Содержание
- 2. Overview Introduction Etiology, epidemiology Pathogenesis Clinical features Complications Diagnosis Treatment Prevention
- 3. Malaria is a life-threatening disease caused by parasites that are transmitted to people through the bites
- 4. Between 2010 and 2015, malaria incidence among populations at risk (the rate of new cases) fell
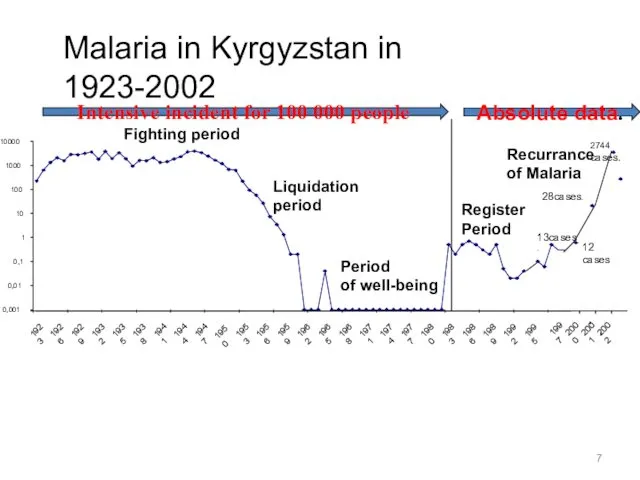
- 7. Malaria in Kyrgyzstan in 1923-2002 0,001 0,01 0,1 1 10 100 1000 10000 1923 1926 1929
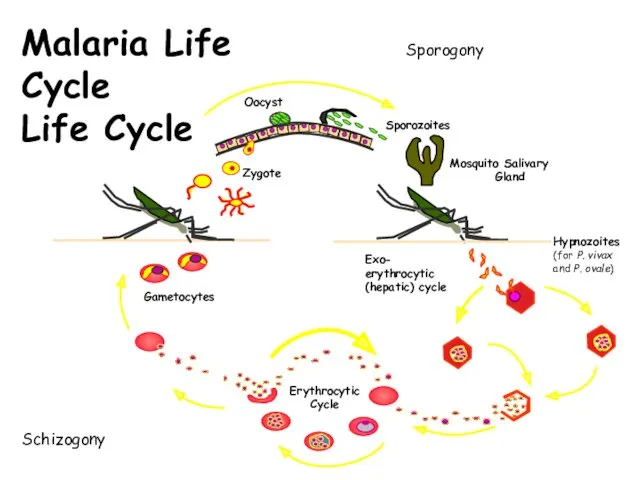
- 8. Exo- erythrocytic (hepatic) cycle Malaria Life Cycle Life Cycle Schizogony Sporogony
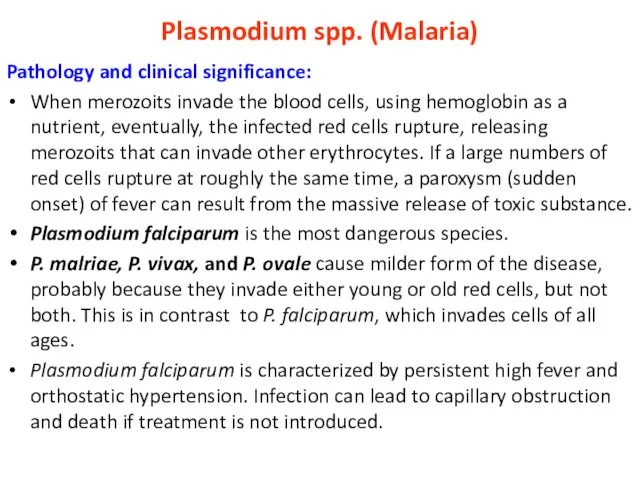
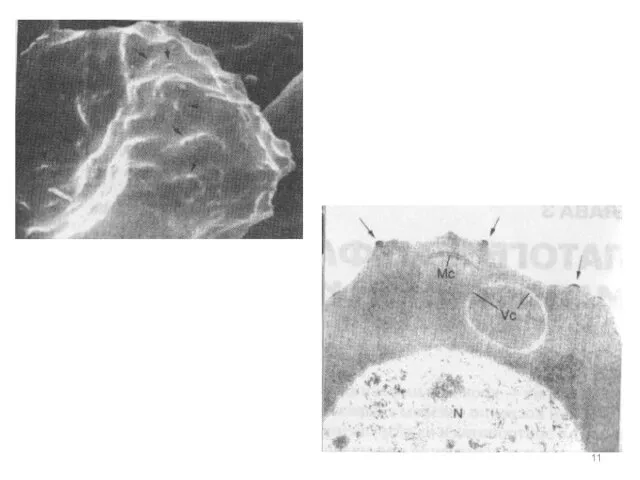
- 10. Plasmodium spp. (Malaria) Pathology and clinical significance: When merozoits invade the blood cells, using hemoglobin as
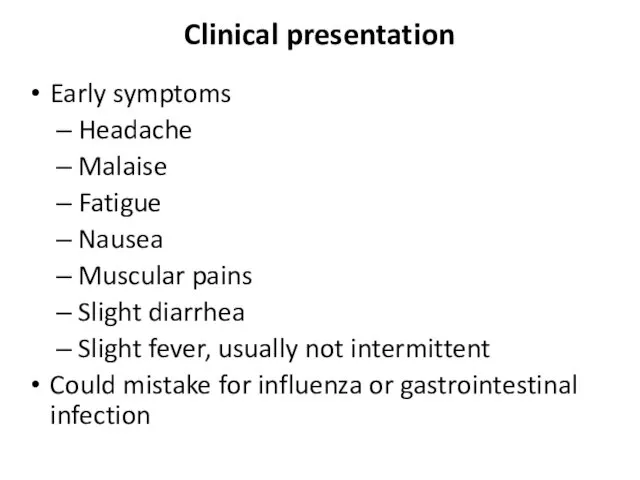
- 12. Clinical presentation Early symptoms Headache Malaise Fatigue Nausea Muscular pains Slight diarrhea Slight fever, usually not
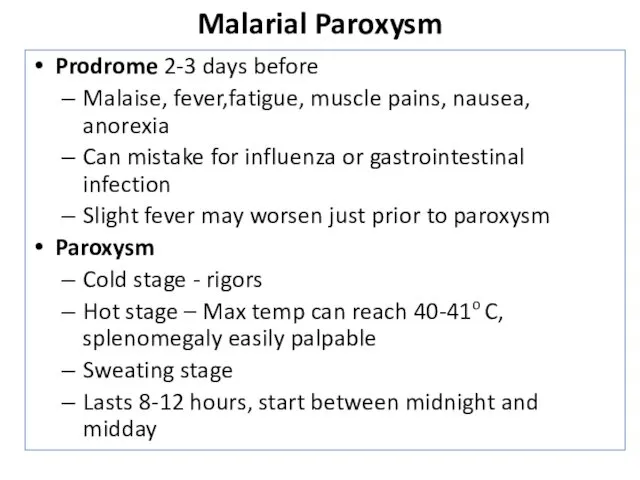
- 13. Malarial Paroxysm Prodrome 2-3 days before Malaise, fever,fatigue, muscle pains, nausea, anorexia Can mistake for influenza
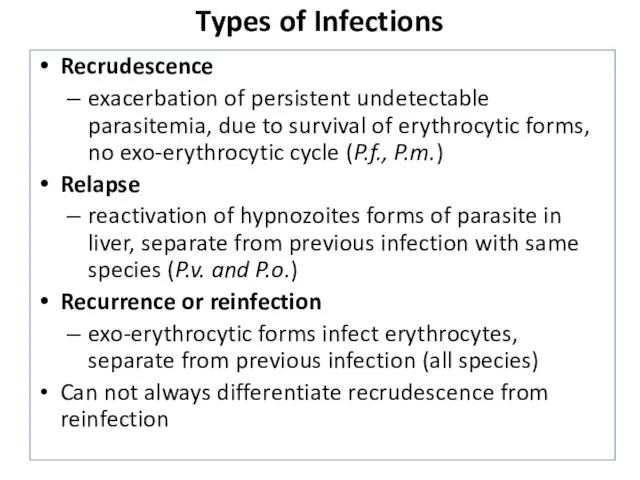
- 14. Types of Infections Recrudescence exacerbation of persistent undetectable parasitemia, due to survival of erythrocytic forms, no
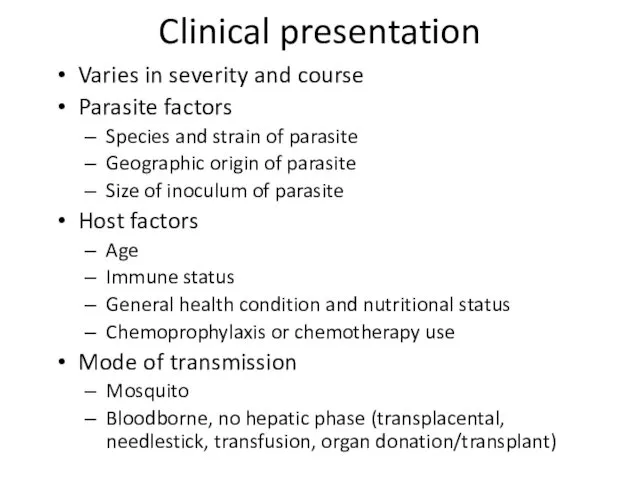
- 15. Clinical presentation Varies in severity and course Parasite factors Species and strain of parasite Geographic origin
- 16. Malarial Paroxysm Periodicity Days 1 and 3 for P.v., P.o., (and P.f.) - tertian Usually persistent
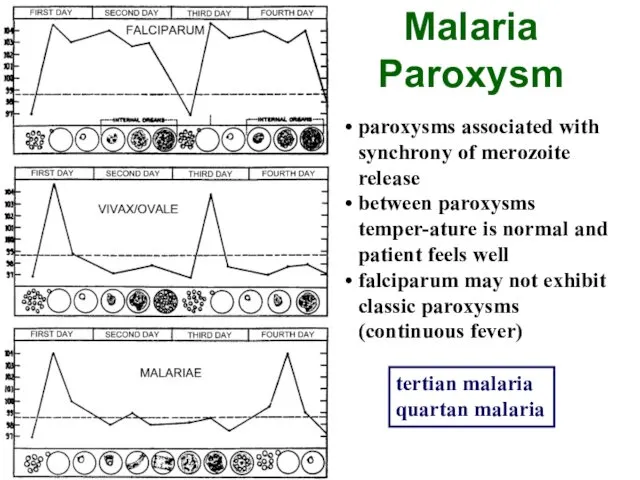
- 17. paroxysms associated with synchrony of merozoite release between paroxysms temper-ature is normal and patient feels well
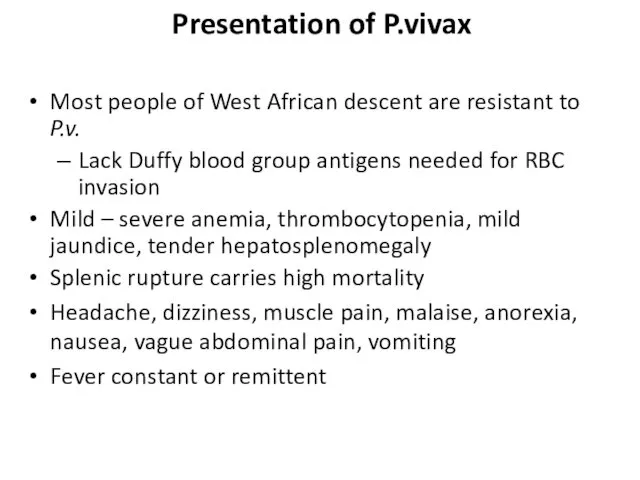
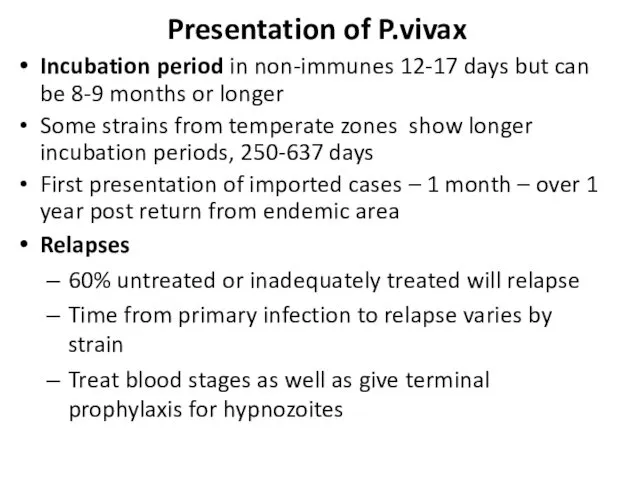
- 18. Presentation of P.vivax Most people of West African descent are resistant to P.v. Lack Duffy blood
- 19. Incubation period in non-immunes 12-17 days but can be 8-9 months or longer Some strains from
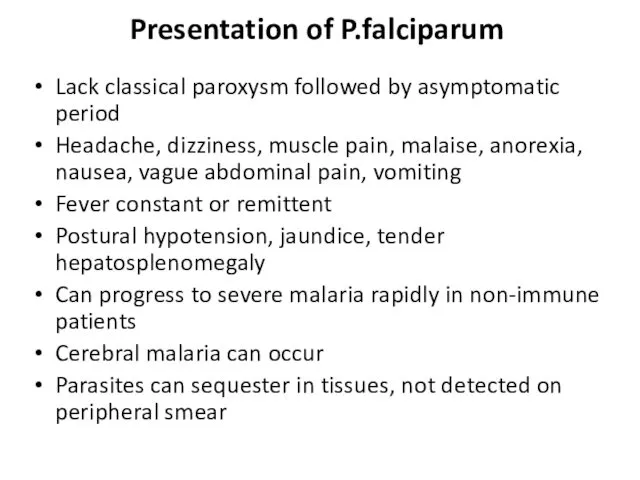
- 21. Lack classical paroxysm followed by asymptomatic period Headache, dizziness, muscle pain, malaise, anorexia, nausea, vague abdominal
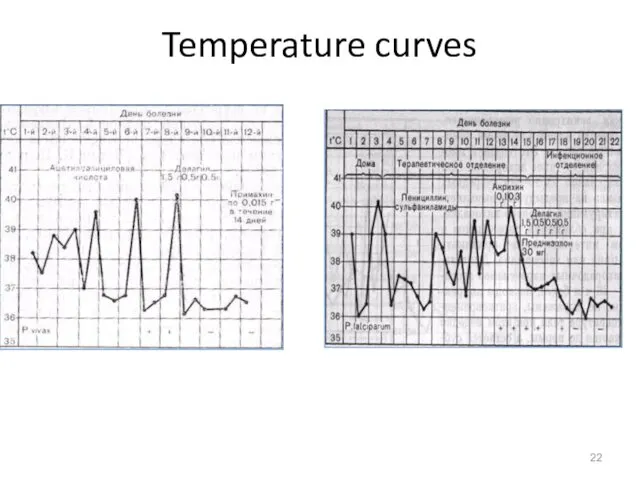
- 22. Temperature curves
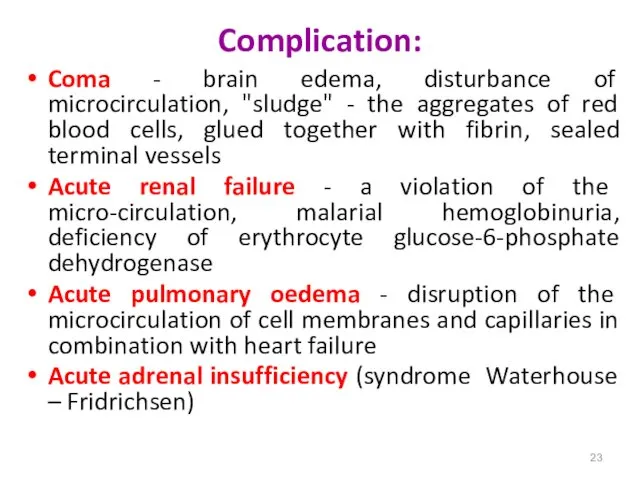
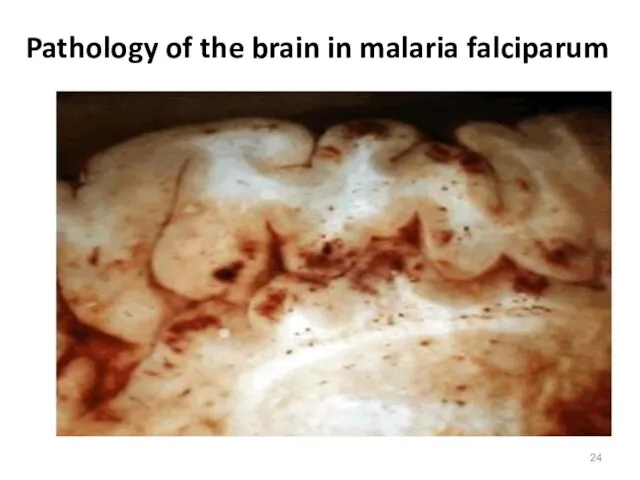
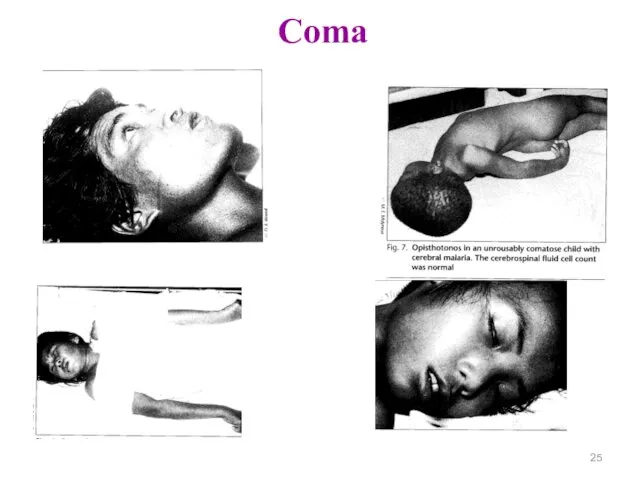
- 23. Complication: Coma - brain edema, disturbance of microcirculation, "sludge" - the aggregates of red blood cells,
- 24. Pathology of the brain in malaria falciparum
- 25. Coma
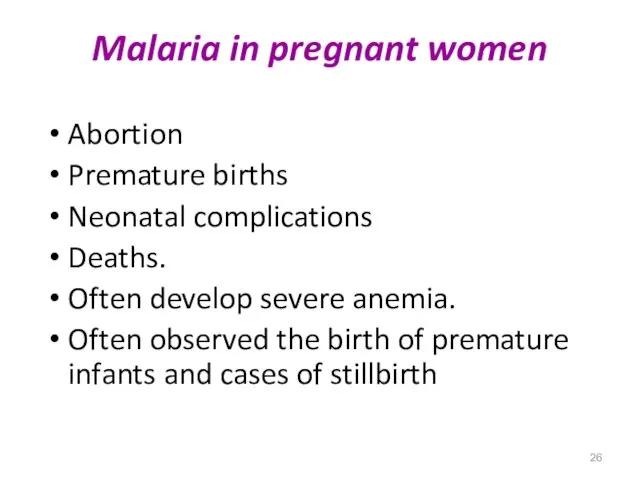
- 26. Malaria in pregnant women Abortion Premature births Neonatal complications Deaths. Often develop severe anemia. Often observed
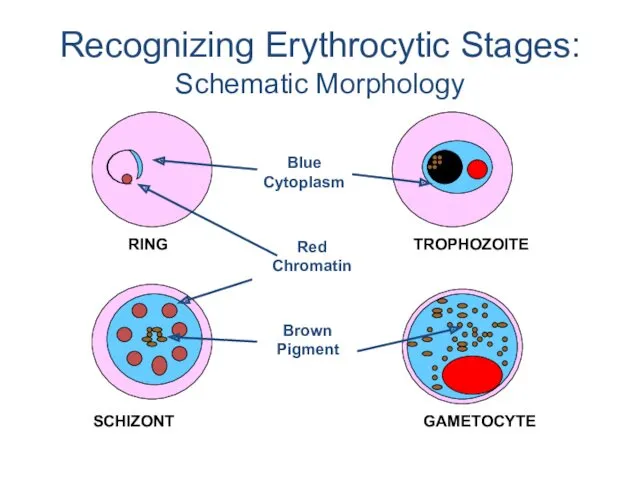
- 27. Recognizing Erythrocytic Stages: Schematic Morphology
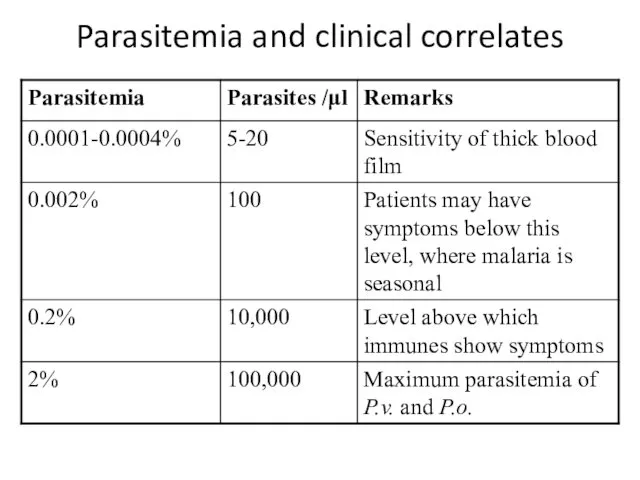
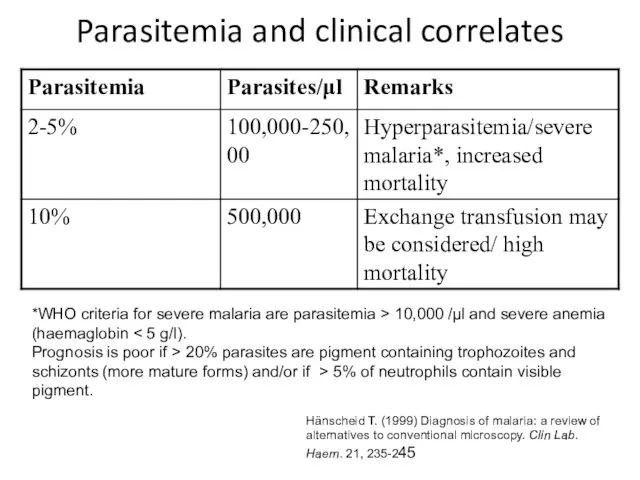
- 28. Parasitemia and clinical correlates
- 29. Parasitemia and clinical correlates *WHO criteria for severe malaria are parasitemia > 10,000 /μl and severe
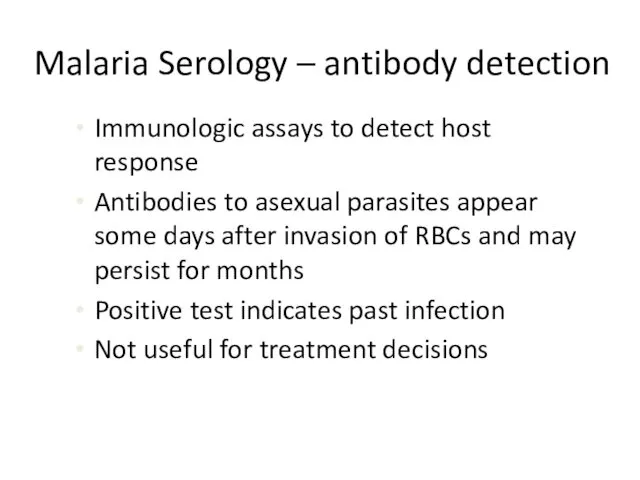
- 36. Malaria Serology – antibody detection Immunologic assays to detect host response Antibodies to asexual parasites appear
- 37. Malaria Serology – antibody detection Valuable epidemiologic tool in some settings Useful for Identifying infective donor
- 38. Polymerase Chain Reaction (PCR) Molecular technique to identify parasite genetic material Uses whole blood collected in
- 40. Скачать презентацию



 Қанның тасымалдаушы липопротеиндерінің құрамы, құрылысы және жіктелуі
Қанның тасымалдаушы липопротеиндерінің құрамы, құрылысы және жіктелуі Задачи принципы организации диетического питания
Задачи принципы организации диетического питания Ерте кезеңдегі ұлы дәрігерлер
Ерте кезеңдегі ұлы дәрігерлер Chronic gastritis
Chronic gastritis Болевой синдром и его лечение в ОВП
Болевой синдром и его лечение в ОВП Коматозды жағдайлардың патофизиологиясы
Коматозды жағдайлардың патофизиологиясы Медициналық сұхбаттасу техникасы
Медициналық сұхбаттасу техникасы Анемия. Эритроциттердің формасы мен көлемі
Анемия. Эритроциттердің формасы мен көлемі Хронические обструктивные заболевания легких. Бронхиты
Хронические обструктивные заболевания легких. Бронхиты Лекция 11. Ненаркотические анальгетики
Лекция 11. Ненаркотические анальгетики Основы психосоматики и психологии больного. Сестринское дело. Переподготовка
Основы психосоматики и психологии больного. Сестринское дело. Переподготовка Профилактика ВИЧ-инфекции. СПИД
Профилактика ВИЧ-инфекции. СПИД Ошибки и осложнения после протезирования на имплантатах. Гигиенические мероприятия при наличии в полости рта имплантатов
Ошибки и осложнения после протезирования на имплантатах. Гигиенические мероприятия при наличии в полости рта имплантатов Роль гормонов в обменных процессах, нервно-гуморальная регуляция, её нарушения
Роль гормонов в обменных процессах, нервно-гуморальная регуляция, её нарушения Внутривенные наркотики. Героиновая наркомания. Заменители героина
Внутривенные наркотики. Героиновая наркомания. Заменители героина Опыт хирургического лечения опухолей надпочечников у детей
Опыт хирургического лечения опухолей надпочечников у детей ЭКГ - диагностика при подозрении на инфаркт миокарда
ЭКГ - диагностика при подозрении на инфаркт миокарда Отравление алкоголем и его суррогатами
Отравление алкоголем и его суррогатами NIR
NIR Acquired Immunodeficiency syndrome
Acquired Immunodeficiency syndrome Особенности ведения преждевременных родов
Особенности ведения преждевременных родов Общая характеристика и эпидемиология новообразований ЛОР-органов
Общая характеристика и эпидемиология новообразований ЛОР-органов Цукровий діабет у дітей
Цукровий діабет у дітей Особенности капсульной эндоскопии
Особенности капсульной эндоскопии Дезинфекционные мероприятия при новой коронавирусной инфекции (2019-nCoV)
Дезинфекционные мероприятия при новой коронавирусной инфекции (2019-nCoV) Травмы. Травматический шок
Травмы. Травматический шок Методические указания по приготовлению дезинфицирующим растворов. Отбор проб дезинфектантов
Методические указания по приготовлению дезинфицирующим растворов. Отбор проб дезинфектантов Общий алгоритм подбора очковой коррекции
Общий алгоритм подбора очковой коррекции