Содержание
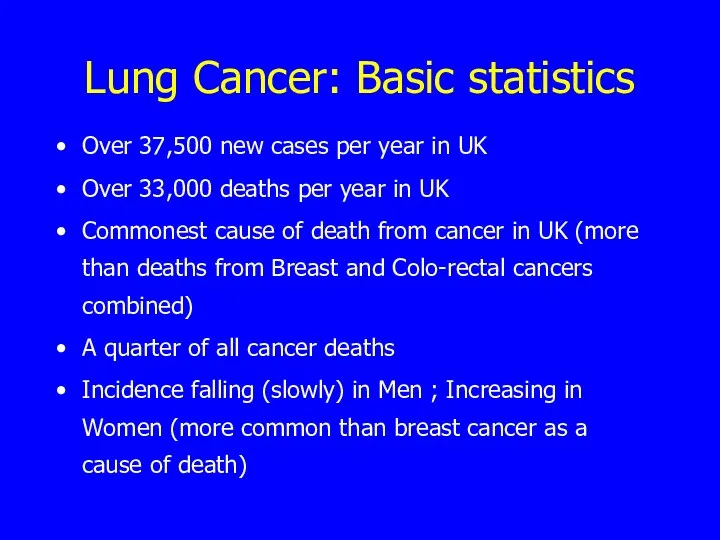
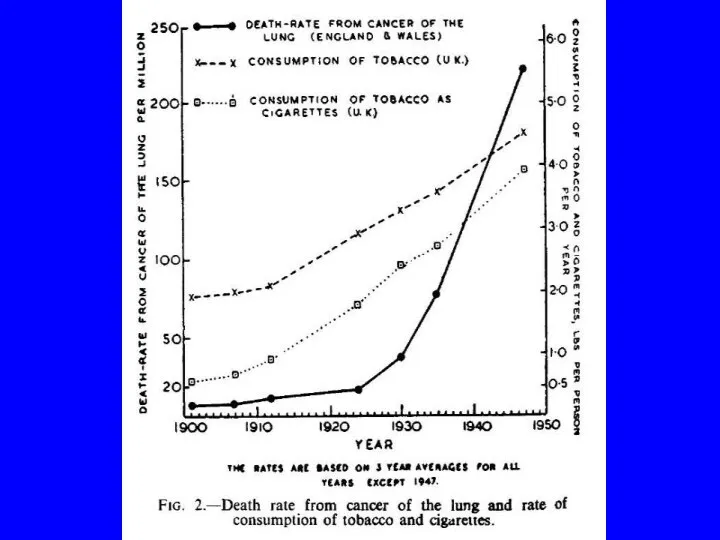
- 2. Lung Cancer: Basic statistics Over 37,500 new cases per year in UK Over 33,000 deaths per
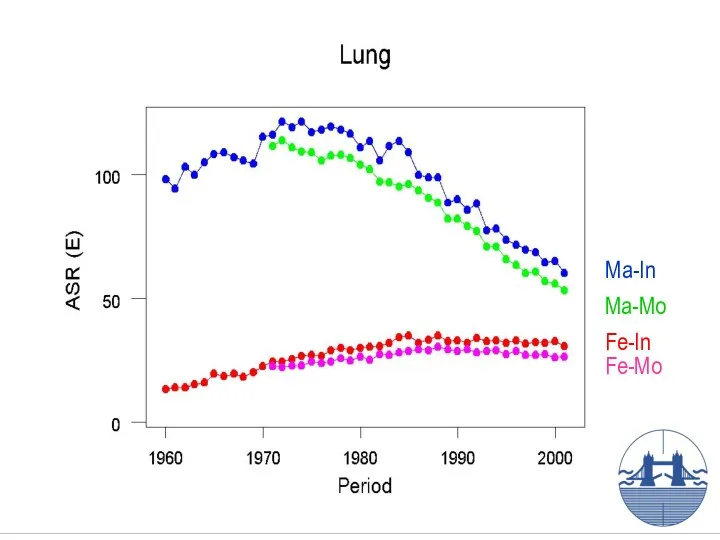
- 3. Ma-In Fe-In Ma-Mo Fe-Mo
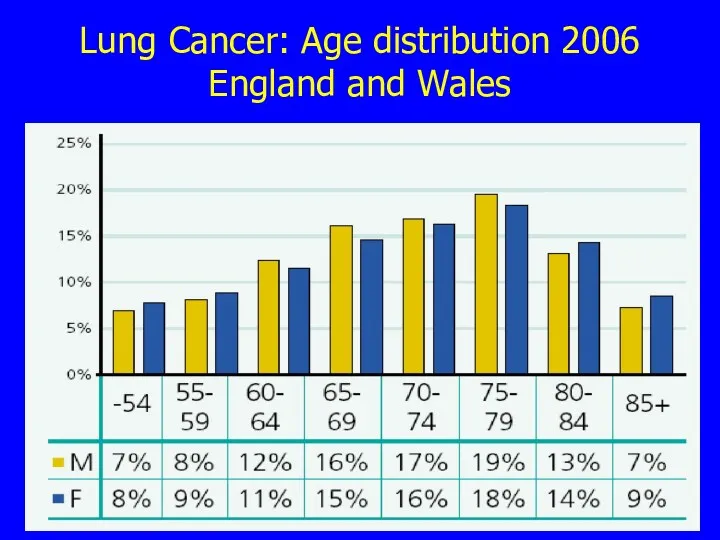
- 4. Lung Cancer: Age distribution 2006 England and Wales
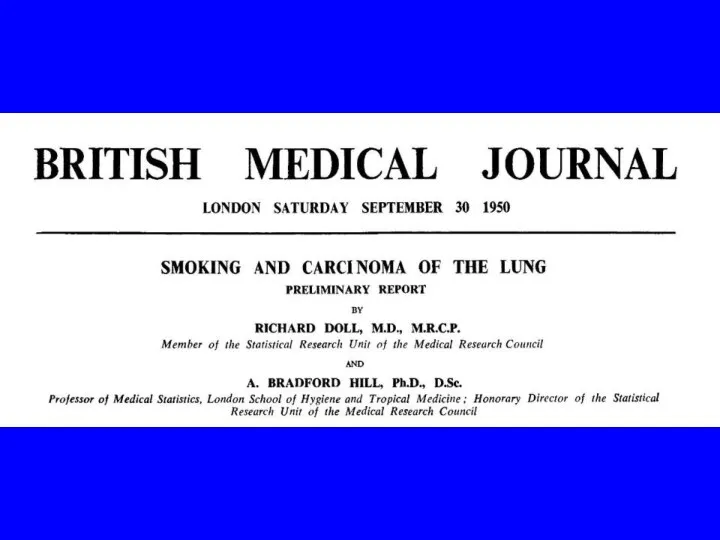
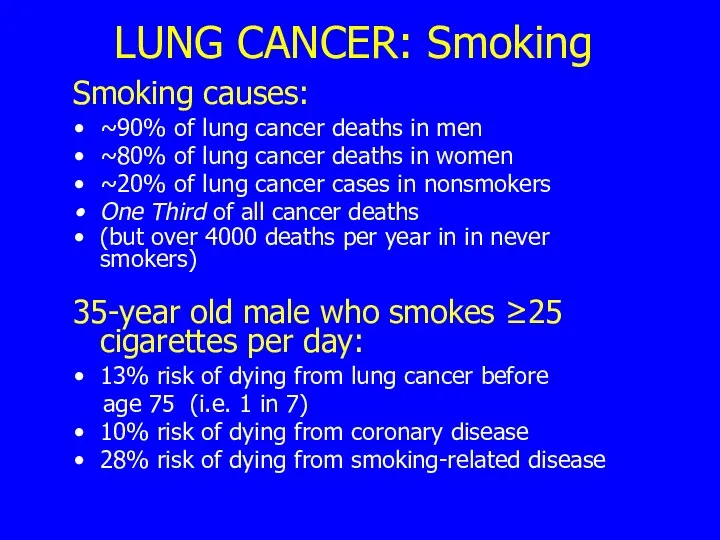
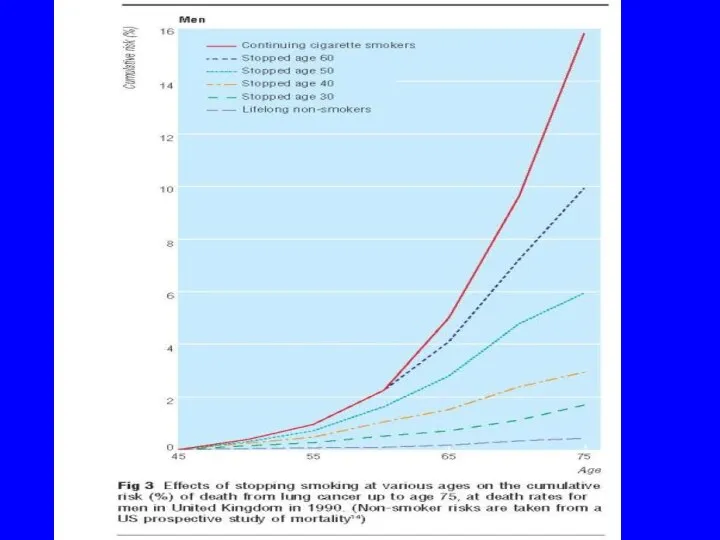
- 7. LUNG CANCER: Smoking Smoking causes: ~90% of lung cancer deaths in men ~80% of lung cancer
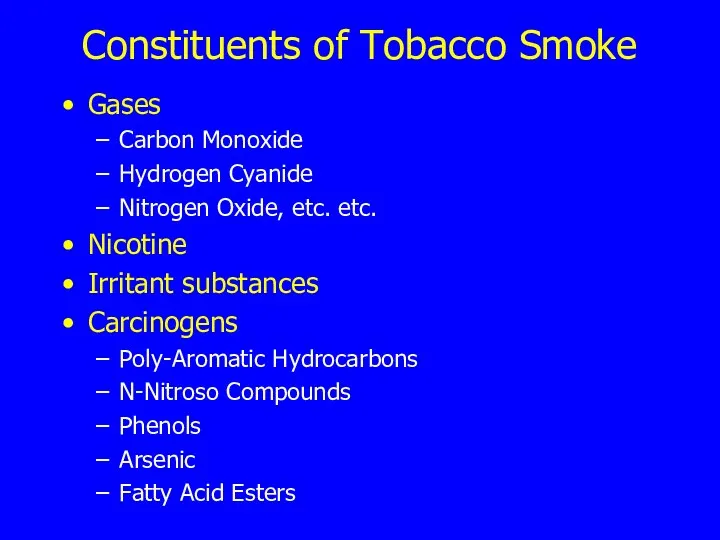
- 8. Constituents of Tobacco Smoke Gases Carbon Monoxide Hydrogen Cyanide Nitrogen Oxide, etc. etc. Nicotine Irritant substances
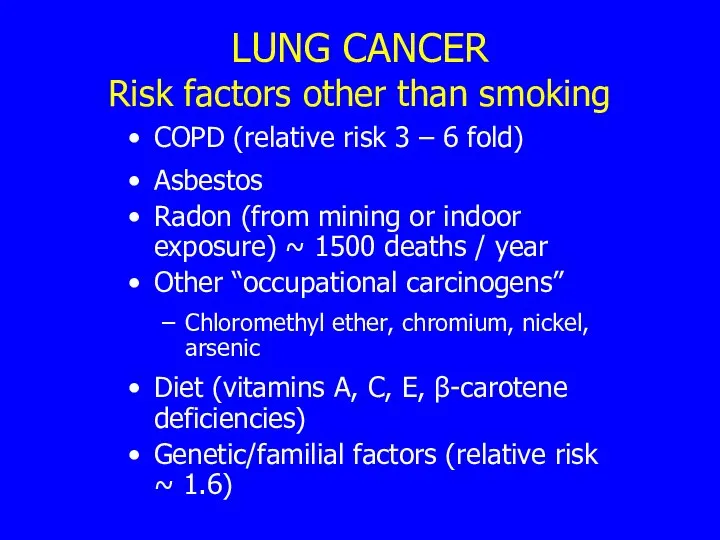
- 10. LUNG CANCER Risk factors other than smoking COPD (relative risk 3 – 6 fold) Asbestos Radon
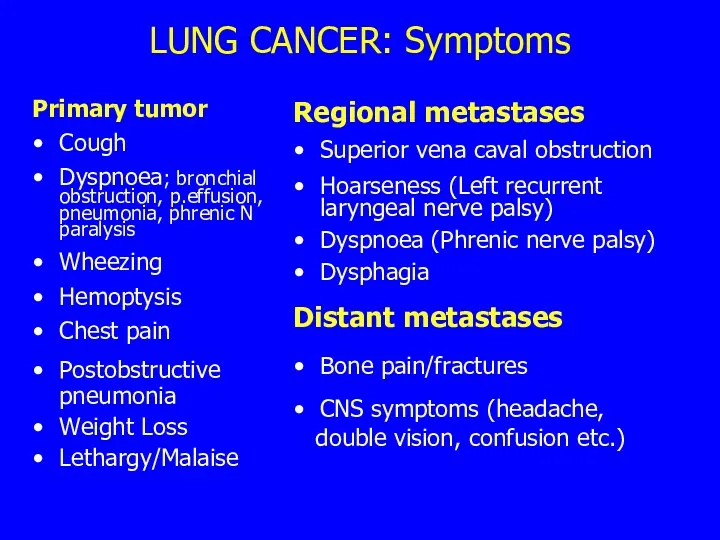
- 12. LUNG CANCER: Symptoms Primary tumor Cough Dyspnoea; bronchial obstruction, p.effusion, pneumonia, phrenic N paralysis Wheezing Hemoptysis
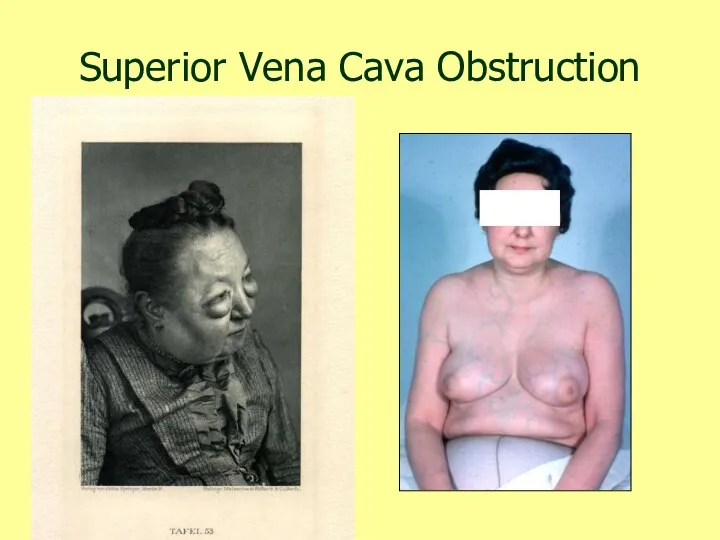
- 13. Superior Vena Cava Obstruction
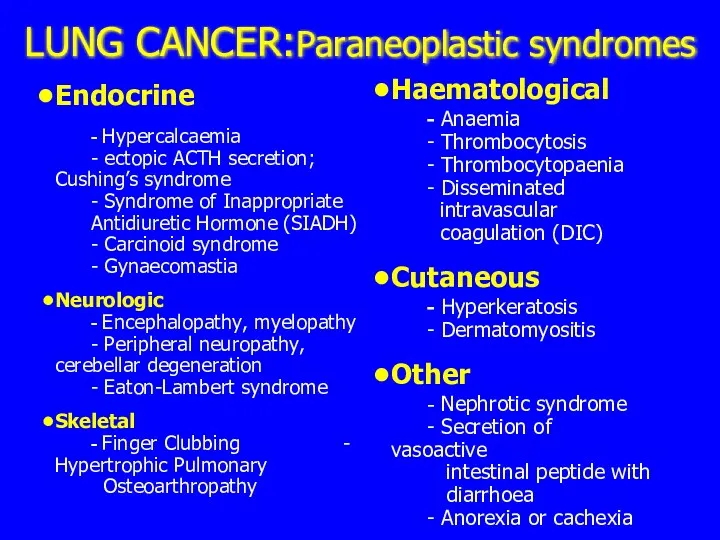
- 14. LUNG CANCER:Paraneoplastic syndromes Endocrine - Hypercalcaemia - ectopic ACTH secretion; Cushing’s syndrome - Syndrome of Inappropriate
- 15. Lung Cancer : Finger Clubbing
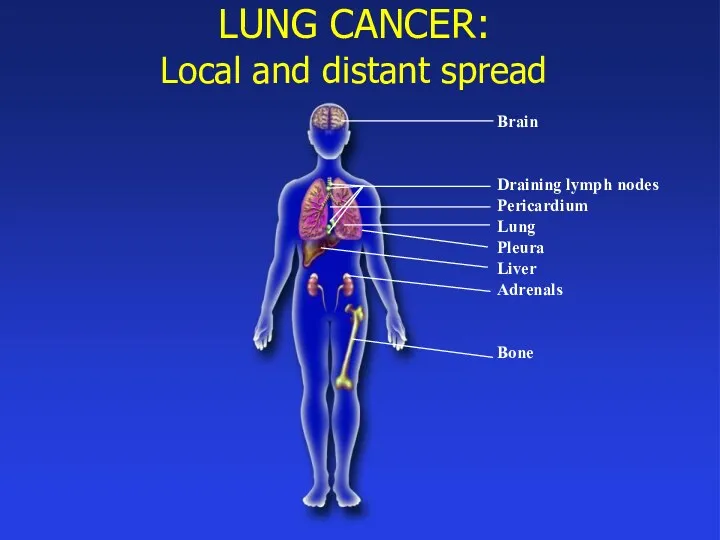
- 16. LUNG CANCER: Local and distant spread Brain Draining lymph nodes Pericardium Lung Pleura Liver Adrenals Bone
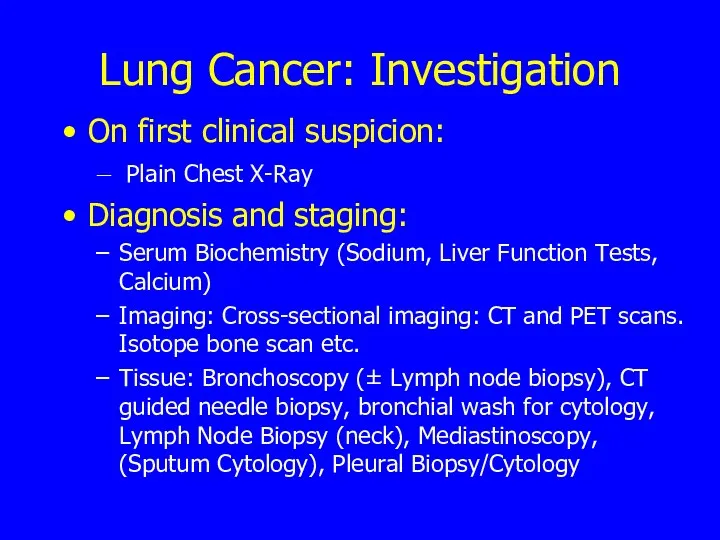
- 17. Lung Cancer: Investigation On first clinical suspicion: Plain Chest X-Ray Diagnosis and staging: Serum Biochemistry (Sodium,
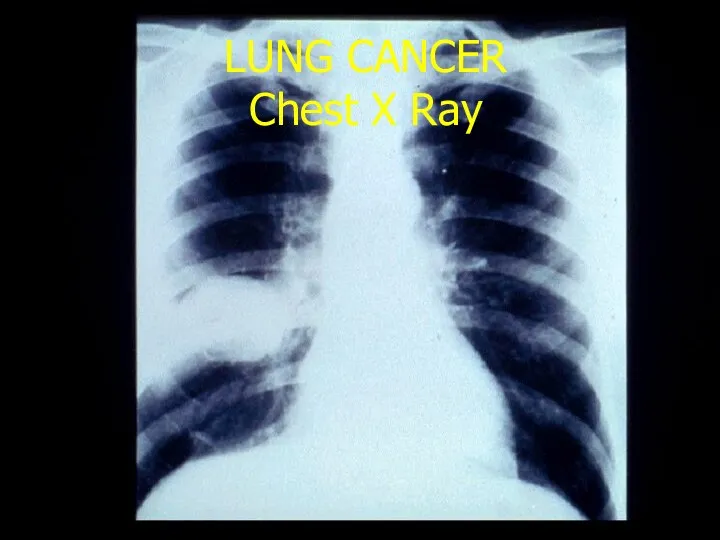
- 18. LUNG CANCER Chest X Ray
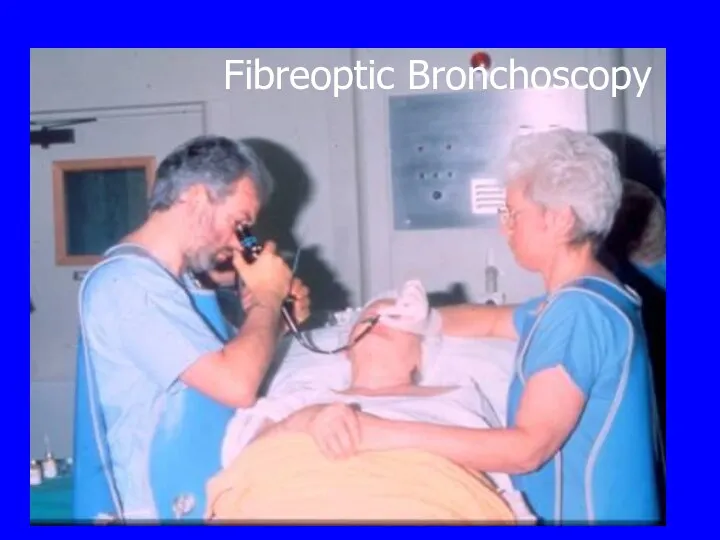
- 19. Fibreoptic Bronchoscopy
- 20. LUNG CANCER Bronchoscopy
- 21. Lung cancer staging TNM T- tumor size. N- lymph node involvement. M- distant metastasis. CT, PET,
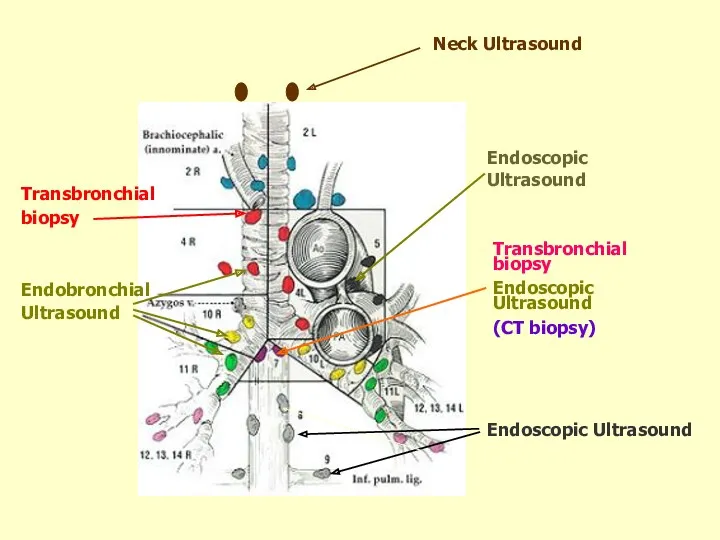
- 22. Transbronchial biopsy Endoscopic Ultrasound (CT biopsy) Endoscopic Ultrasound Endoscopic Ultrasound Neck Ultrasound Endobronchial Ultrasound Transbronchial biopsy
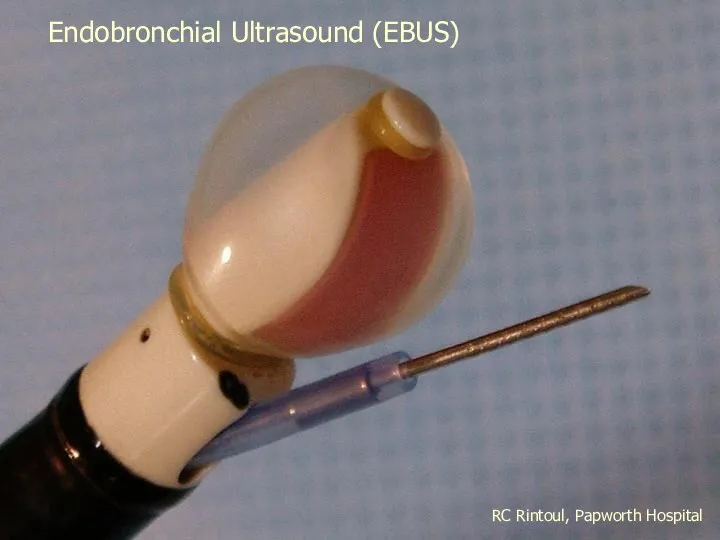
- 23. RC Rintoul, Papworth Hospital Endobronchial Ultrasound (EBUS)
- 24. RC Rintoul, Papworth Hospital RC Rintoul, Papworth Hospital
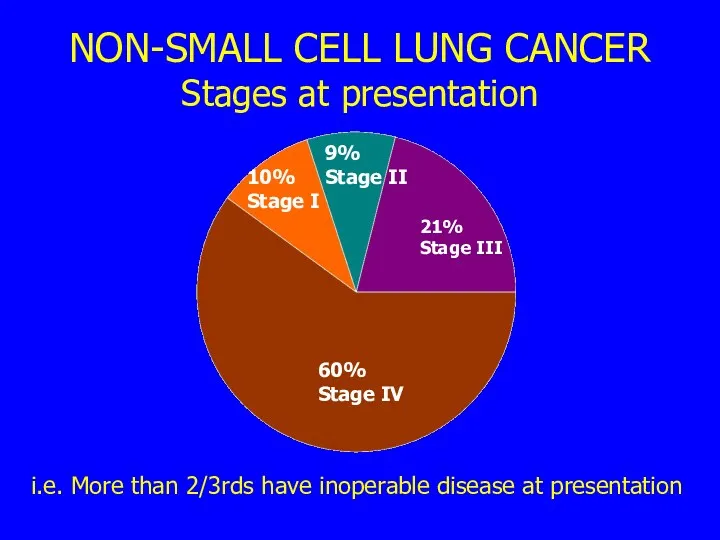
- 25. NON-SMALL CELL LUNG CANCER Stages at presentation i.e. More than 2/3rds have inoperable disease at presentation
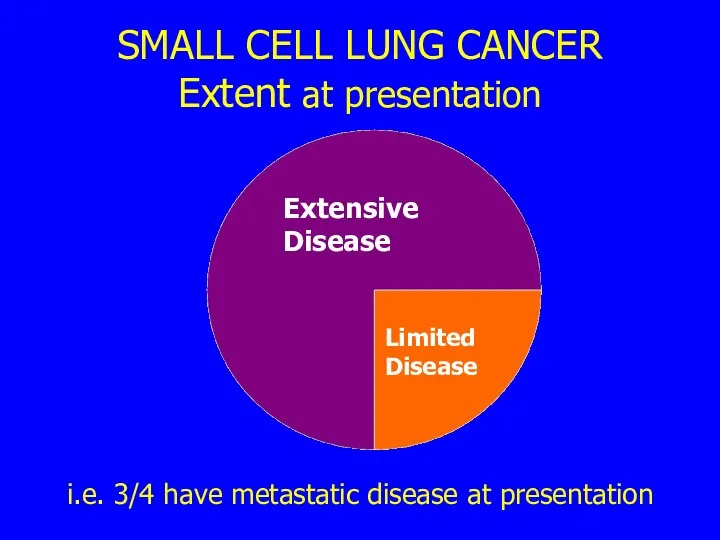
- 26. SMALL CELL LUNG CANCER Extent at presentation i.e. 3/4 have metastatic disease at presentation Limited Disease
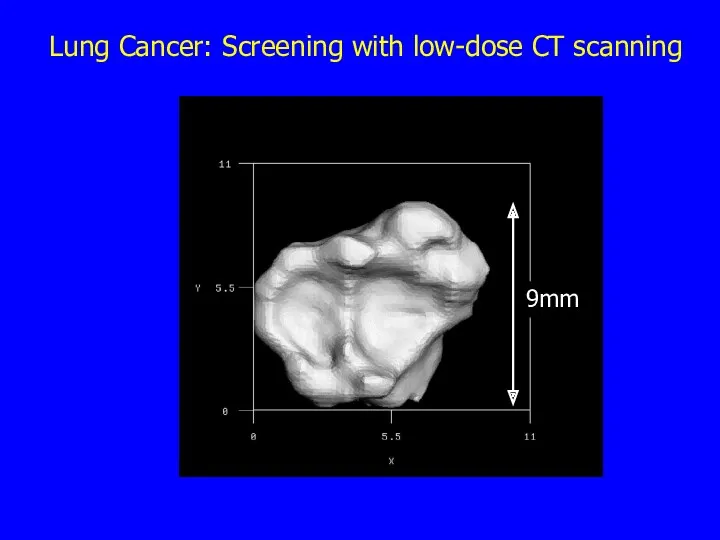
- 27. Lung Cancer: Screening with low-dose CT scanning 9mm
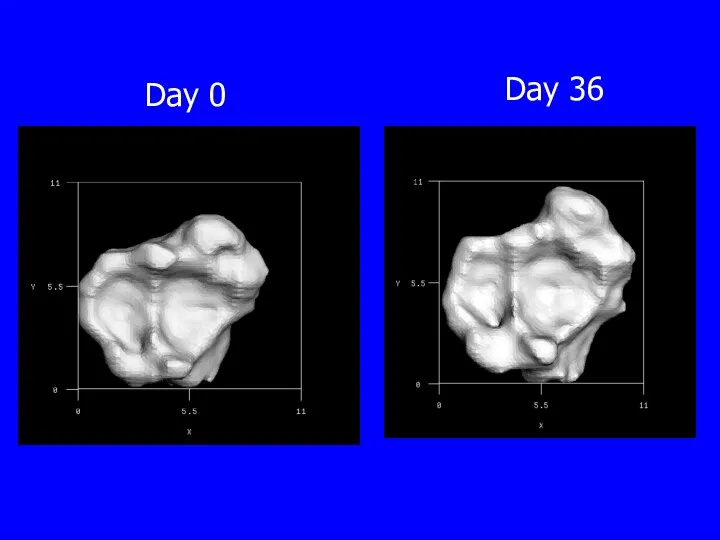
- 28. Day 0 Day 36
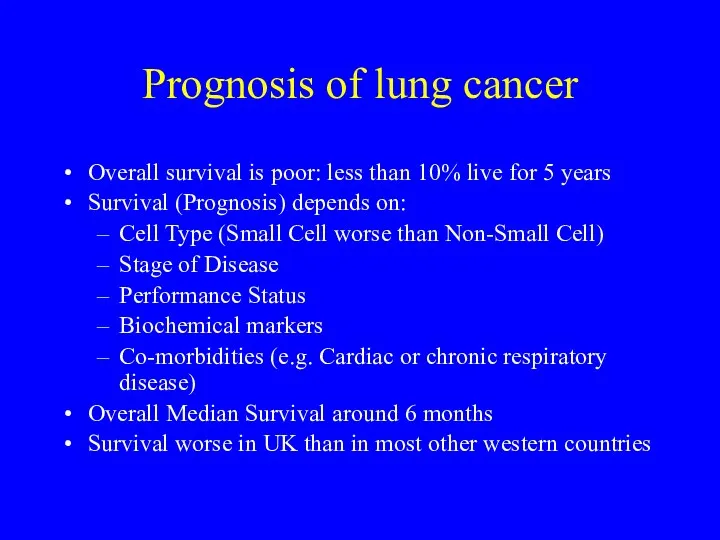
- 29. Prognosis of lung cancer Overall survival is poor: less than 10% live for 5 years Survival
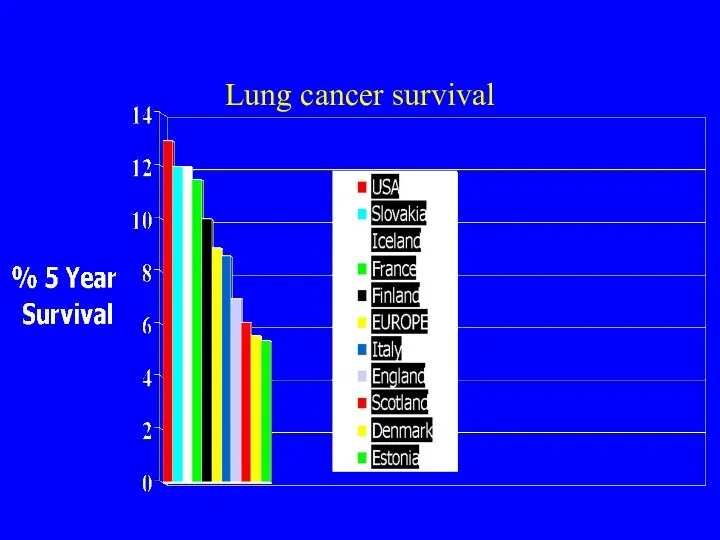
- 30. Lung cancer survival
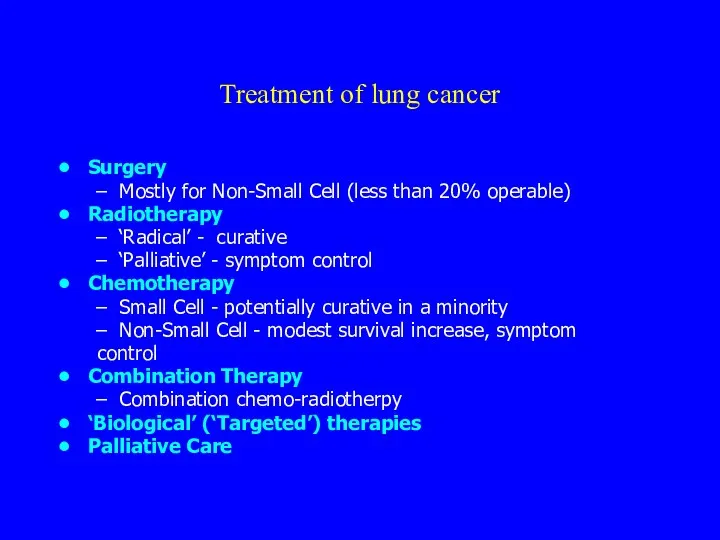
- 31. Treatment of lung cancer Surgery Mostly for Non-Small Cell (less than 20% operable) Radiotherapy ‘Radical’ -
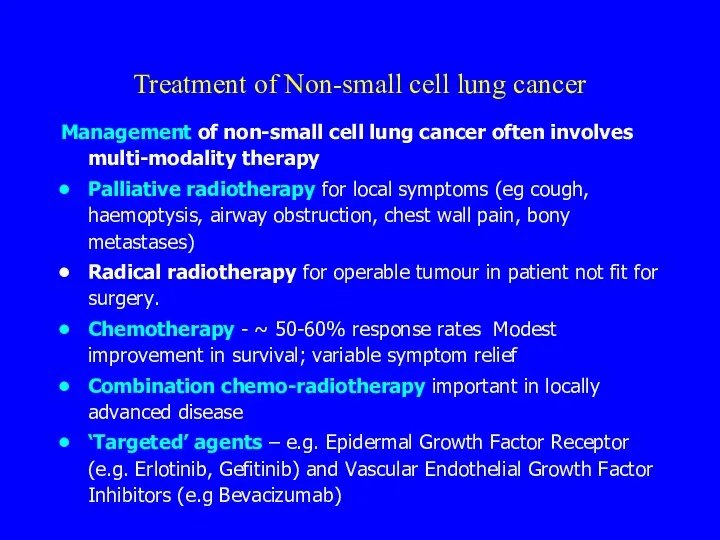
- 32. Treatment of Non-small cell lung cancer Management of non-small cell lung cancer often involves multi-modality therapy
- 33. Prognosis of non-small cell cancer Up to 20% operable Overall surgical survival 50% at 5 years
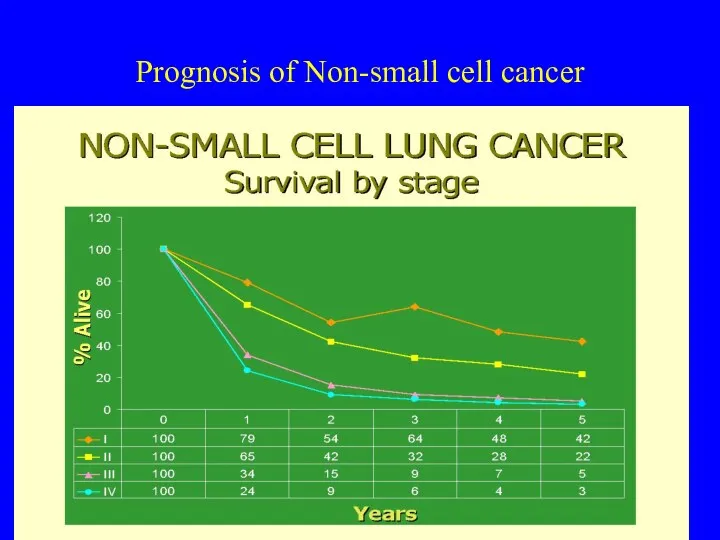
- 34. Prognosis of Non-small cell cancer Survival by stage
- 35. Treatment and prognosis of small cell cancer A systemic disease in >80% of cases Rarely operable
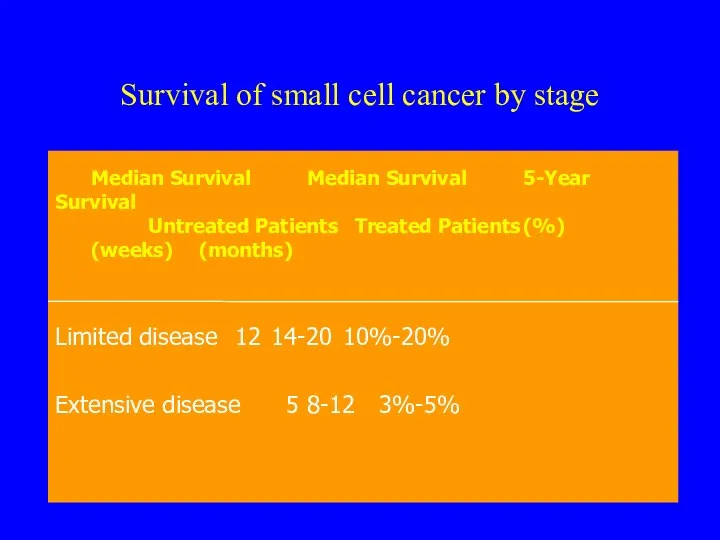
- 36. Survival of small cell cancer by stage
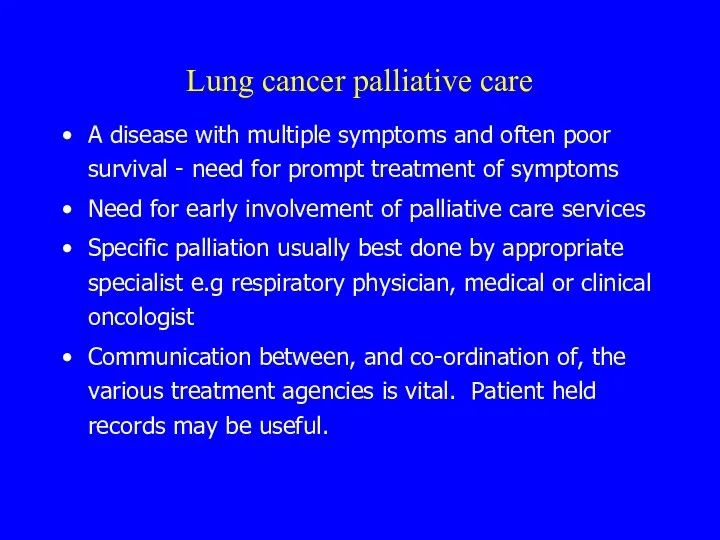
- 37. Lung cancer palliative care A disease with multiple symptoms and often poor survival - need for
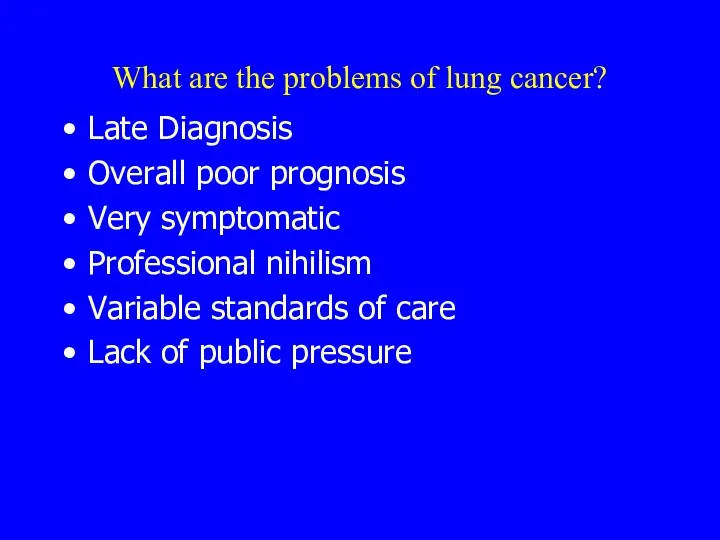
- 38. What are the problems of lung cancer? Late Diagnosis Overall poor prognosis Very symptomatic Professional nihilism
- 40. Скачать презентацию



 Консультирование бесплодной пары
Консультирование бесплодной пары Реабилитация больных, перенесших инсульт
Реабилитация больных, перенесших инсульт Паллиативная и симптоматическая помощь терминальным больным при ЗНО органов репродуктивной системы
Паллиативная и симптоматическая помощь терминальным больным при ЗНО органов репродуктивной системы Дифференциальный диагноз состояний, сопровождающихся астмоидным дыханием, лечение и поодерживающий уход
Дифференциальный диагноз состояний, сопровождающихся астмоидным дыханием, лечение и поодерживающий уход Влияние вредных факторов на плод
Влияние вредных факторов на плод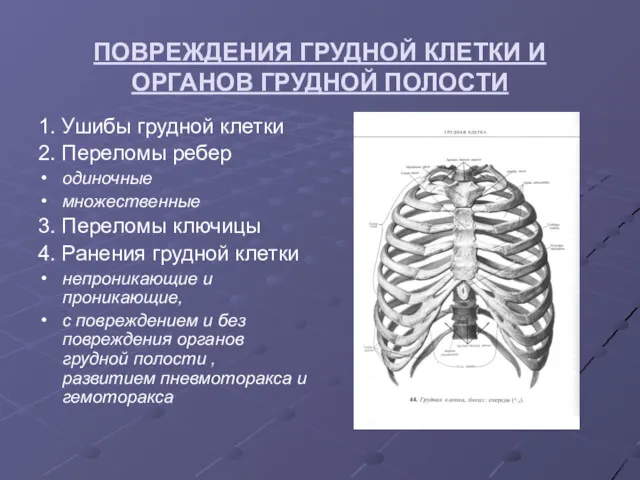 Повреждения грудной клетки и органов грудной полости
Повреждения грудной клетки и органов грудной полости Ангины. Хронический тонзиллит
Ангины. Хронический тонзиллит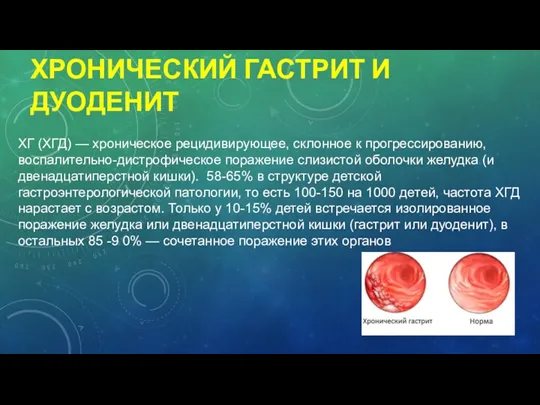 Хронический гастрит и дуоденит
Хронический гастрит и дуоденит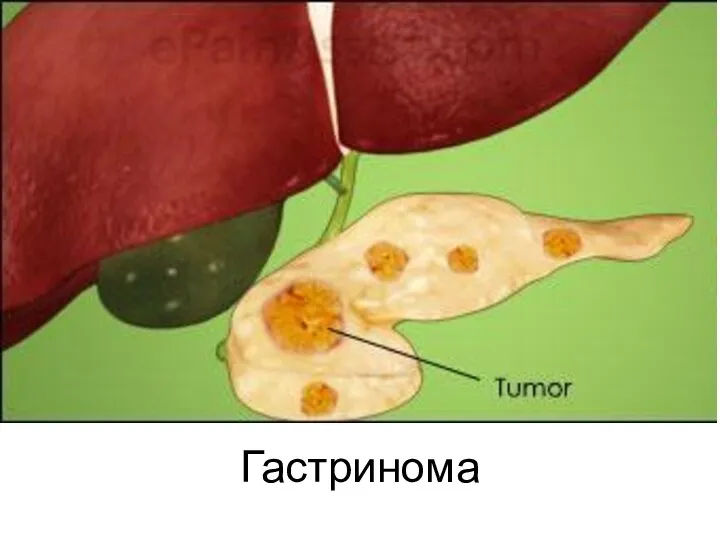 Гастринома
Гастринома Классификация лекарственных растений и эксплуатация ресурсов лекарственных растений
Классификация лекарственных растений и эксплуатация ресурсов лекарственных растений Рентгенодиагностика грибковых и паразитарных заболеваний легких
Рентгенодиагностика грибковых и паразитарных заболеваний легких Особенности памяти школьника
Особенности памяти школьника Аймақтық денсаулықсақтаудағы ақпараттанудың маңызды міндеттемелері
Аймақтық денсаулықсақтаудағы ақпараттанудың маңызды міндеттемелері Первичная вакцинация 10-валентной пневмококковой нетипируемой гемофильный белок D конъюгированной вакциной (PHiD-CV) младенцев
Первичная вакцинация 10-валентной пневмококковой нетипируемой гемофильный белок D конъюгированной вакциной (PHiD-CV) младенцев Эклампсия у собак
Эклампсия у собак Балалардағы эхинококкоздың алдын алу жолдары
Балалардағы эхинококкоздың алдын алу жолдары Применение новых технологий в ортопедической стоматологии. Технология изготовления безметалловых керамических протезов
Применение новых технологий в ортопедической стоматологии. Технология изготовления безметалловых керамических протезов Cent ans de phagothérapie: de la découverte de Félix D’Hérelle à nos jours
Cent ans de phagothérapie: de la découverte de Félix D’Hérelle à nos jours Бруцеллез
Бруцеллез Предмет и содержание гигиены и экологии человека. Лекция № 1
Предмет и содержание гигиены и экологии человека. Лекция № 1 Classification of female genitals
Classification of female genitals Проктология. Повреждения и инородные тела прямой кишки
Проктология. Повреждения и инородные тела прямой кишки Смерть. Некроз. Апоптоз
Смерть. Некроз. Апоптоз ЭКГ - диагностика при подозрении на инфаркт миокарда
ЭКГ - диагностика при подозрении на инфаркт миокарда Портальная гипертензия
Портальная гипертензия Общие закономерности действия промышленных ядов
Общие закономерности действия промышленных ядов Гемостаздың және қанның реологиялық қасиеттерінің бұзылыстары
Гемостаздың және қанның реологиялық қасиеттерінің бұзылыстары Врожденный гипотиреоз
Врожденный гипотиреоз