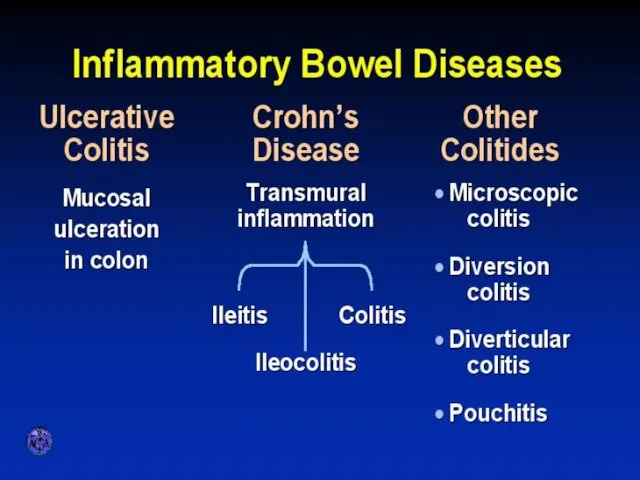
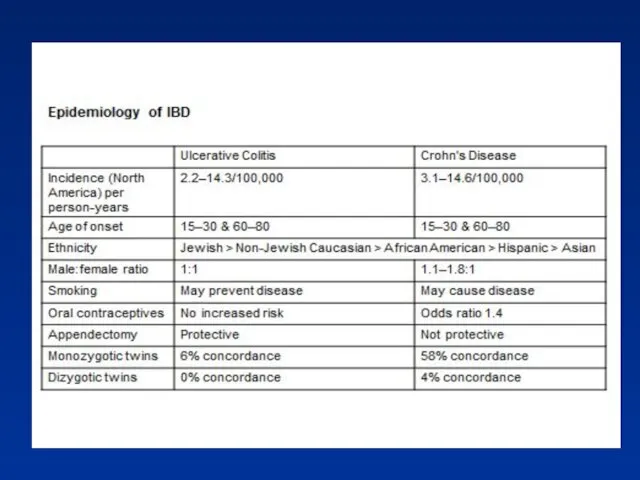
- 2. INFLAMMATORY BOWEL DISEASES
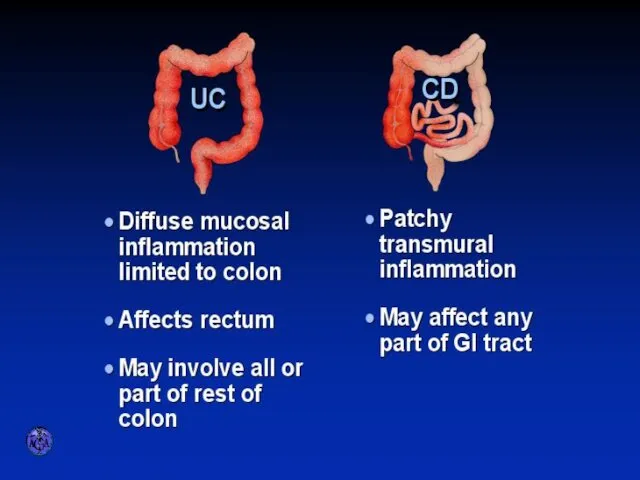
- 3. ULCERATIVE COLITIS AND CROHN’S DISEASE
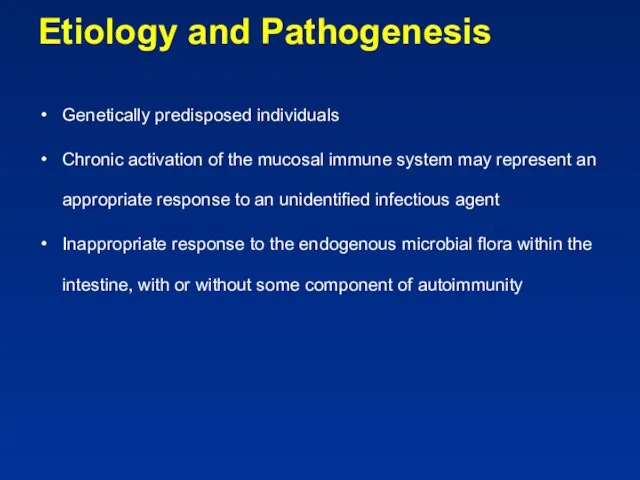
- 5. Etiology and Pathogenesis Genetically predisposed individuals Chronic activation of the mucosal immune system may represent an
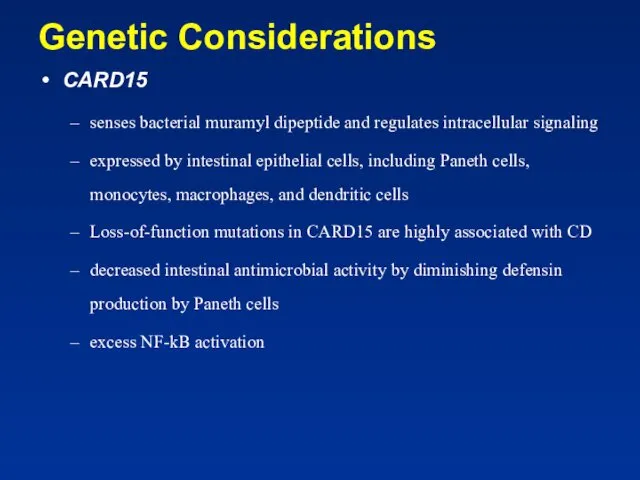
- 6. Genetic Considerations CARD15 senses bacterial muramyl dipeptide and regulates intracellular signaling expressed by intestinal epithelial cells,
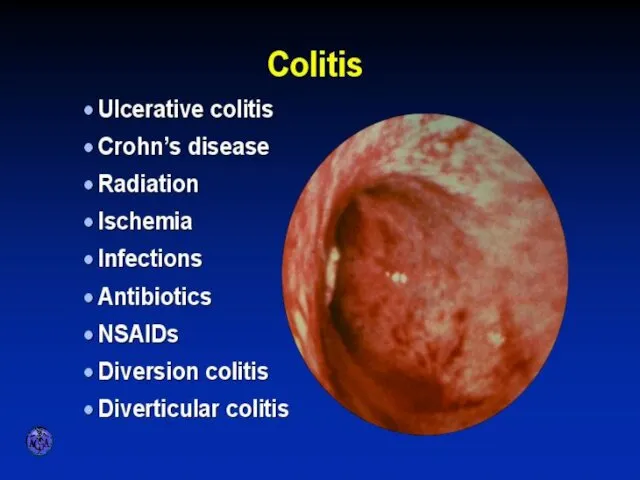
- 7. VARIETIES OF COLITIS
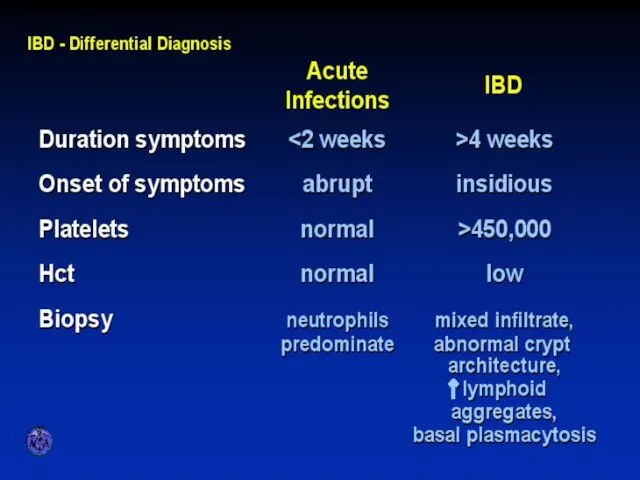
- 8. DIFFERENTIAL DIAGNOSIS OF INFECTIOUS AND ULCERATIVE COLITIS
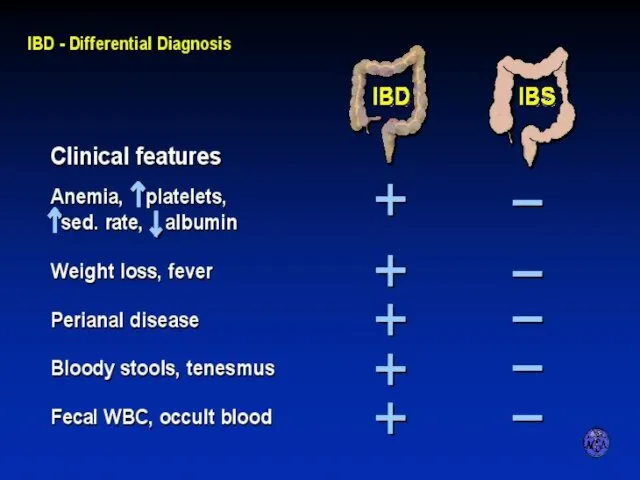
- 9. DIFFERENTIAL DIAGNOSIS OF IBD AND IBS
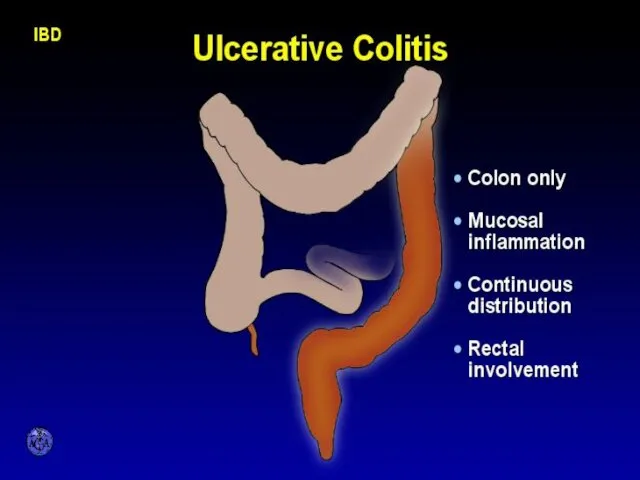
- 10. CHARACTERISTIC FEATURES OF ULCERATIVE COLITIS
- 11. Pathology Ulcerative Colitis: Macroscopic Features mucosal disease that usually involves the rectum and extends proximally to
- 12. UC Physical findings Abdomen: tenderness and distension, but can be normal Extra colonic: arthritis, skin changes
- 13. UC Laboratory findings No specific findings ESR ↑, CRP ↑, anemia (chronic disease, Fe↓), WBC ↑
- 14. UC Clinical Features Relapsing disease (~ 80% 1yr) Symptoms usually parallel disease extent (More disease→more systemic
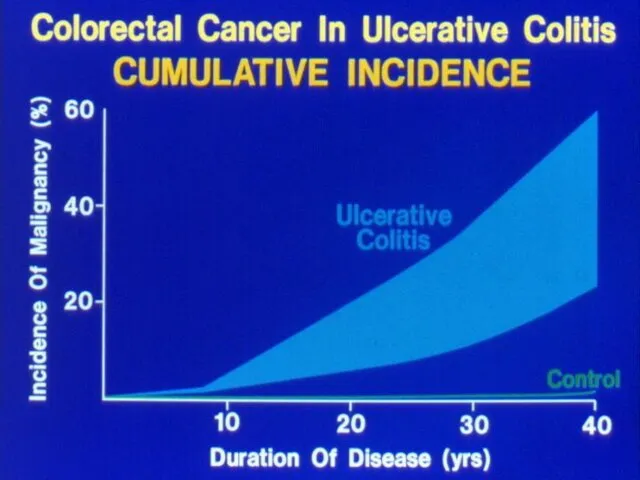
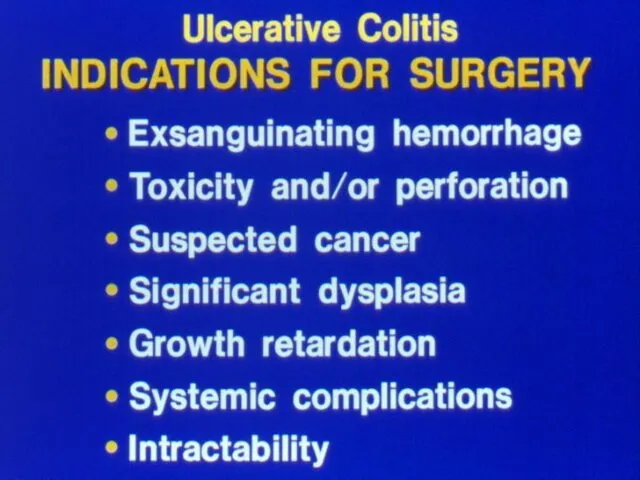
- 15. UC- Complications Bleeding Perforation Toxicity Cancer
- 17. Crohn’s disease (CD) Transmural disease, symptoms depend on site of involvement and complications Abdominal pain, diarrhea
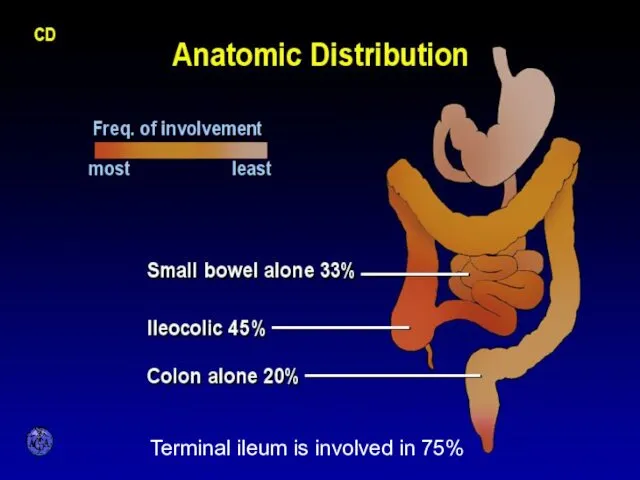
- 18. ANATOMIC DISTRIBUTION Terminal ileum is involved in 75%
- 19. CD Small bowel Abdominal pain (mainly RLQ), may be constant and dull, may be colicky (obstruction)
- 20. CD Colon Colon: diarrhea, less rectal bleeding (less colon & rectum involved), characteristic rectal sparing. Perianal
- 21. CD Perianal Disease Fissures Fistulas Perirectal abscess
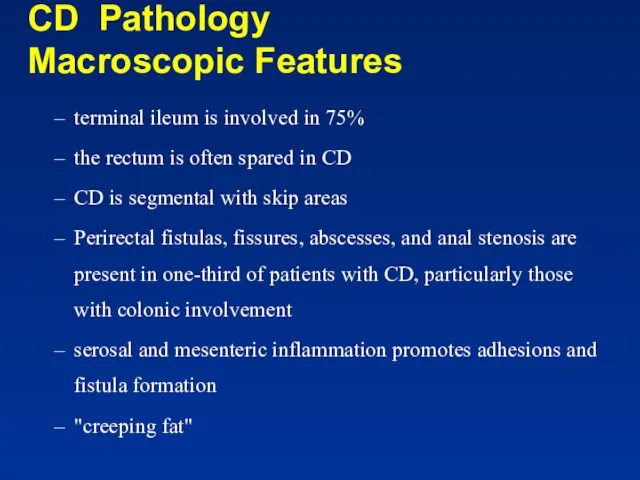
- 22. CD Pathology Macroscopic Features terminal ileum is involved in 75% the rectum is often spared in
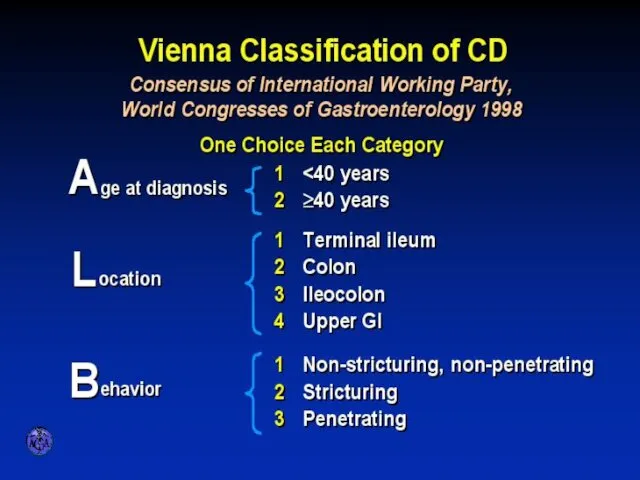
- 23. VIENNA CLASSIFICATION
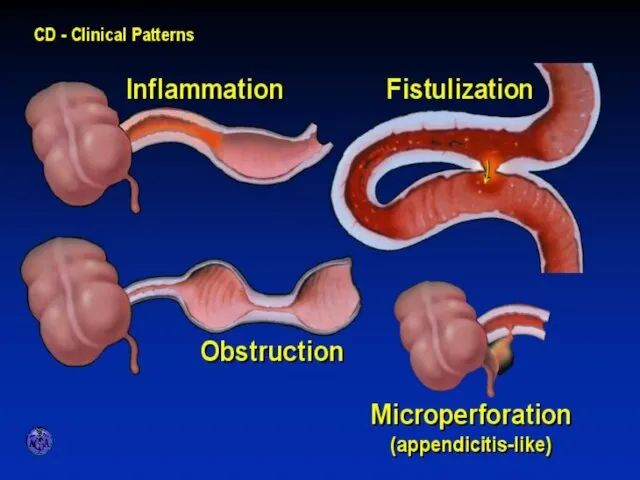
- 24. CLINICAL PATTERNS
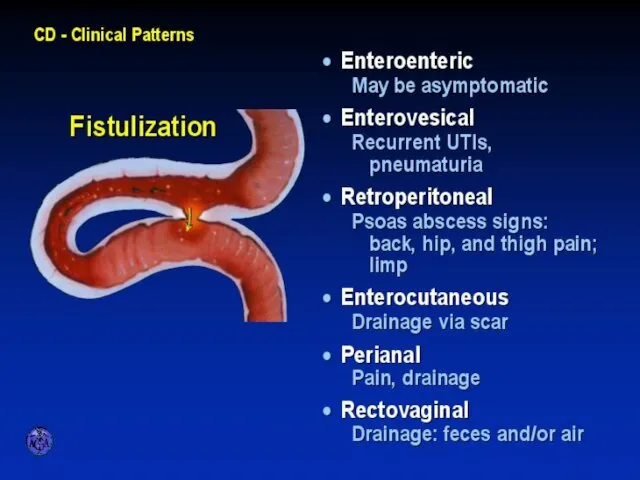
- 25. FISTULIZATION
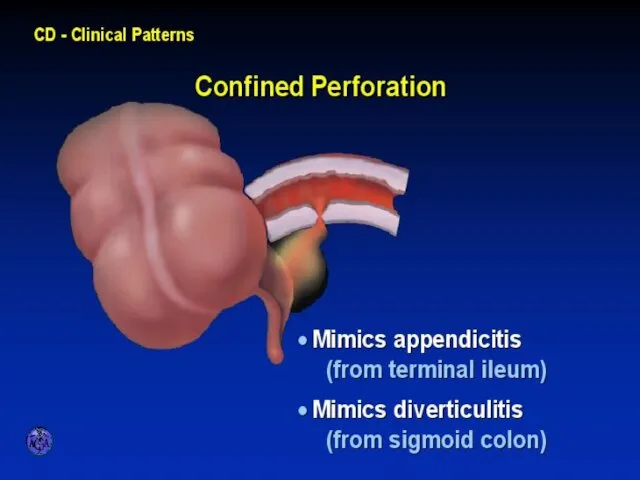
- 26. CONFINED PERFORATION
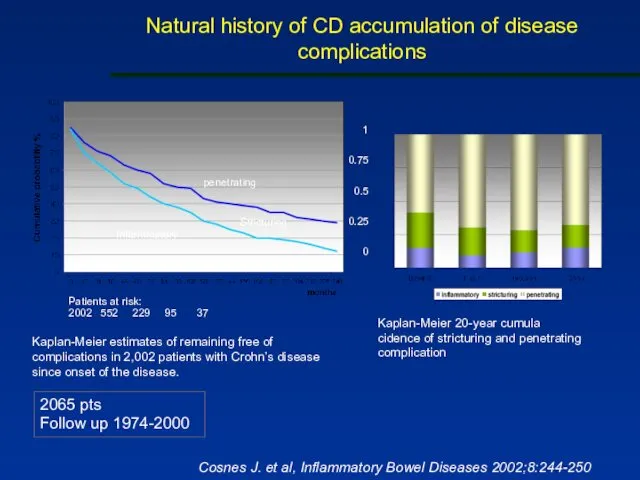
- 27. Natural history of CD accumulation of disease complications 2065 pts Follow up 1974-2000 Kaplan-Meier estimates of
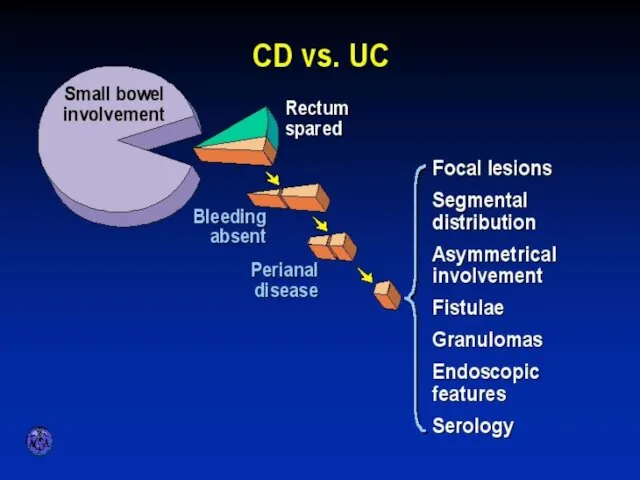
- 28. APPROACH TO DIFFERENTIAL DIAGNOSIS OF ULCERATIVE VERSUS CROHN’S COLITITS
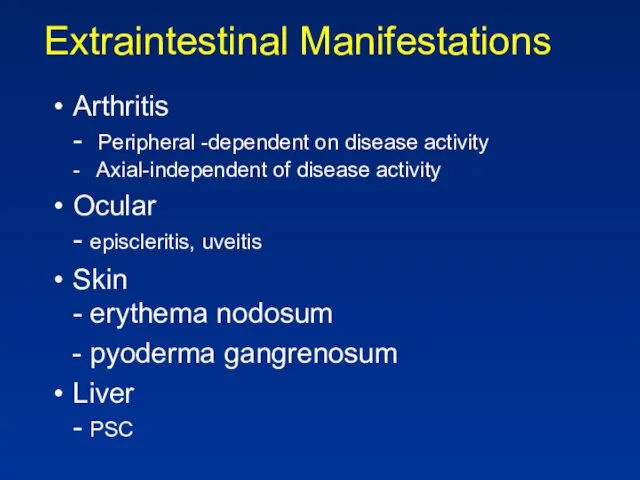
- 29. Extraintestinal Manifestations Arthritis - Peripheral -dependent on disease activity - Axial-independent of disease activity Ocular -
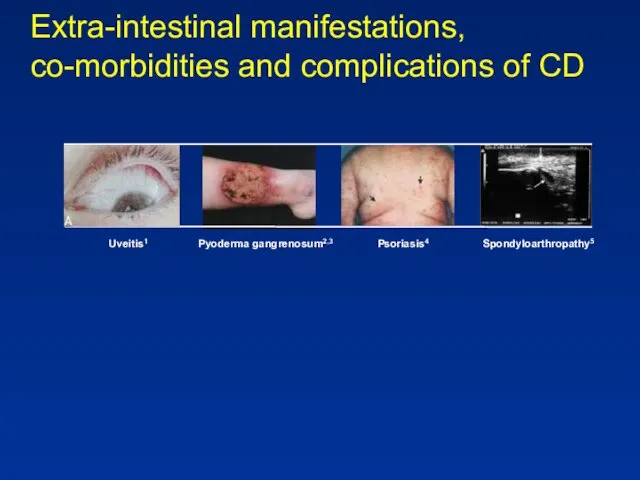
- 30. Extra-intestinal manifestations, co-morbidities and complications of CD Uveitis1 Pyoderma gangrenosum2,3 Psoriasis4 Spondyloarthropathy5
- 31. Extraintestinal Manifestations Rheumatologic Peripheral arthritis- 15–20% of IBD patients more common in CD worsens with exacerbations
- 32. Extraintestinal Manifestations Rheumatologic Sacroilitis Symmetric equally in UC and CD often asymptomatic does not correlate with
- 33. Extraintestinal manifestations - Skin Pyoderma gangrenosum- more in UC patients may occur years before the onset
- 35. Extraintestinal Manifestations - Skin - Erythema nodosum (15% of CD patients and 10% of UC patients)
- 36. Erythema nodosum
- 37. Extraintestinal Manifestations Ocular: The most common are conjunctivitis, anterior uveitis/iritis, and episcleritis Uveitis is associated with
- 38. Extraintestinal Manifestations Urologic calculi, ureteral obstruction, and fistulas nephrolithiasis (10–20%) occurs in patients with CD hyperoxaluria
- 39. Extraintestinal Manifestations Thromboembolic Disorders increased risk of both venous and arterial thrombosis Other Disorders cardiopulmonary manifestations:
- 40. Diagnosis History - How long? - How bad: no. of stools? Blood? Signs of rectal involvement
- 41. Diagnosis Laboratory tests- non specific and reflect disease severity & involvement Anemia- normocytic normochromic (chronic disease),
- 42. Diagnosis Stool: Steatorrhea (mild), WBC in stool, Increased calprotectin Disturbed Liver function tests (Alk. P- PSC,
- 43. Diagnosis Determine anatomic involvement Determine nature of involvement (UC Vs CD Vs others)
- 44. Diagnosis Endoscopic examinations: Rectosigmoidoscopy- rectum? Mucosal morphology? (ulcer type, skip areas) Colonoscopy- Same + disease extent
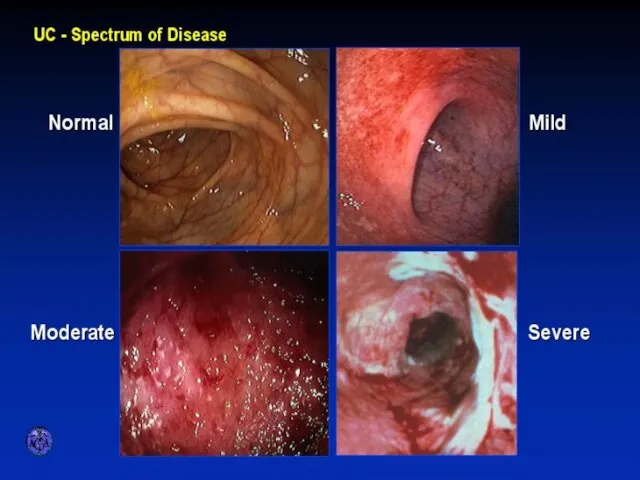
- 45. ENDOSCOPIC SPECTRUM OF SEVERITY
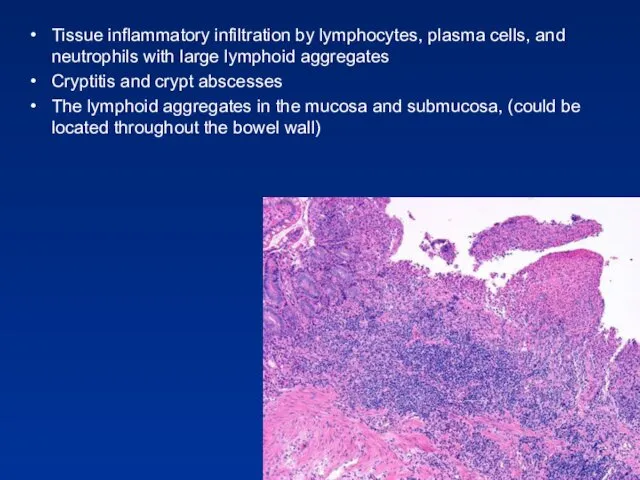
- 46. Tissue inflammatory infiltration by lymphocytes, plasma cells, and neutrophils with large lymphoid aggregates Cryptitis and crypt
- 47. ENDOSCOPIC APPEARANCES CD aphthae stellate ulcer longitudinal ulcer Macroulcerations and pseudoplyps
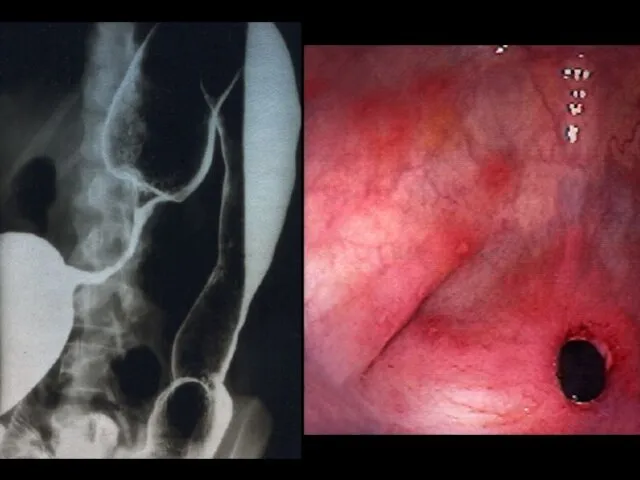
- 48. Diagnosis Radiology Barium enema: fistula, sinus tract, stricturing (not used today) Small bowel follow through- small
- 49. TRANSVERSE COLON STRICTURE
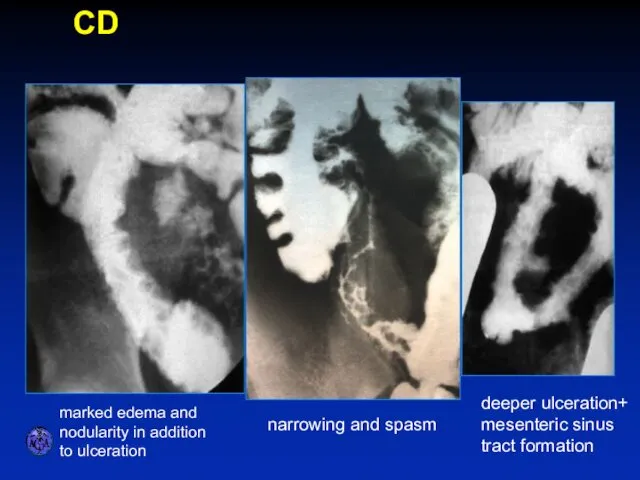
- 50. SPECTRUM OF ILEITIS marked edema and nodularity in addition to ulceration narrowing and spasm deeper ulceration+
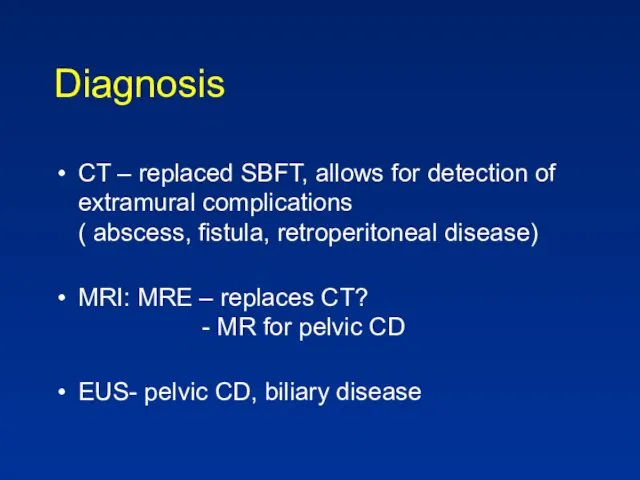
- 51. Diagnosis CT – replaced SBFT, allows for detection of extramural complications ( abscess, fistula, retroperitoneal disease)
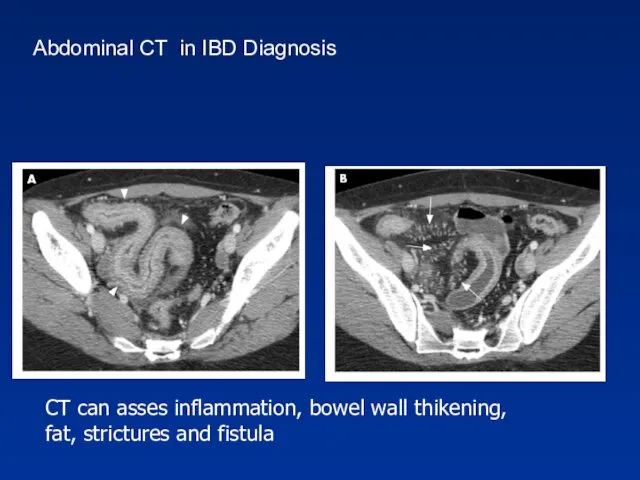
- 52. CT can asses inflammation, bowel wall thikening, fat, strictures and fistula Abdominal CT in IBD Diagnosis
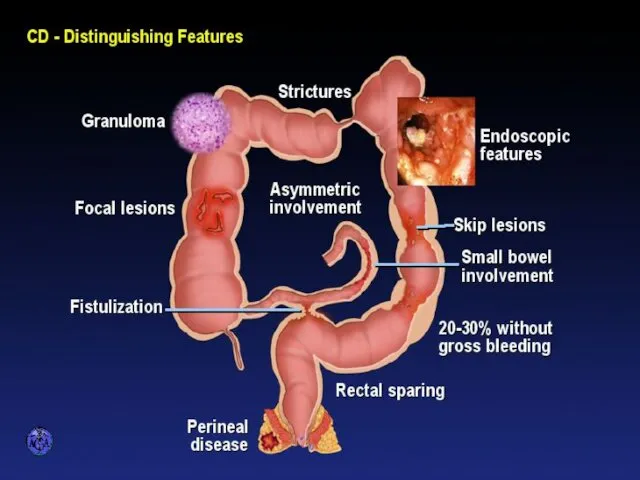
- 53. DISTINGUISHING FEATURES OF CROHN’S DISEASE
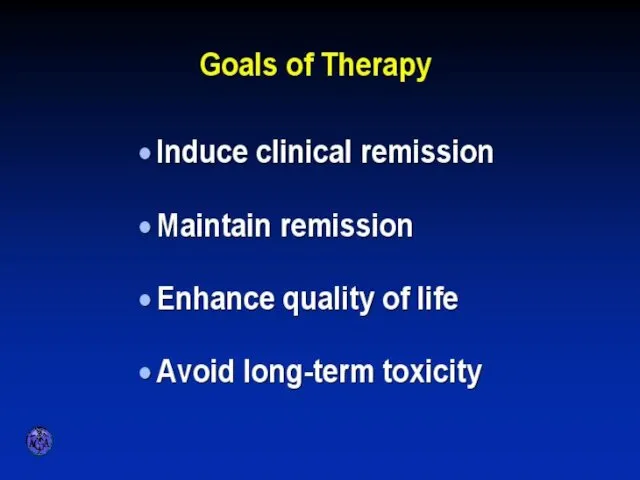
- 54. GOALS OF THERAPY
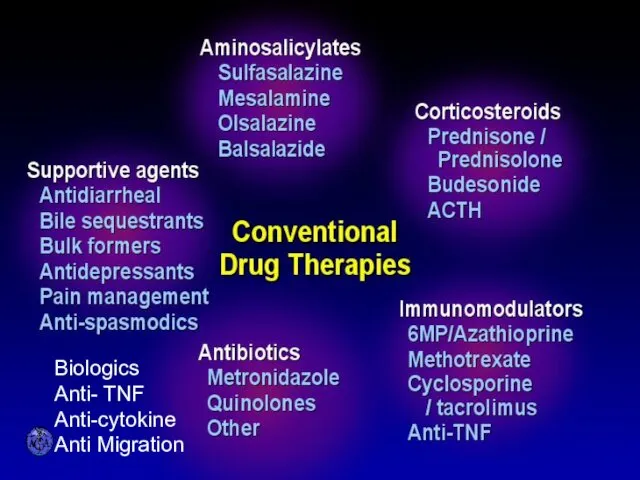
- 55. CONVENTIONAL DRUG THERAPIES Biologics Anti- TNF Anti-cytokine Anti Migration
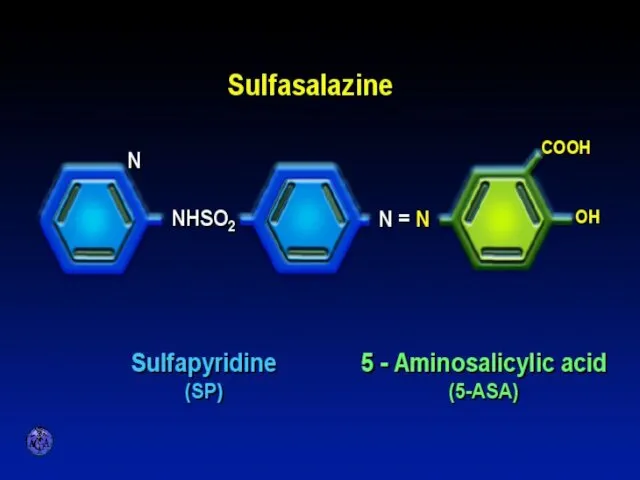
- 56. SULFASALAZINE
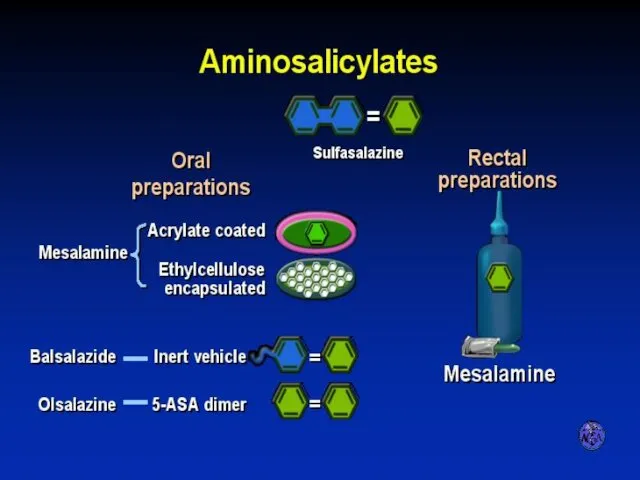
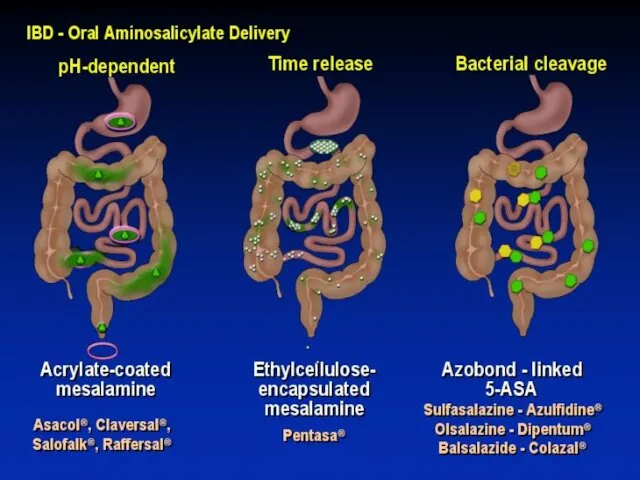
- 57. AMINOSALICYLATES
- 58. AMINOSALICYLATE DISTRIBUTION
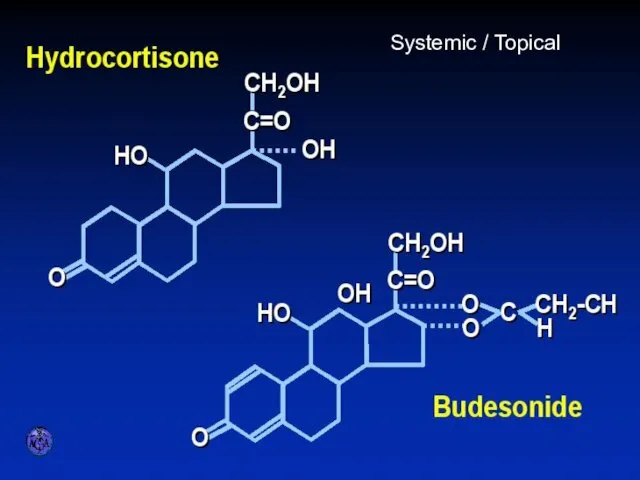
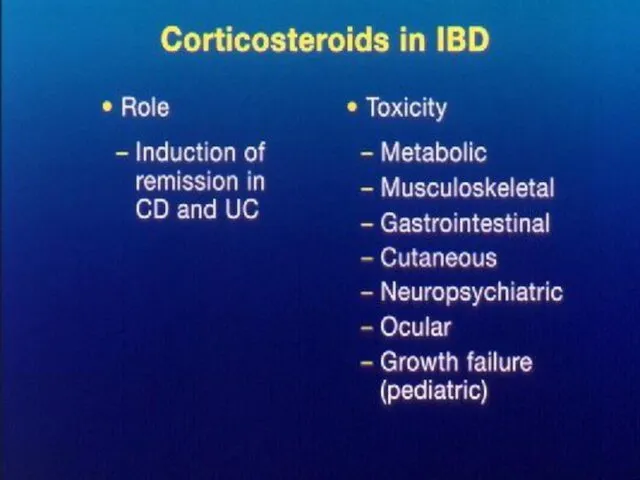
- 59. STEROID PREPARATIONS Systemic / Topical
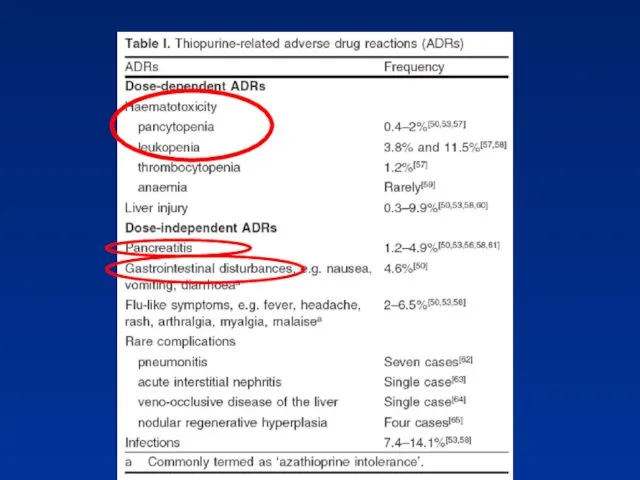
- 61. Immuno-suppressors in IBD Azathioprine, 6-Mercaptopurine Methotrexate Cyclosporin Tacrolimus
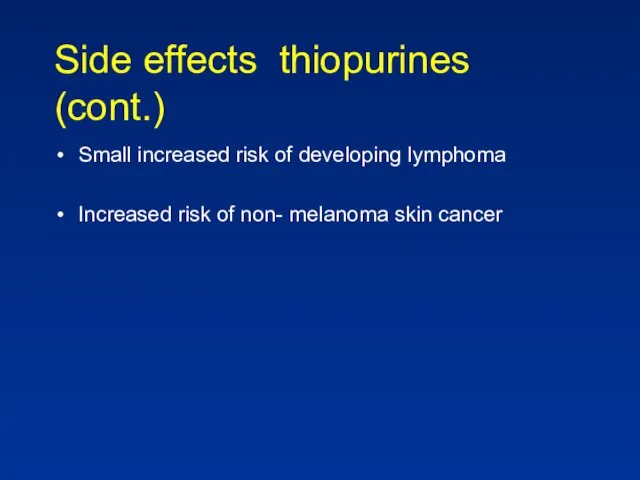
- 63. Side effects thiopurines (cont.) Small increased risk of developing lymphoma Increased risk of non- melanoma skin
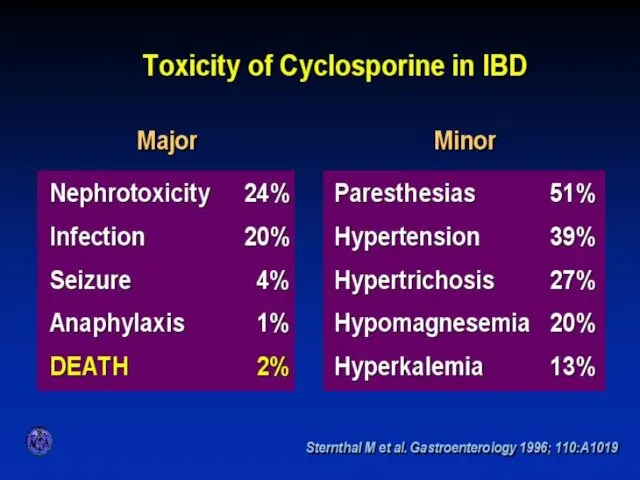
- 64. TOXICITY OF CYCLOSPORINE
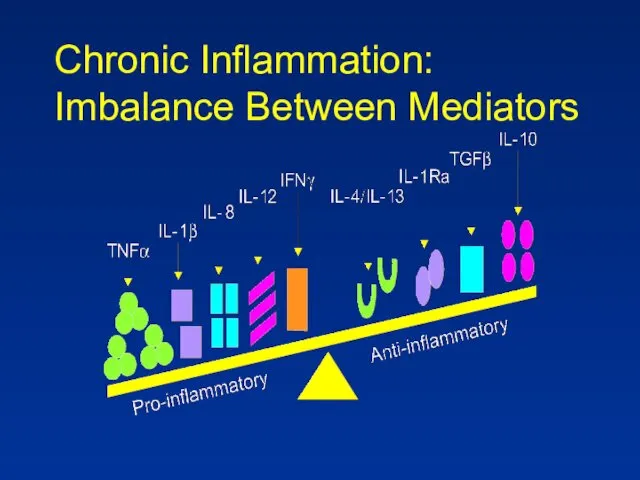
- 65. Chronic Inflammation: Imbalance Between Mediators
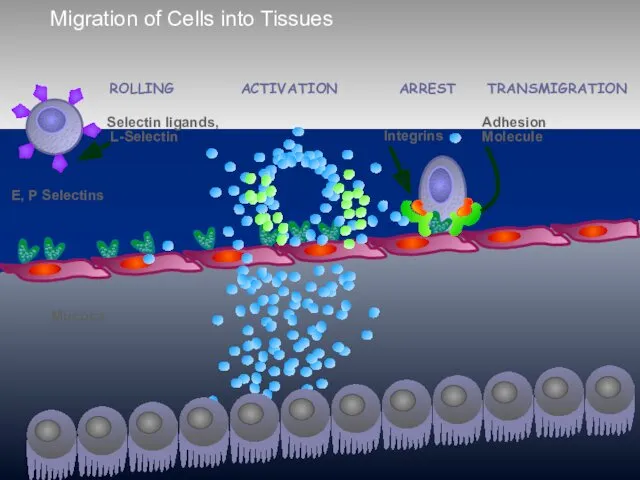
- 66. Migration of Cells into Tissues E, P Selectins Mucosa ACTIVATION ARREST ROLLING TRANSMIGRATION
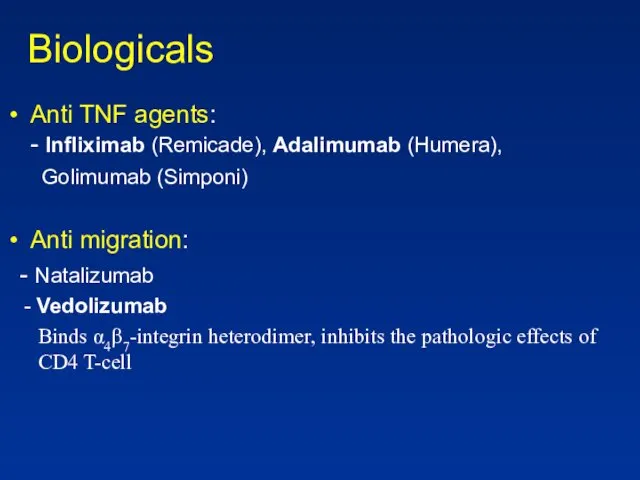
- 67. Biologicals Anti TNF agents: - Infliximab (Remicade), Adalimumab (Humera), Golimumab (Simponi) Anti migration: - Natalizumab -
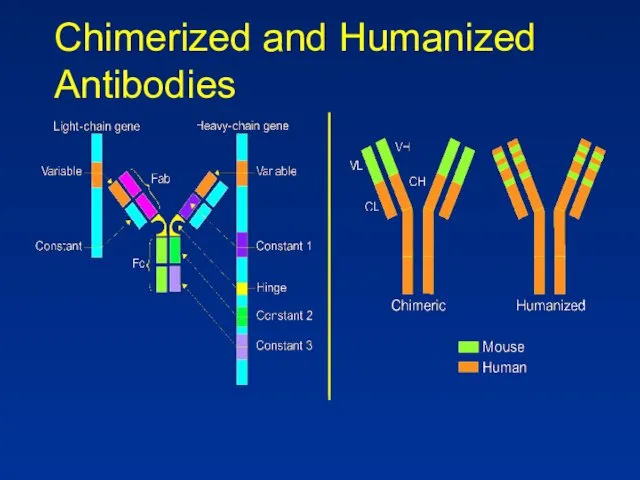
- 68. Chimerized and Humanized Antibodies
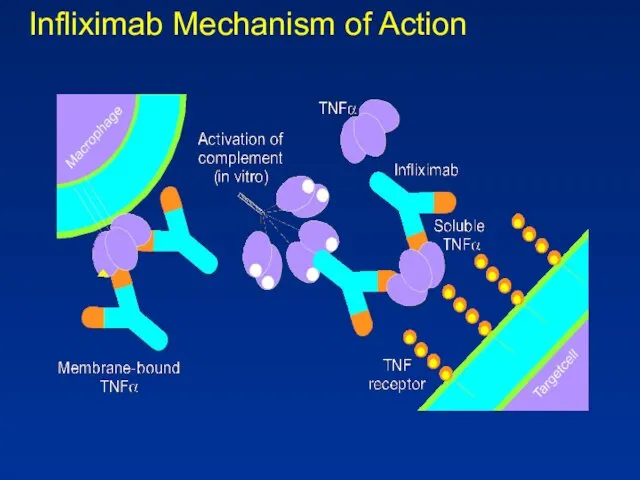
- 69. Infliximab Mechanism of Action
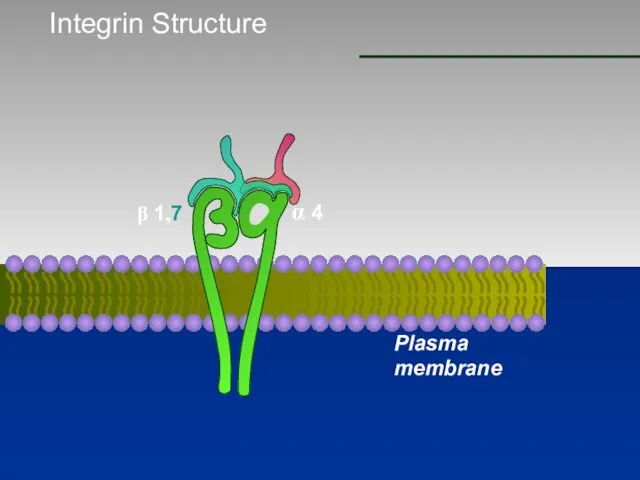
- 70. Integrin Structure β 1,7 α 4 Plasma membrane
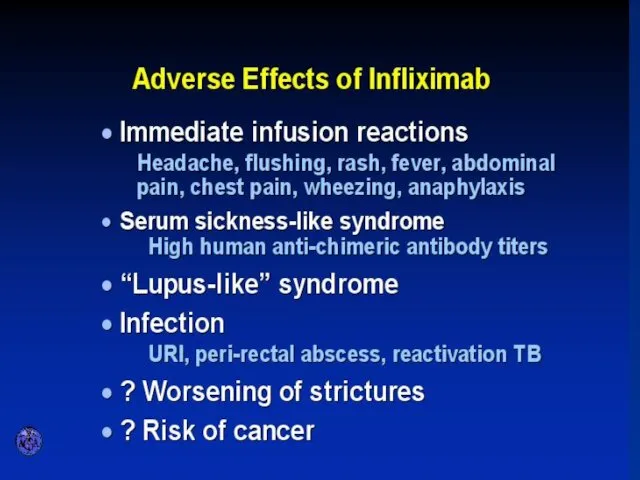
- 71. ADVERSE EFFECTS OF INFLIXIMAB
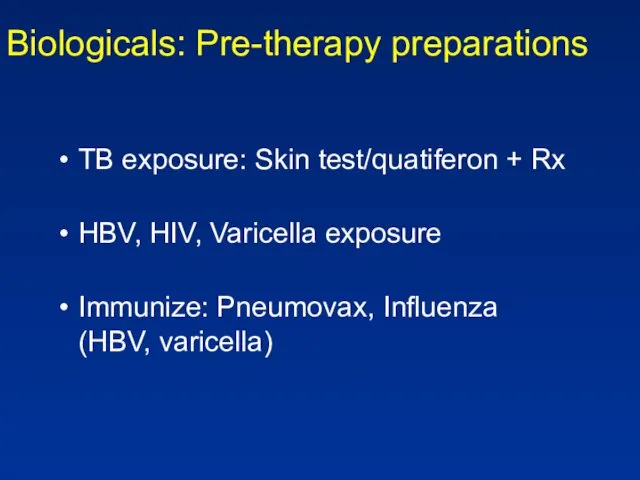
- 72. Biologicals: Pre-therapy preparations TB exposure: Skin test/quatiferon + Rx HBV, HIV, Varicella exposure Immunize: Pneumovax, Influenza
- 73. Diagnosis
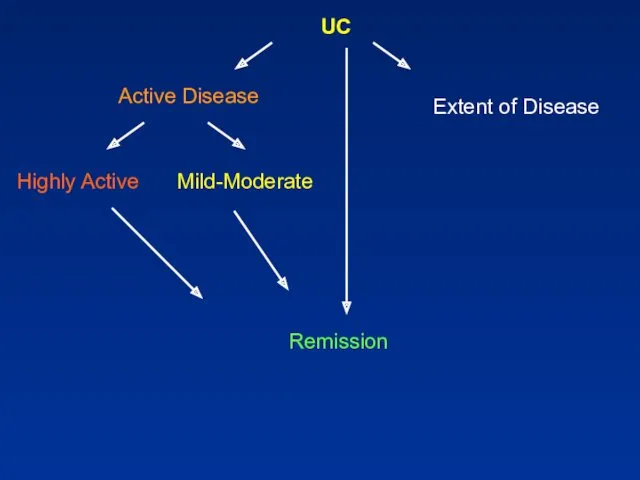
- 74. UC Active Disease Highly Active Mild-Moderate Remission Extent of Disease
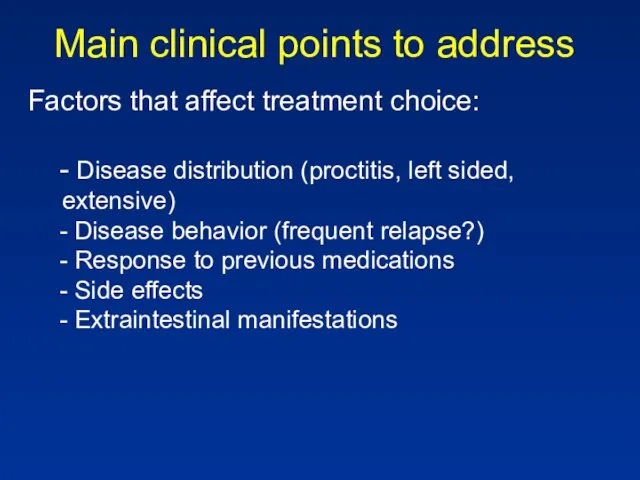
- 75. Main clinical points to address Factors that affect treatment choice: - Disease distribution (proctitis, left sided,
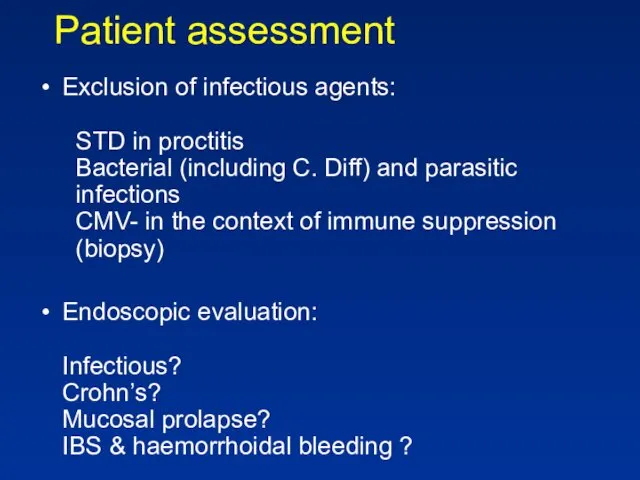
- 76. Patient assessment Exclusion of infectious agents: STD in proctitis Bacterial (including C. Diff) and parasitic infections
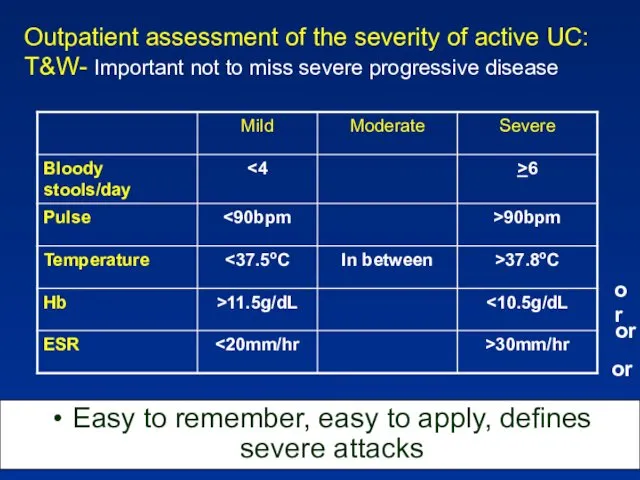
- 77. Outpatient assessment of the severity of active UC: T&W- Important not to miss severe progressive disease
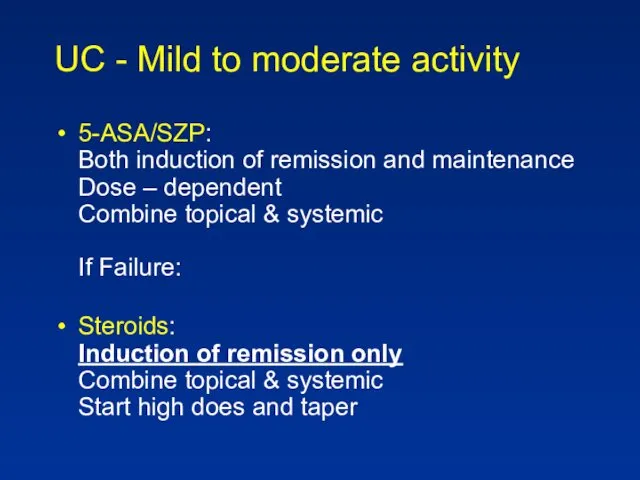
- 78. UC - Mild to moderate activity 5-ASA/SZP: Both induction of remission and maintenance Dose – dependent
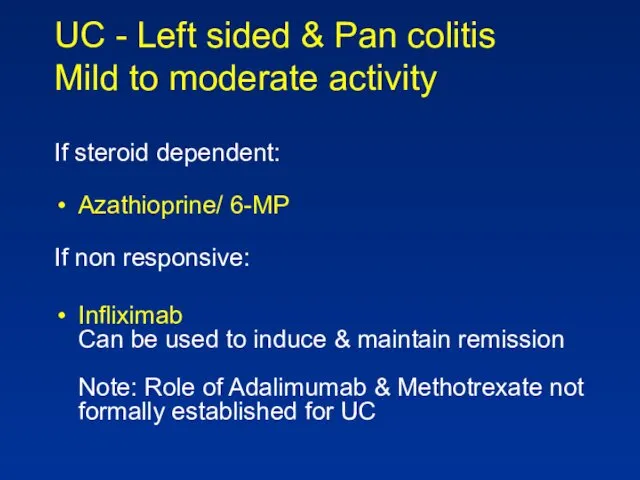
- 79. UC - Left sided & Pan colitis Mild to moderate activity If steroid dependent: Azathioprine/ 6-MP
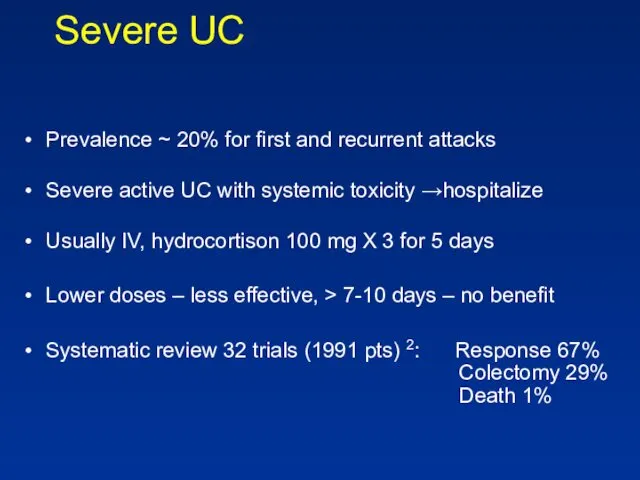
- 80. Severe UC Prevalence ~ 20% for first and recurrent attacks Severe active UC with systemic toxicity
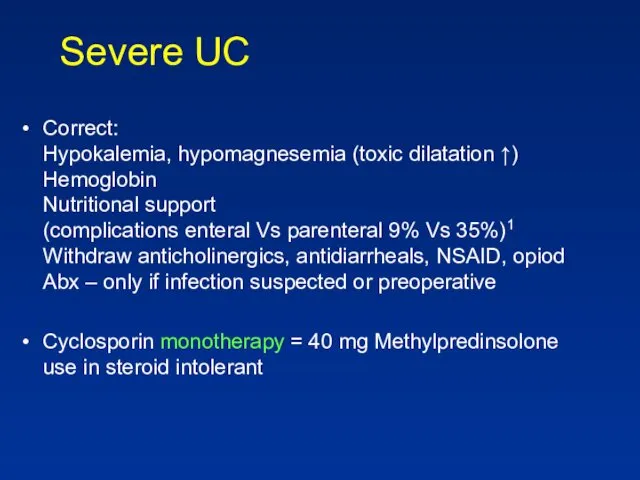
- 81. Severe UC Correct: Hypokalemia, hypomagnesemia (toxic dilatation ↑) Hemoglobin Nutritional support (complications enteral Vs parenteral 9%
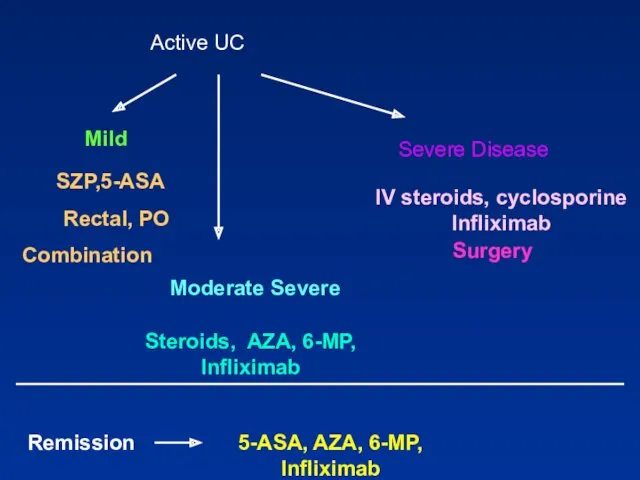
- 83. Active UC Mild Steroids, AZA, 6-MP, Infliximab IV steroids, cyclosporine Infliximab Surgery Remission 5-ASA, AZA, 6-MP,
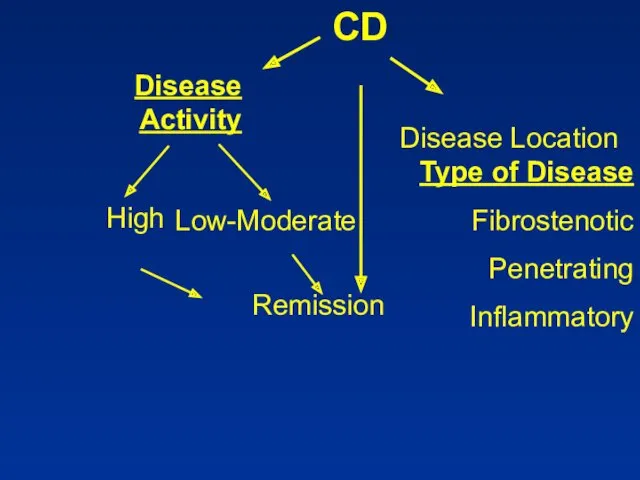
- 84. CD
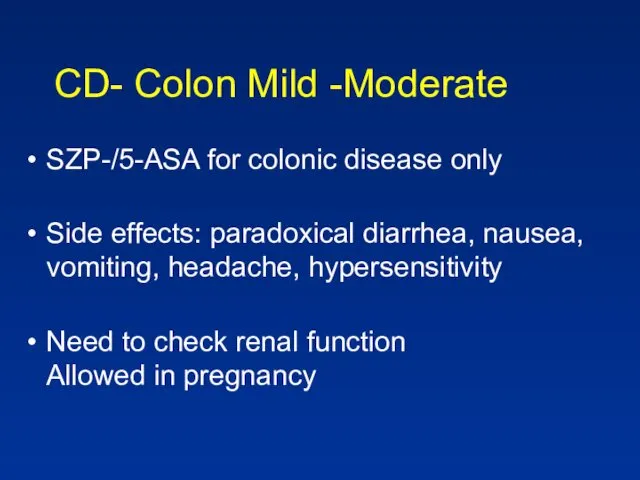
- 85. CD- Colon Mild -Moderate SZP-/5-ASA for colonic disease only Side effects: paradoxical diarrhea, nausea, vomiting, headache,
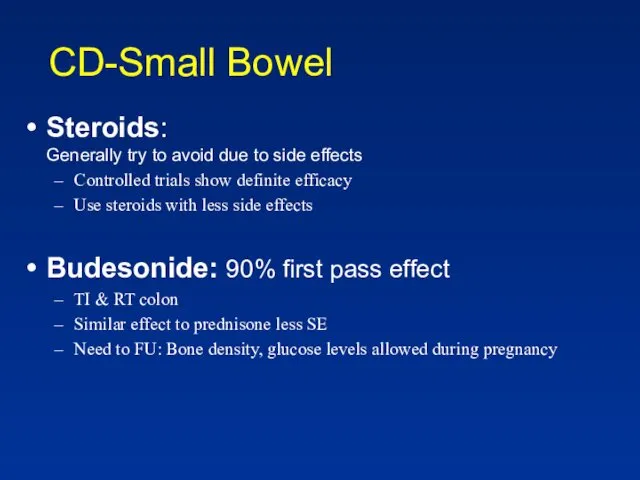
- 86. CD-Small Bowel Steroids: Generally try to avoid due to side effects Controlled trials show definite efficacy
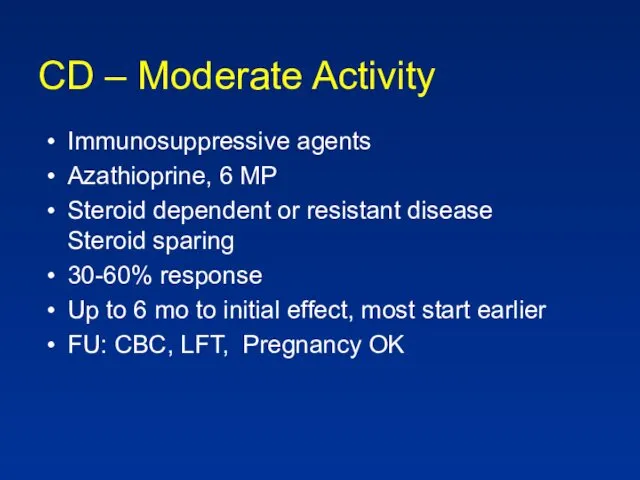
- 87. CD – Moderate Activity Immunosuppressive agents Azathioprine, 6 MP Steroid dependent or resistant disease Steroid sparing
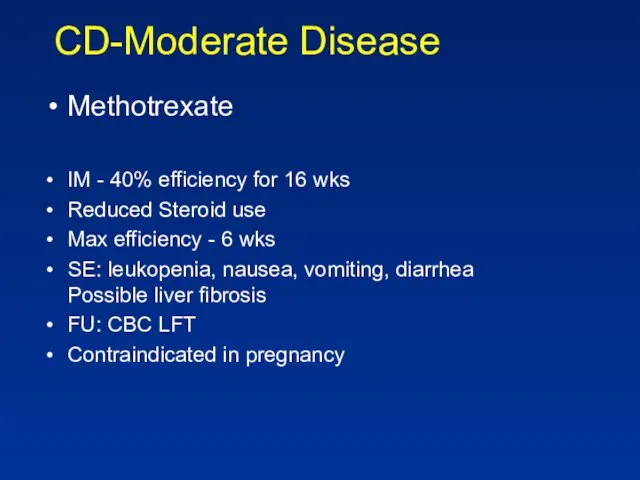
- 88. CD-Moderate Disease Methotrexate IM - 40% efficiency for 16 wks Reduced Steroid use Max efficiency -
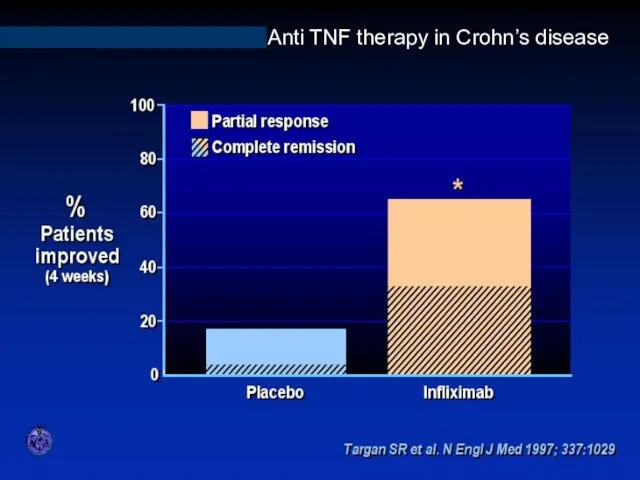
- 89. INFLIXIMAB IN ACTIVE CROHN’S DISEASE Anti TNF therapy in Crohn’s disease
- 90. Biologicals No difference between Infliximab and Adalimumab for efficacy Different modes of administration Loading, scheduled therapy
- 91. CD- Severe Disease Hospitalization IV steroids If abscess, fistula- drain, consider TPN Anti TNF Abs
- 92. CD- Effect of Disease Type Perianal & fistula: Antibiotics Azathioprine/6 MP Infliximab Surgery Treatment sequence: Image,
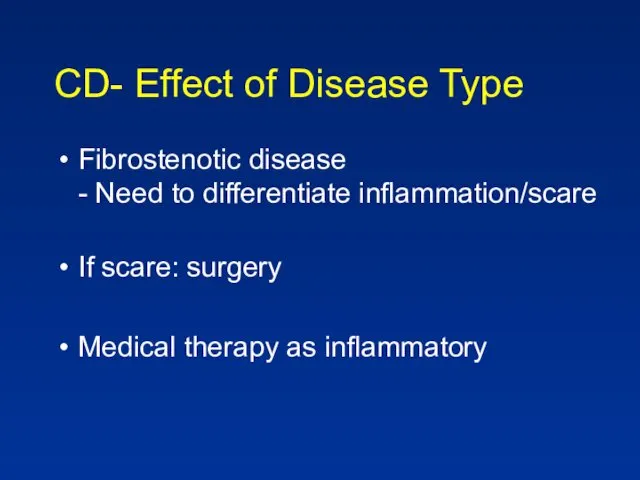
- 93. CD- Effect of Disease Type Fibrostenotic disease - Need to differentiate inflammation/scare If scare: surgery Medical
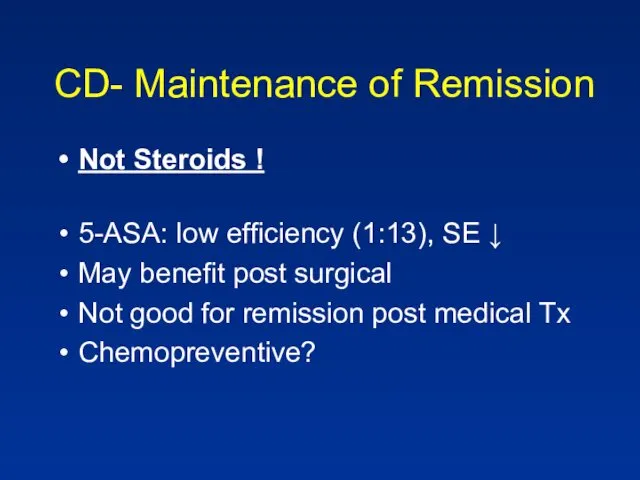
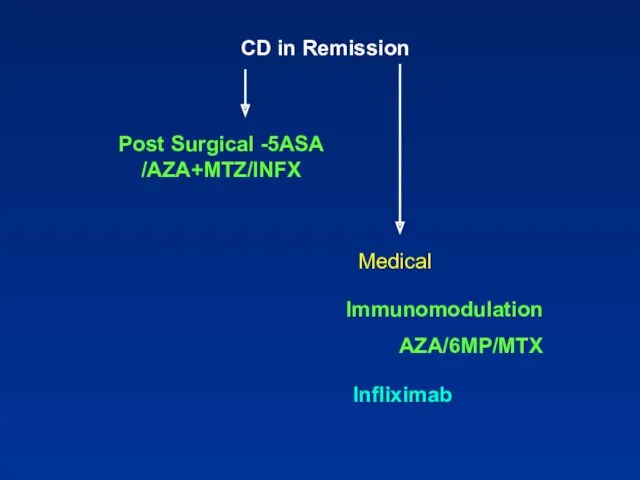
- 94. CD- Maintenance of Remission Not Steroids ! 5-ASA: low efficiency (1:13), SE ↓ May benefit post
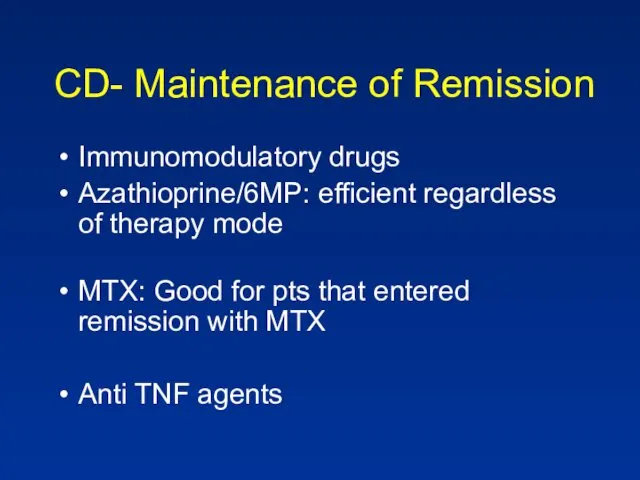
- 95. CD- Maintenance of Remission Immunomodulatory drugs Azathioprine/6MP: efficient regardless of therapy mode MTX: Good for pts
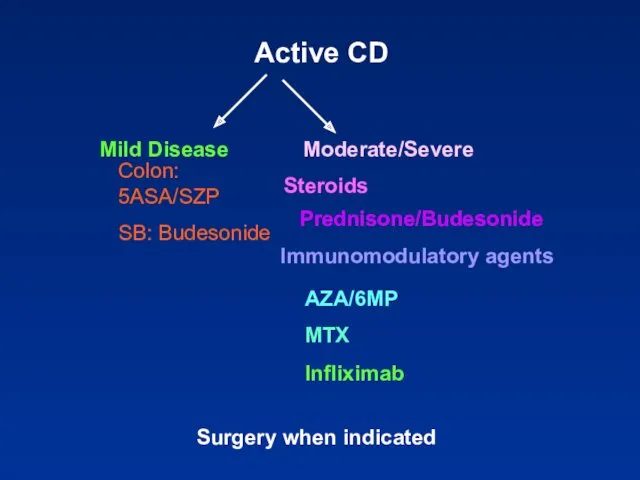
- 96. Active CD Colon: 5ASA/SZP SB: Budesonide Steroids Prednisone/Budesonide Immunomodulatory agents AZA/6MP MTX Infliximab Surgery when indicated
- 97. CD in Remission Medical Immunomodulation AZA/6MP/MTX Infliximab
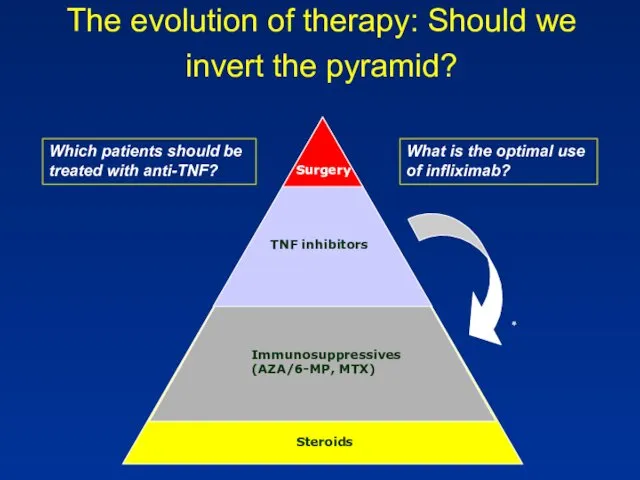
- 98. The evolution of therapy: Should we invert the pyramid? Which patients should be treated with anti-TNF?
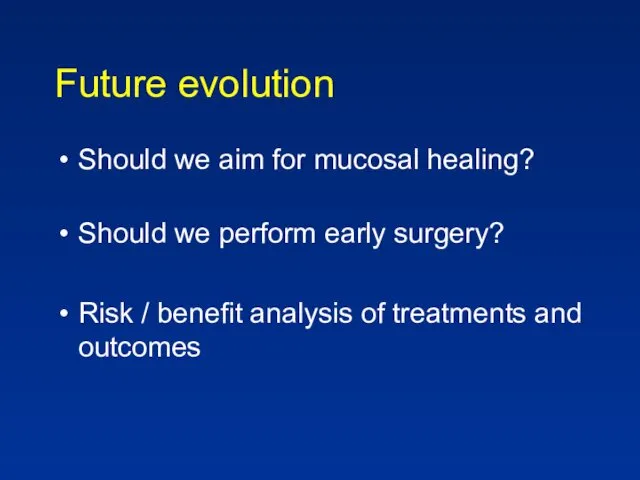
- 99. Future evolution Should we aim for mucosal healing? Should we perform early surgery? Risk / benefit
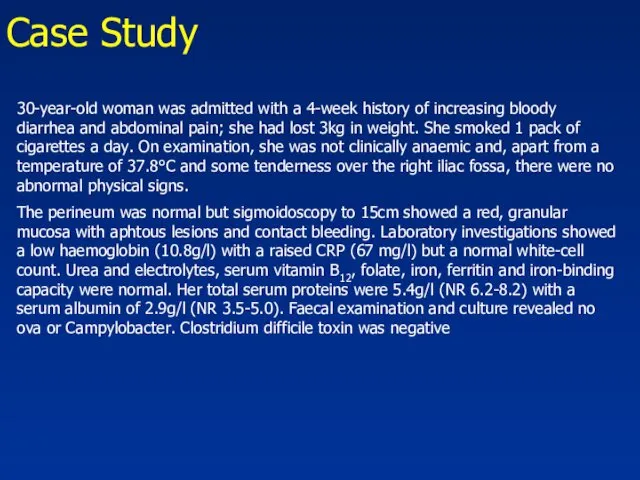
- 100. Case Study 30-year-old woman was admitted with a 4-week history of increasing bloody diarrhea and abdominal
- 101. Case Study The rectal biopsy : many crypt abscesses were present. The lamina propria contained a
- 102. י.ע. 9/2011 בת 54, מזה כחודש וחצי סובלת משלשולים רבים, יציאות דמיות וריריות לסירוגין, ירידה במשקל
- 103. אושפזה בפנימית להמשך בירור וטיפול. בקבלתה הוחל טיפול בסטרואידים ורפסל.במהלך אשפוזה שיפור ניכר בתלונות. לאחר 3
- 104. באשפוז הקודם הותחל גם טיפול גם ב6-MP. שוחחתי ארוכות עם החולה ובעלה אודות הסיכונים שבטיפול זה
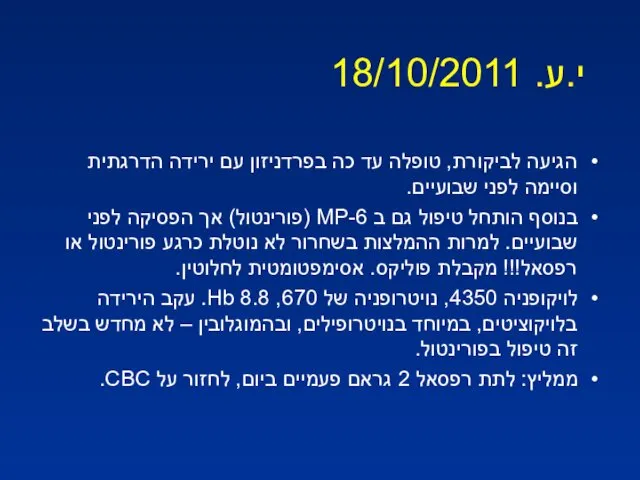
- 105. י.ע. 18/10/2011 הגיעה לביקורת, טופלה עד כה בפרדניזון עם ירידה הדרגתית וסיימה לפני שבועיים. בנוסף הותחל
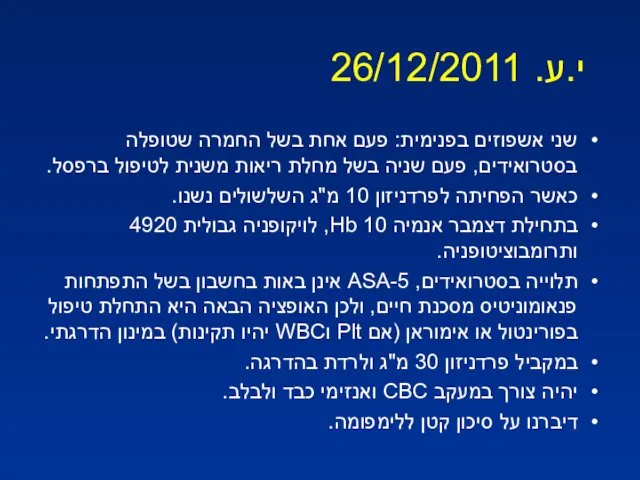
- 106. י.ע. 26/12/2011 שני אשפוזים בפנימית: פעם אחת בשל החמרה שטופלה בסטרואידים, פעם שניה בשל מחלת ריאות
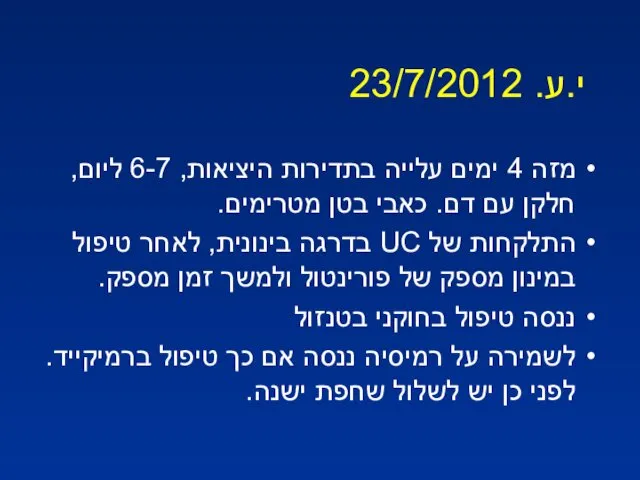
- 107. י.ע. 23/7/2012 מזה 4 ימים עלייה בתדירות היציאות, 6-7 ליום, חלקן עם דם. כאבי בטן מטרימים.
- 109. Скачать презентацию



 Мужское бесплодие
Мужское бесплодие Оценка комплексного состояния здоровья ребенка, определение группы здоровья по форме 112/у
Оценка комплексного состояния здоровья ребенка, определение группы здоровья по форме 112/у Нейролептические экстрапирамидные расстройства
Нейролептические экстрапирамидные расстройства Тірі ағзаларға ульракүлгін сәулелерінің әсері
Тірі ағзаларға ульракүлгін сәулелерінің әсері Лечение и профилактика гриппа, вызванного вирусом типа A/H1N1
Лечение и профилактика гриппа, вызванного вирусом типа A/H1N1 Порядок оказания акушерско-гинекологической помощи в Российской Федерации
Порядок оказания акушерско-гинекологической помощи в Российской Федерации Военная токсикология. Отравляющие вещества психотомиметического действия. Клиника, диагностика, лечение
Военная токсикология. Отравляющие вещества психотомиметического действия. Клиника, диагностика, лечение Лихорадка неясного генеза - вчера, сегодня, завтра
Лихорадка неясного генеза - вчера, сегодня, завтра Первая помощь при ранении
Первая помощь при ранении Аппендициттің асқынулары
Аппендициттің асқынулары Біологія і медицина XVIII-XIX
Біологія і медицина XVIII-XIX Муталлапова 301М Орг. мед. пом. жен. и детям
Муталлапова 301М Орг. мед. пом. жен. и детям Основи курортології. Курортні ресурси України. (Тема 2)
Основи курортології. Курортні ресурси України. (Тема 2) Лечебная физическая культура при заболевании глаз
Лечебная физическая культура при заболевании глаз Сепсис новонароджених етіологія, клініка, лікування. Синдром системної запальної відповіді
Сепсис новонароджених етіологія, клініка, лікування. Синдром системної запальної відповіді Коронавирус COVID-19
Коронавирус COVID-19 Амилоидоз почек. Диагностика, принципы лечения
Амилоидоз почек. Диагностика, принципы лечения Рак эндометрия
Рак эндометрия Толстокишечные кровотечение
Толстокишечные кровотечение Внешние признаки внутренних болезней
Внешние признаки внутренних болезней Сестринский уход за спинальными больными
Сестринский уход за спинальными больными Основы трансфузиологии
Основы трансфузиологии Язвенная болезнь. Патогенетические механизмы и принципы терапии
Язвенная болезнь. Патогенетические механизмы и принципы терапии Заболевания шейки матки
Заболевания шейки матки Трехуровневая модель оказания реабилитационной помощи
Трехуровневая модель оказания реабилитационной помощи Особливості формування серця і стимуляція регенерації серцевої м'язової тканини в умовах сучасної медицини
Особливості формування серця і стимуляція регенерації серцевої м'язової тканини в умовах сучасної медицини Функциональные пробы в ЛФК
Функциональные пробы в ЛФК Артериялық гипертензия
Артериялық гипертензия