Содержание
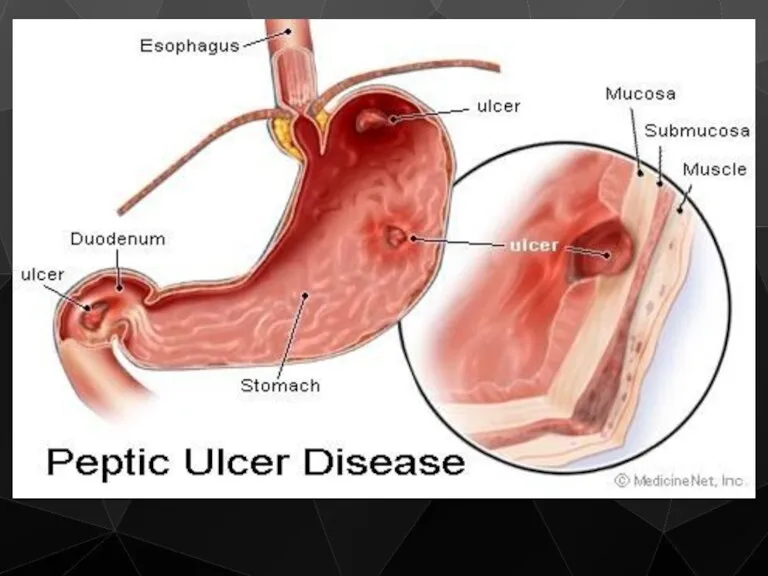
- 2. A peptic ulcer is an open sore in the upper digestive tract. There are two types
- 4. Classification Stomach (called gastric ulcer) Duodenum (called duodenal ulcer) Oesophagus (called Oesophageal ulcer) Types of peptic
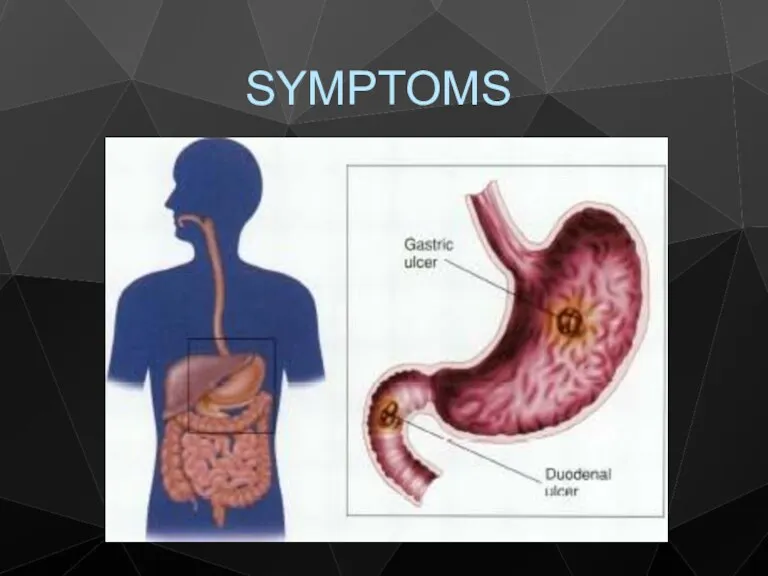
- 5. SYMPTOMS
- 7. CAUSES
- 8. Helicobacter pylori, a bacteria that is frequently found in the stomach Nonsteroidal anti-inflammatory drugs (NSAIDS) such
- 9. Helicobacter pylori infection H. pylori is a helix-shaped Gram-negative, slow-growing organism
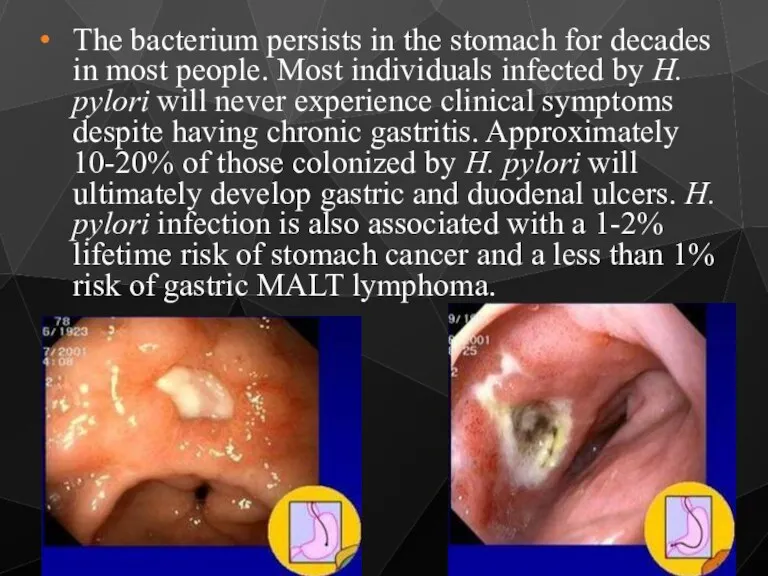
- 10. The bacterium persists in the stomach for decades in most people. Most individuals infected by H.
- 11. Effects of smoking on PUD Increased rate of gastric emptying Diminished pancreatic bicarbonate secretion Decreased duodenal
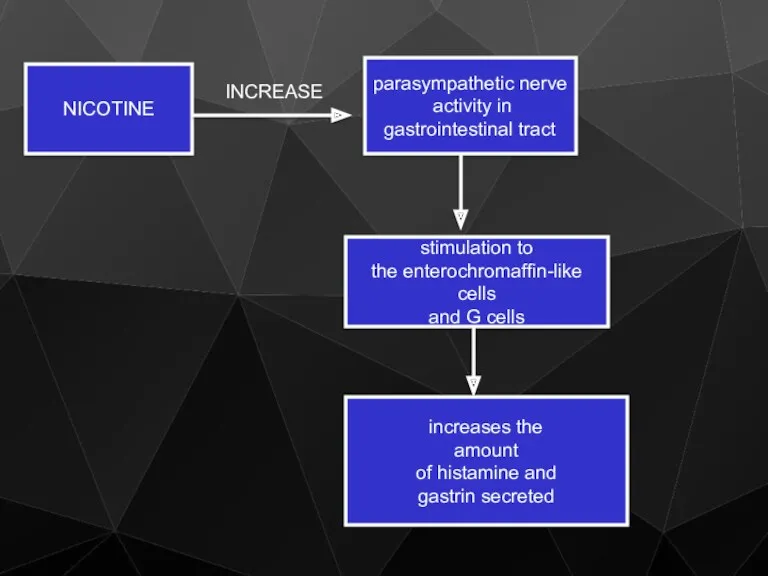
- 12. NICOTINE parasympathetic nerve activity in gastrointestinal tract INCREASE stimulation to the enterochromaffin-like cells and G cells
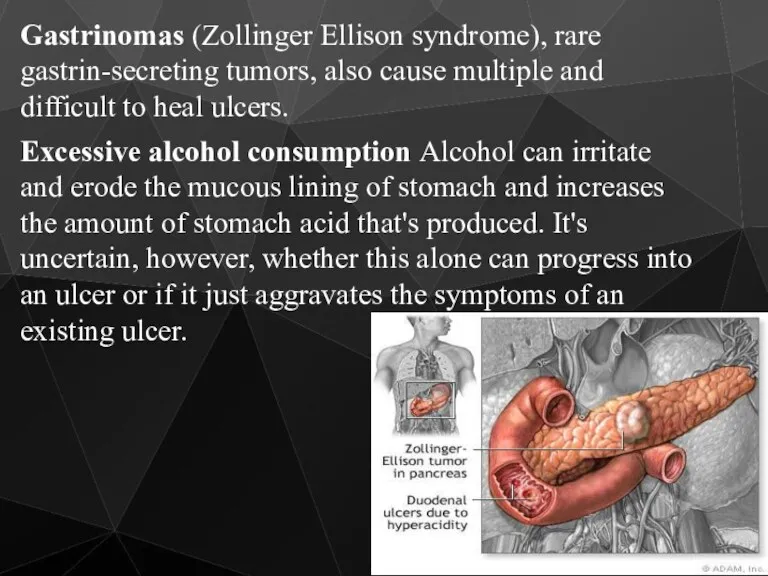
- 13. Gastrinomas (Zollinger Ellison syndrome), rare gastrin-secreting tumors, also cause multiple and difficult to heal ulcers. Excessive
- 14. Caffeine Beverages and foods that contain caffeine can stimulate acid secretion in the stomach. This can
- 15. The complications of Peptic Ulceration The common complications are: Perforation Penetration Bleeding Stenosis
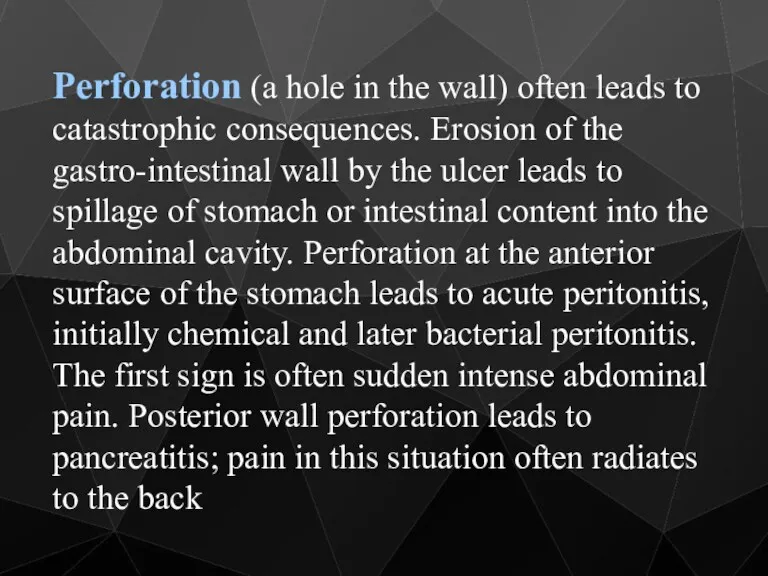
- 16. Perforation (a hole in the wall) often leads to catastrophic consequences. Erosion of the gastro-intestinal wall
- 17. Perforation Clinical Features History of peptic ulcer Sudden onset, severe, generalized abdominal pain Starts as chemical
- 18. Perforation Clinical symptoms Tachycardia, pyrexia Shock Board like rigidity of abdomen Abdominal splinting
- 19. Perforation Clinical Features In elderly, the classical presentation of PPU may be absent Use of NSAID
- 20. Perforation Clinical Features The most frequent place for perforation is the anterior wall of duodenum Anterior
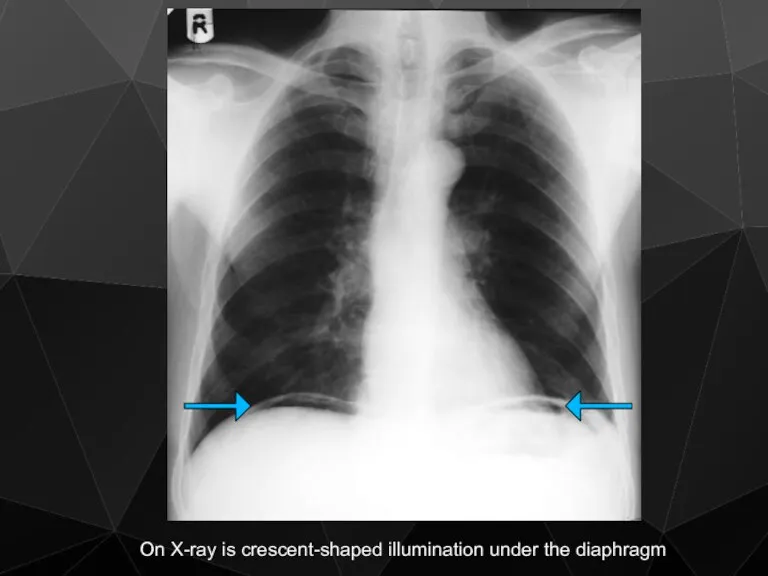
- 21. Perforation Investigations Observe chest X-ray will reveal free gas under the diaphragm in more than 50%
- 22. On X-ray is crescent-shaped illumination under the diaphragm
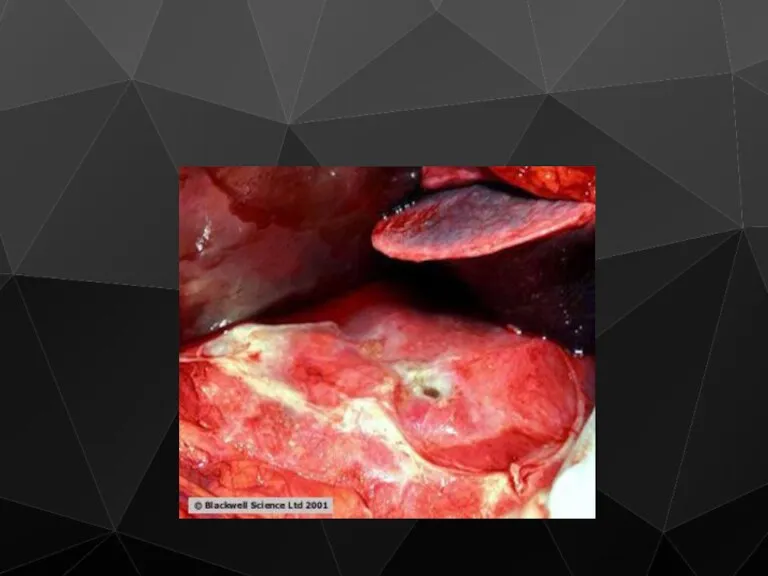
- 23. Perforation Treatment Hospitalisation and analgesia The treatment is principally surgical Midline laparotomy Thorough peritoneal toilet Duodenal
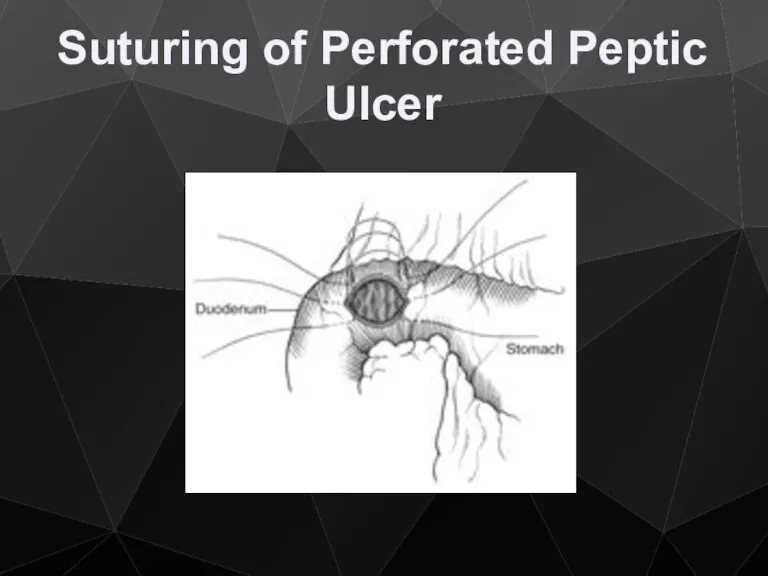
- 26. Suturing of Perforated Peptic Ulcer
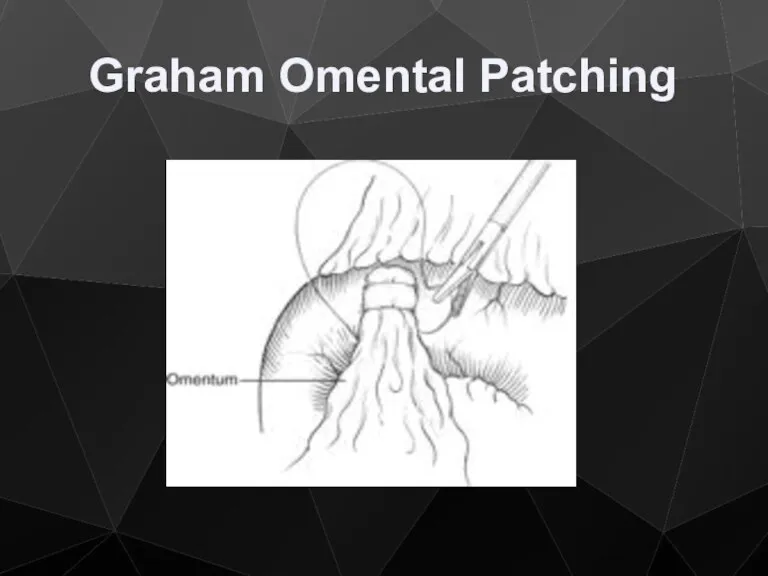
- 27. Graham Omental Patching
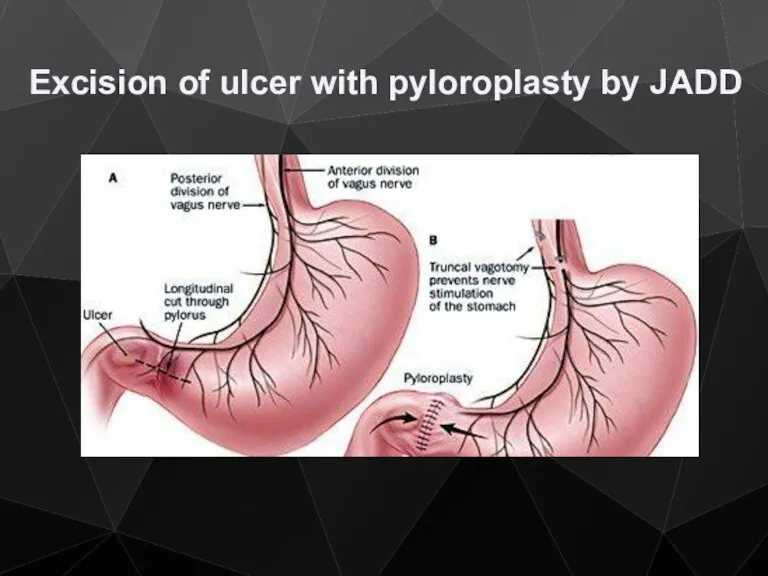
- 28. Excision of ulcer with pyloroplasty by JADD
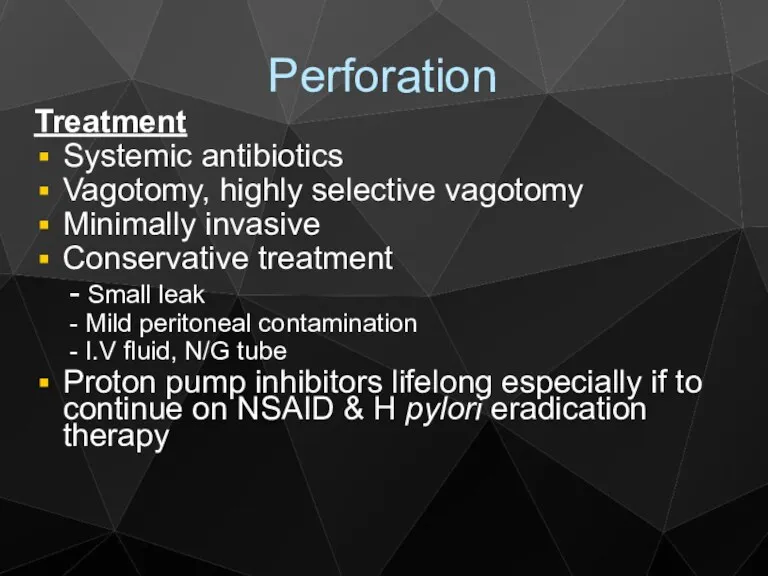
- 29. Perforation Treatment Systemic antibiotics Vagotomy, highly selective vagotomy Minimally invasive Conservative treatment - Small leak -
- 30. Gastrointestinal bleeding is the most common complication. Sudden large bleeding can be life-threatening. It occurs when
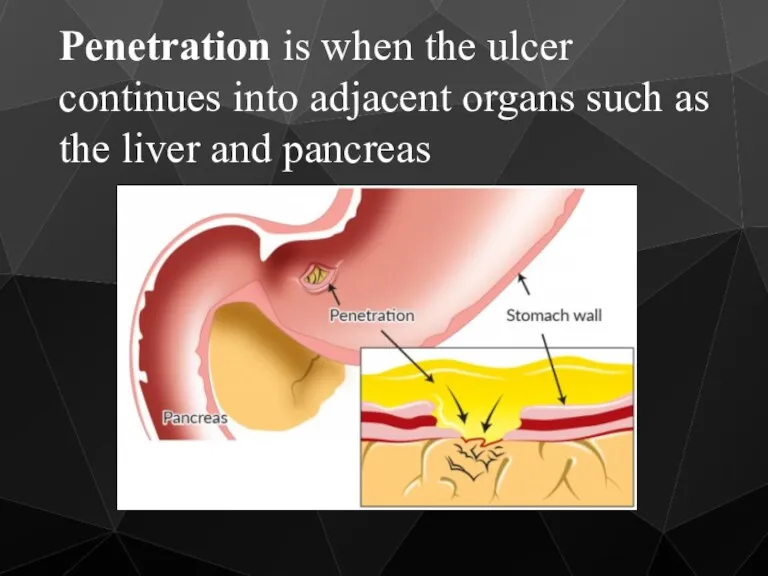
- 31. Penetration is when the ulcer continues into adjacent organs such as the liver and pancreas
- 32. Penetration is a form of perforation in which the perforating ulcers erode the whole thickness of
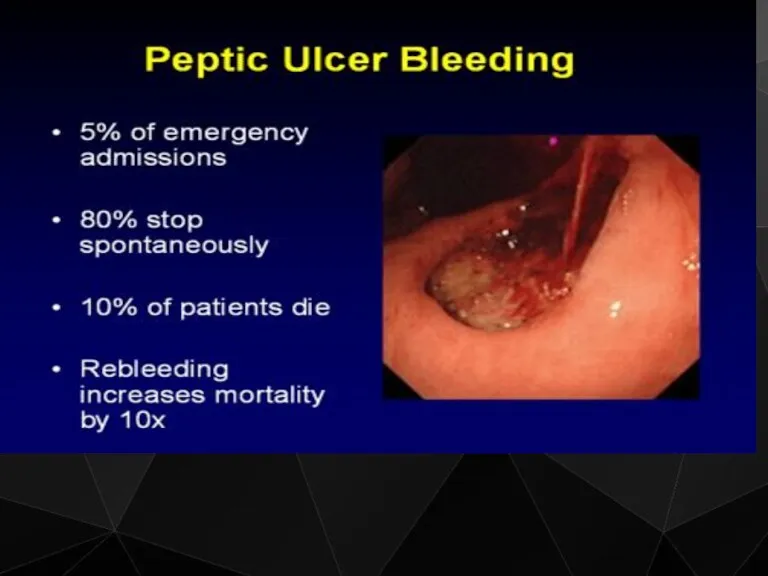
- 33. Bleeding Epidemiology Mirror that of PPU NSAID
- 34. Bleeding
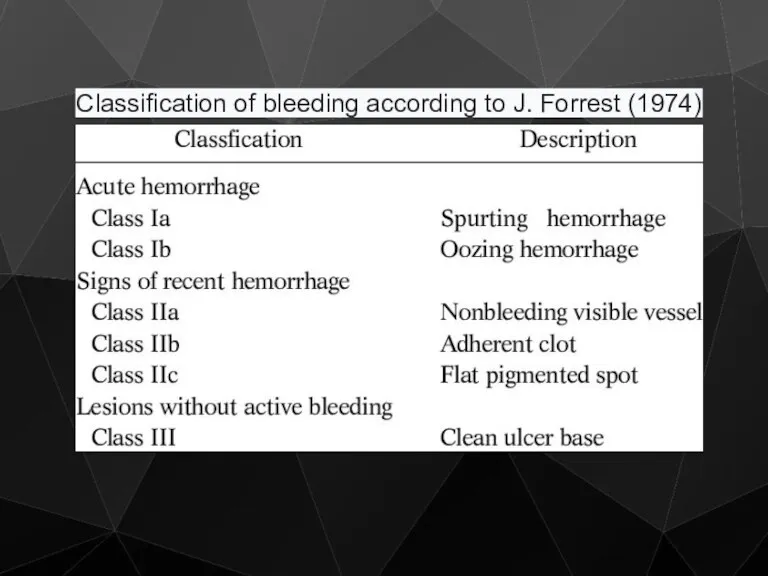
- 35. Classification of bleeding according to J. Forrest (1974)
- 36. Bleeding Treatment / Medical Limited efficacy All patients are started on PPI (omeprasole) Endoscopic control -
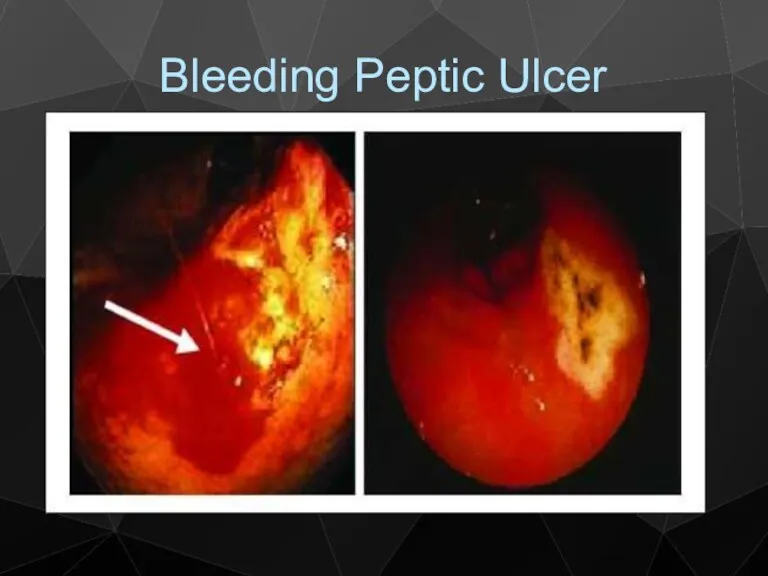
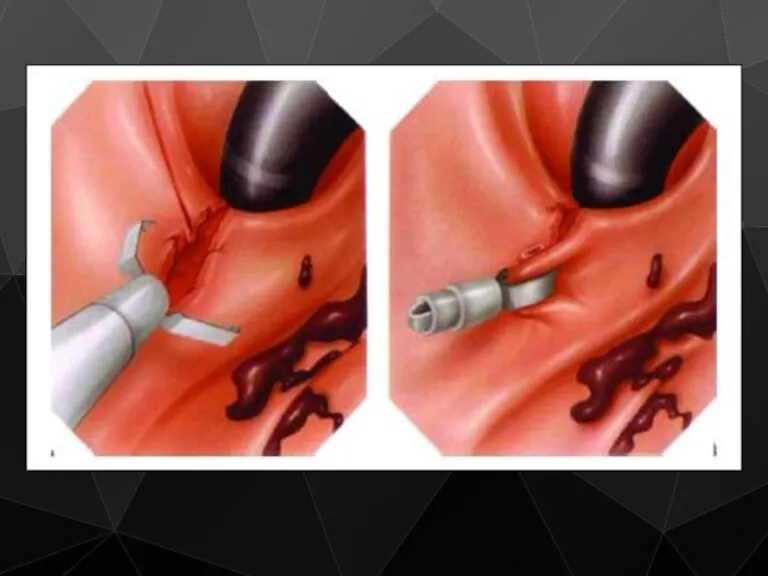
- 37. Bleeding Peptic Ulcer
- 39. Bleeding Treatment / Surgical Indications Patient continue to bleed Visible vessel in ulcer base Spurting vessel
- 40. Bleeding Treatment / Surgical Aim to stop bleeding Upper midline incision Site usually localized by prior
- 41. Bleeding Treatment / Surgical Definitive acid lowering surgery is not required PPI (omeprasole) Anti H pylori
- 42. Stenosis Stenosis is usually found in the 1st part of duodenum This condition occurs less and
- 43. Scar tissue Scarring and swelling due to ulcers causes narrowing in the duodenum and gastric outlet
- 45. Stenosis Clinical Features Long history of peptic ulcer disease Vomiting, unpleasant in nature, totally lacking in
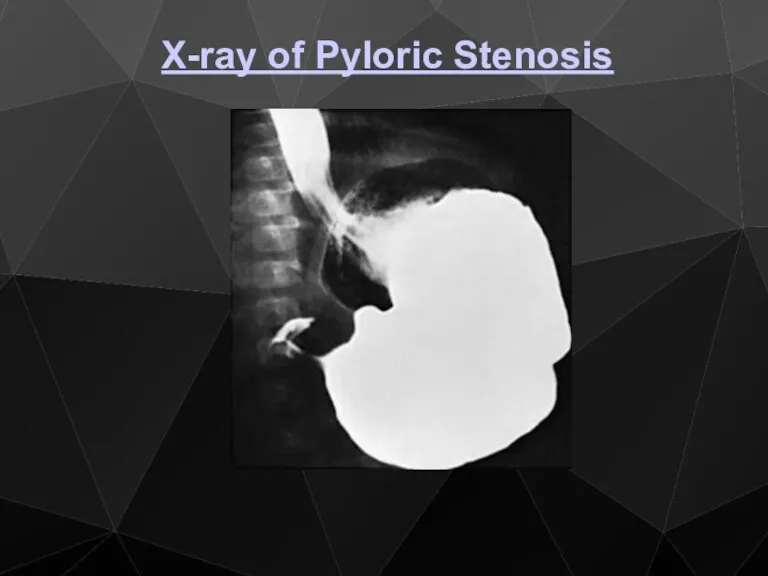
- 46. X-ray of Pyloric Stenosis
- 47. Stenosis Metabolic effects Vomiting of HCl results in hypochloremic acidosis Initially Na+ & K+ levels are
- 48. Stenosis Metabolic effects Then because of dehydration, a phase of Na+ retention follows and K+ and
- 49. Stenosis Management 1) Correct metabolic abnormality Rehydration with isotonic saline with K + supplementation Replacing NaCl
- 50. Stenosis Management 2) Empty the stomach with wide-bore N/G tube, may need lavage 3) Endoscopy and
- 51. Stenosis Management Early cases may settle with conservative measurement, presumably as the edema around the ulcer
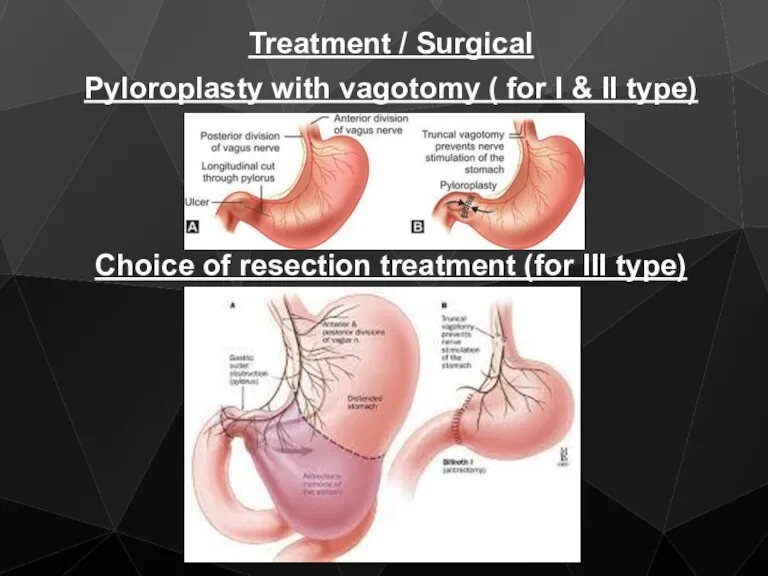
- 52. Treatment / Surgical Pyloroplasty with vagotomy ( for I & II type) Choice of resection treatment
- 54. Скачать презентацию





 Hygiene of work
Hygiene of work Общественное здоровье и организация здравоохранения как наука и предмет преподавания
Общественное здоровье и организация здравоохранения как наука и предмет преподавания Сенсорные нарушения, их коррекция и реабилитация (речевые, зрительные и другие)
Сенсорные нарушения, их коррекция и реабилитация (речевые, зрительные и другие) Антибактериальные химиотерапевтические средства. Антибиотики разных групп
Антибактериальные химиотерапевтические средства. Антибиотики разных групп Правила клинического использования донорской крови и (или) ее компонентов
Правила клинического использования донорской крови и (или) ее компонентов Менингококковая инфекция
Менингококковая инфекция Мукополисахаридоз
Мукополисахаридоз Диагностика беременности. Методы акушерского исследования (урок 3)
Диагностика беременности. Методы акушерского исследования (урок 3) Митральді клапанның минимальді-инвазивті оң жақтық торактомия өткізілген хирургияның ерте және ұзақ мерзімді
Митральді клапанның минимальді-инвазивті оң жақтық торактомия өткізілген хирургияның ерте және ұзақ мерзімді Клизмы. Классификация клизм как процедур
Клизмы. Классификация клизм как процедур Организация работы в специализированных бригадах скорой помощи
Организация работы в специализированных бригадах скорой помощи Механизмы отторжения трапсплантата на примере трансплантации сердца
Механизмы отторжения трапсплантата на примере трансплантации сердца Анатомия и физиология как медицинские науки. Человек как предмет изучения анатомии и физиологии. Лекция № 1
Анатомия и физиология как медицинские науки. Человек как предмет изучения анатомии и физиологии. Лекция № 1 Основные принципы местной анестезии в стоматологии. Оперативная хирургия и топографическая анатомия ЧЛО
Основные принципы местной анестезии в стоматологии. Оперативная хирургия и топографическая анатомия ЧЛО Производственная практика 2018-2019
Производственная практика 2018-2019 Сосудистые заболевания нервной системы
Сосудистые заболевания нервной системы Медициналық клиникалық зерттеулердің дизайны
Медициналық клиникалық зерттеулердің дизайны Опухоли (новообразования)
Опухоли (новообразования) Методы лечения психофармакотерапии с позиции доказательной медицины
Методы лечения психофармакотерапии с позиции доказательной медицины Менингококковая инфекция
Менингококковая инфекция Микрохирургия. Планирование восстановительных операций
Микрохирургия. Планирование восстановительных операций Итальянский метод ринопластики
Итальянский метод ринопластики Инновационные методы лечения головной боли
Инновационные методы лечения головной боли Исследование мочи
Исследование мочи Функциональная анатомия лимфатической системы
Функциональная анатомия лимфатической системы GDP. Склад медикаментов
GDP. Склад медикаментов Световая микроскопия
Световая микроскопия Гипоплазия эмали
Гипоплазия эмали