Содержание
- 2. Plan:
- 3. Functions of the Heart Generating blood pressure Routing blood: separates pulmonary and systemic circulations Ensuring one-way
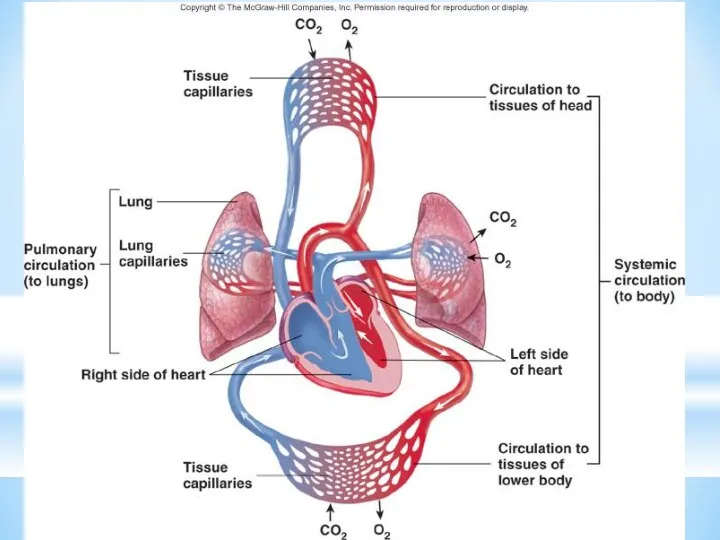
- 4. The cardiovascular system is divided into two circuits Pulmonary circuit blood to and from the lungs
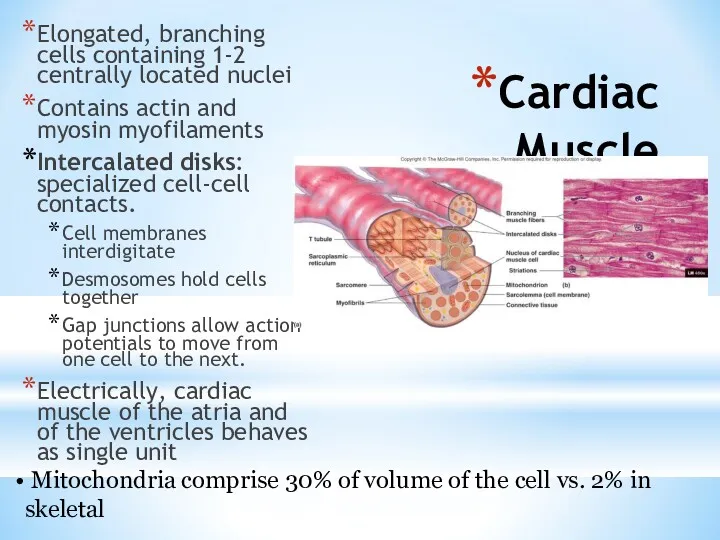
- 6. Cardiac Muscle Elongated, branching cells containing 1-2 centrally located nuclei Contains actin and myosin myofilaments Intercalated
- 7. Heart chambers and valves Structural Differences in heart chambers The left side of the heart is
- 8. Cardiac Muscle Contraction Heart muscle: Is stimulated by nerves and is self-excitable (automaticity) Contracts as a
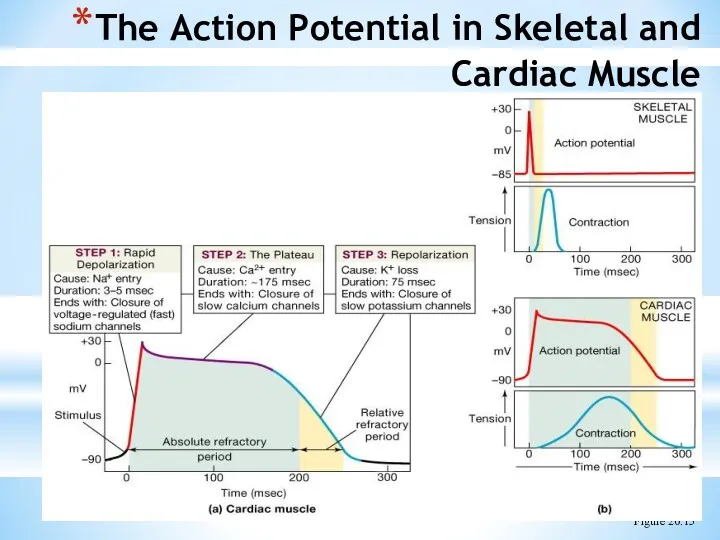
- 9. Differences Between Skeletal and Cardiac Muscle Physiology Action Potential Cardiac: Action potentials conducted from cell to
- 10. The Action Potential in Skeletal and Cardiac Muscle Figure 20.15
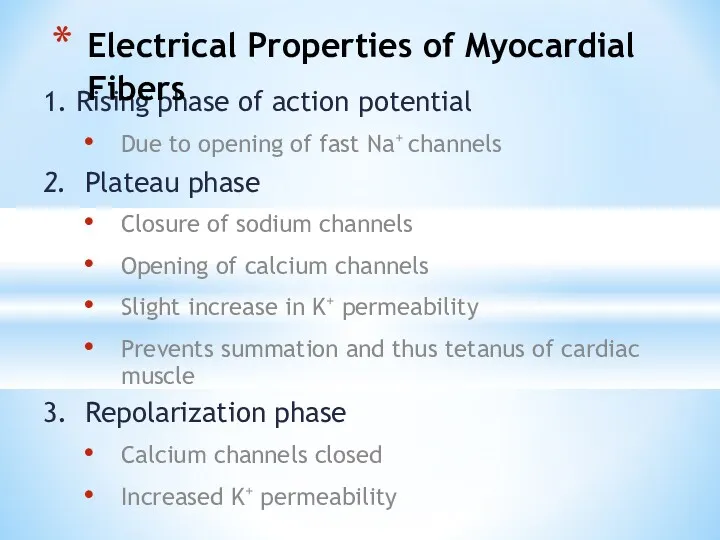
- 11. 1. Rising phase of action potential Due to opening of fast Na+ channels 2. Plateau phase
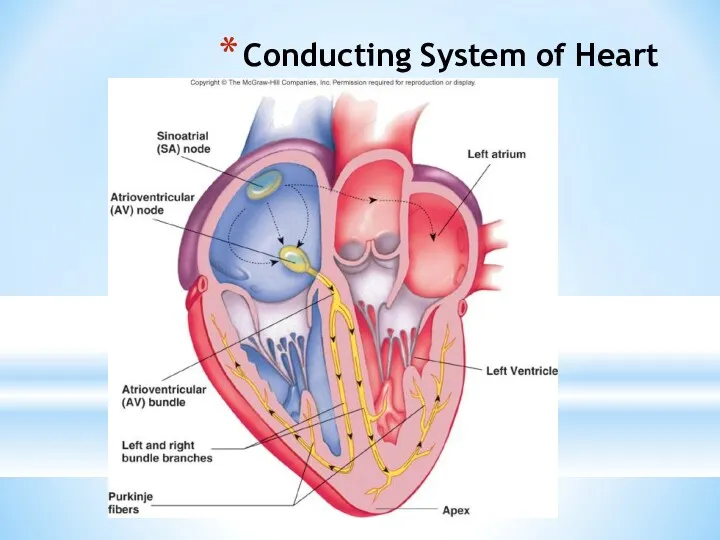
- 12. Conducting System of Heart
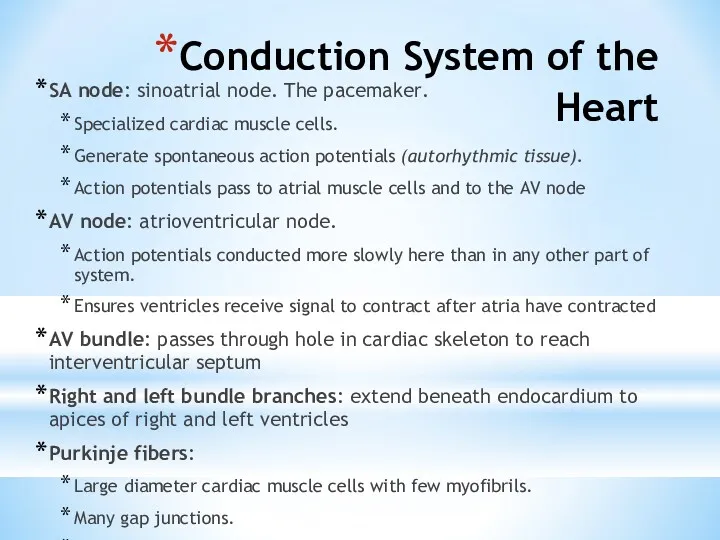
- 13. Conduction System of the Heart SA node: sinoatrial node. The pacemaker. Specialized cardiac muscle cells. Generate
- 14. Heart Physiology: Intrinsic Conduction System Autorhythmic cells: Initiate action potentials Have unstable resting potentials called pacemaker
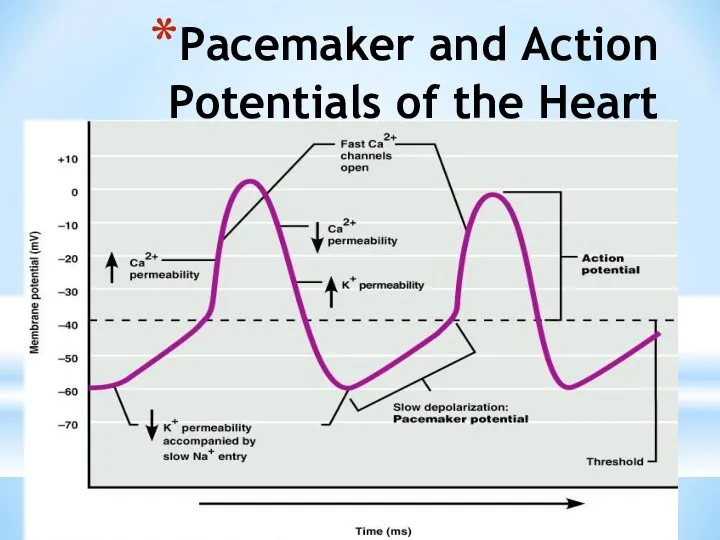
- 15. Depolarization of SA Node SA node - no stable resting membrane potential Pacemaker potential gradual depolarization
- 16. Pacemaker and Action Potentials of the Heart
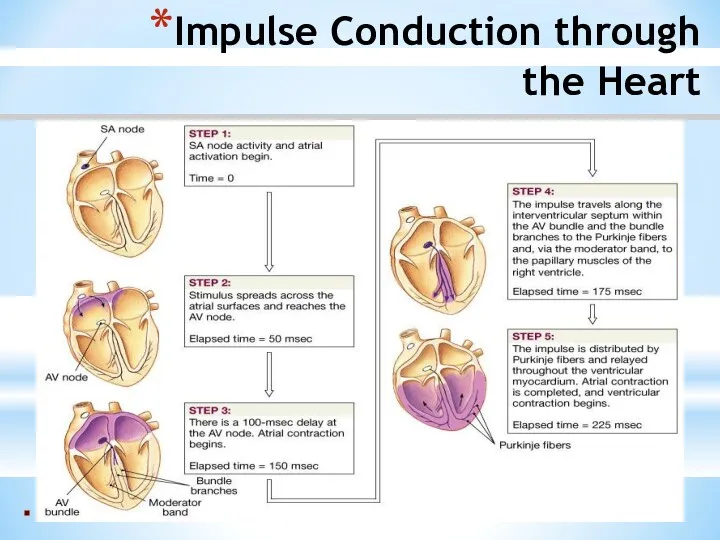
- 17. Heart Physiology: Sequence of Excitation Sinoatrial (SA) node generates impulses about 75 times/minute Atrioventricular (AV) node
- 18. Impulse Conduction through the Heart
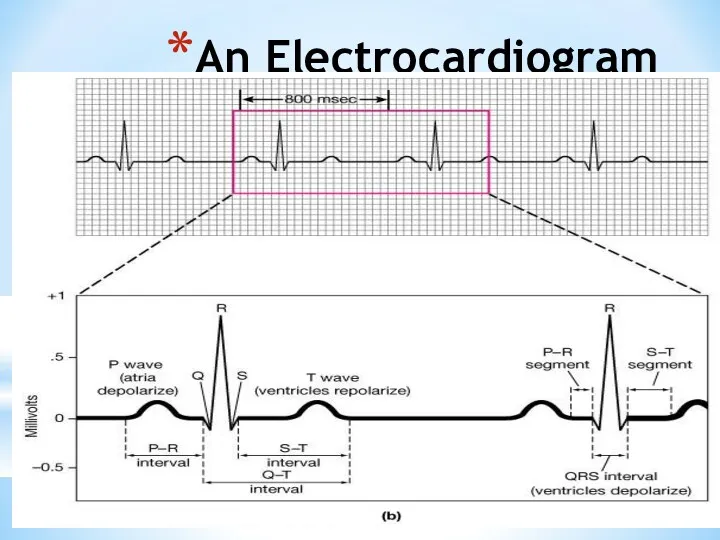
- 19. An Electrocardiogram
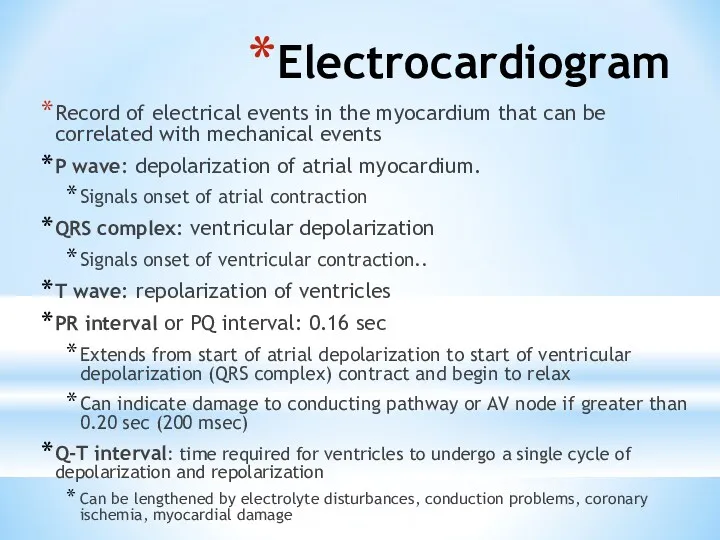
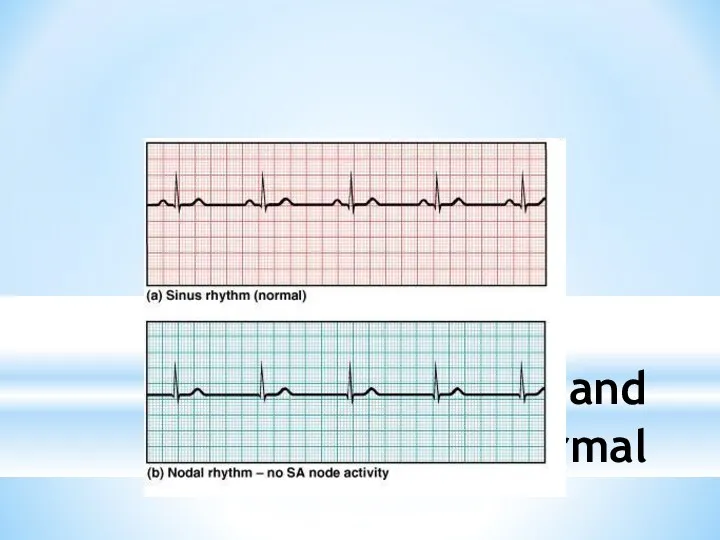
- 20. Electrocardiogram Record of electrical events in the myocardium that can be correlated with mechanical events P
- 21. ECGs, Normal and Abnormal
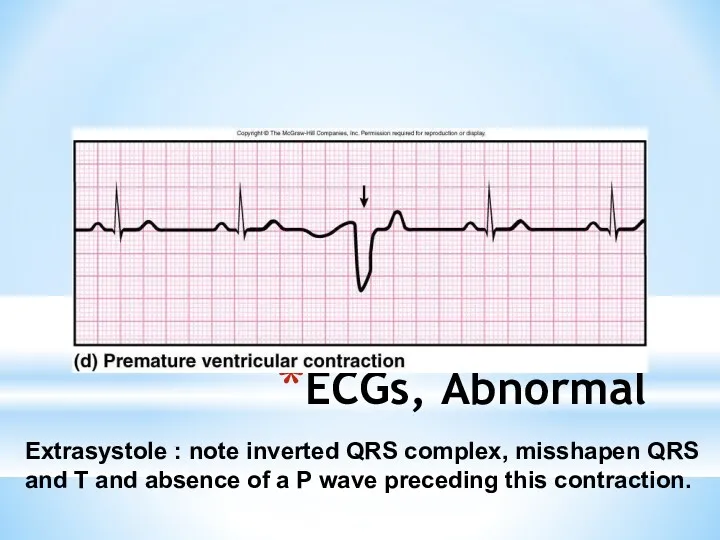
- 22. ECGs, Abnormal Extrasystole : note inverted QRS complex, misshapen QRS and T and absence of a
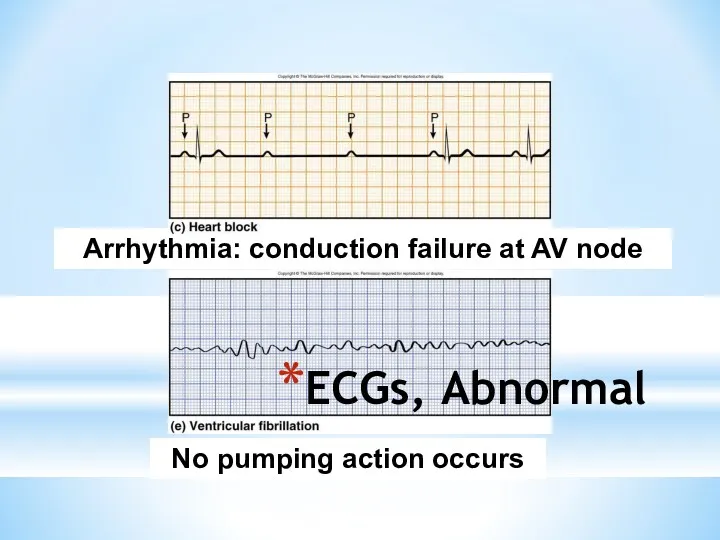
- 23. ECGs, Abnormal Arrhythmia: conduction failure at AV node No pumping action occurs
- 24. The Cardiac Cycle Cardiac cycle refers to all events associated with blood flow through the heart
- 25. Phases of the Cardiac Cycle Atrial diastole and systole - Blood flows into and passively out
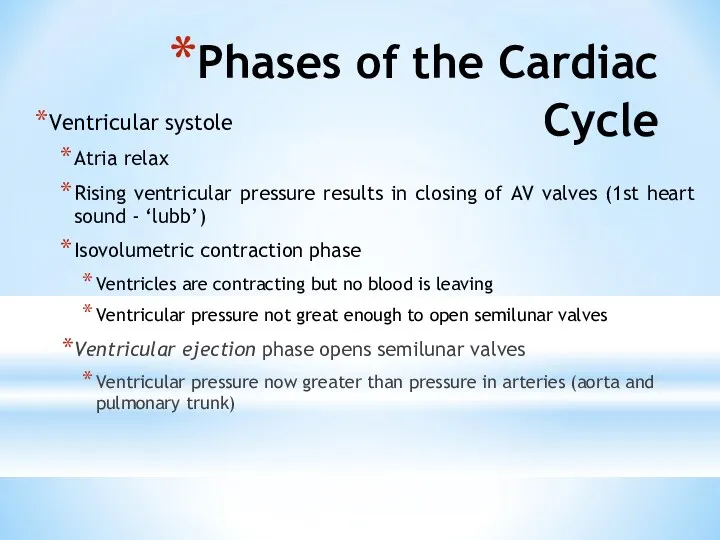
- 26. Phases of the Cardiac Cycle Ventricular systole Atria relax Rising ventricular pressure results in closing of
- 27. Phases of the Cardiac Cycle Ventricular diastole Ventricles relax Backflow of blood in aorta and pulmonary
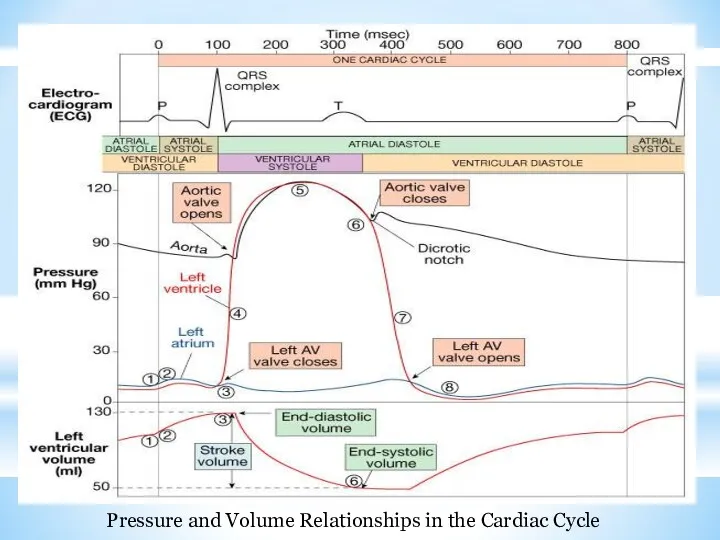
- 28. Pressure and Volume Relationships in the Cardiac Cycle
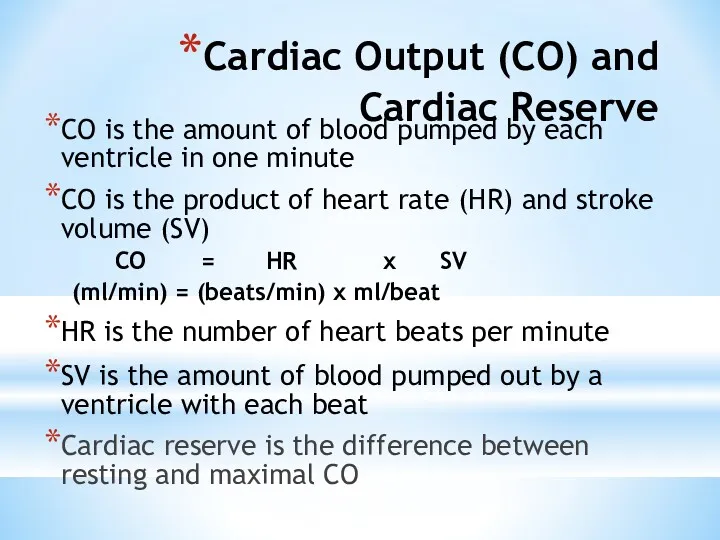
- 29. Cardiac Output (CO) and Cardiac Reserve CO is the amount of blood pumped by each ventricle
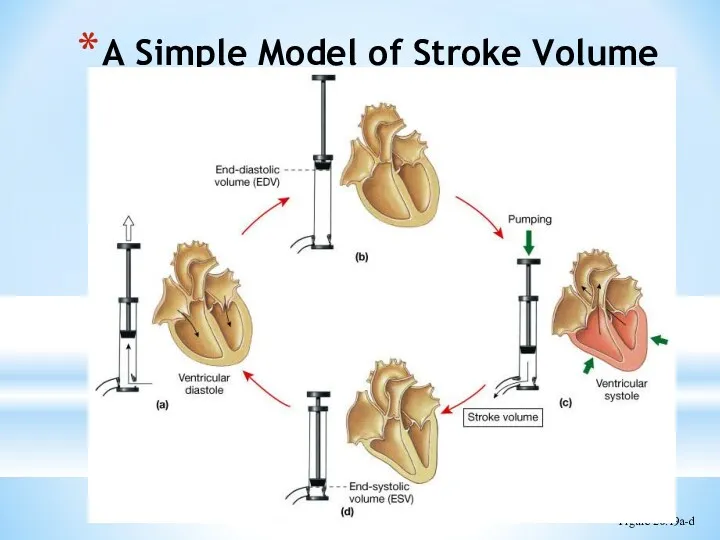
- 30. A Simple Model of Stroke Volume Figure 20.19a-d
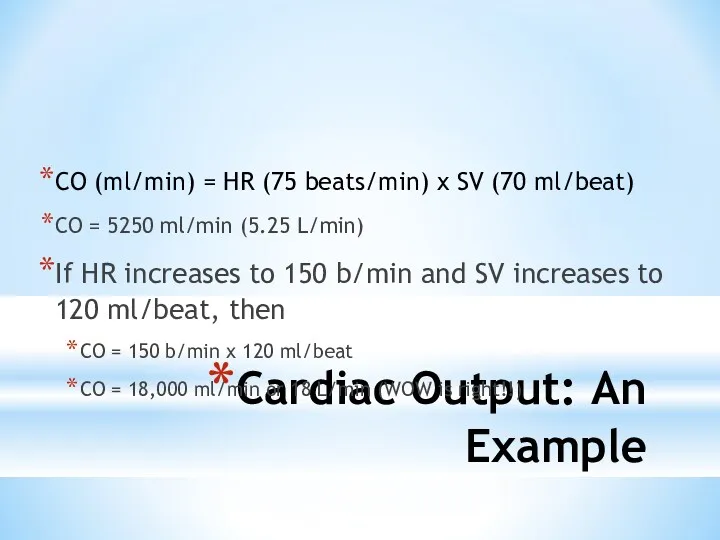
- 31. Cardiac Output: An Example CO (ml/min) = HR (75 beats/min) x SV (70 ml/beat) CO =
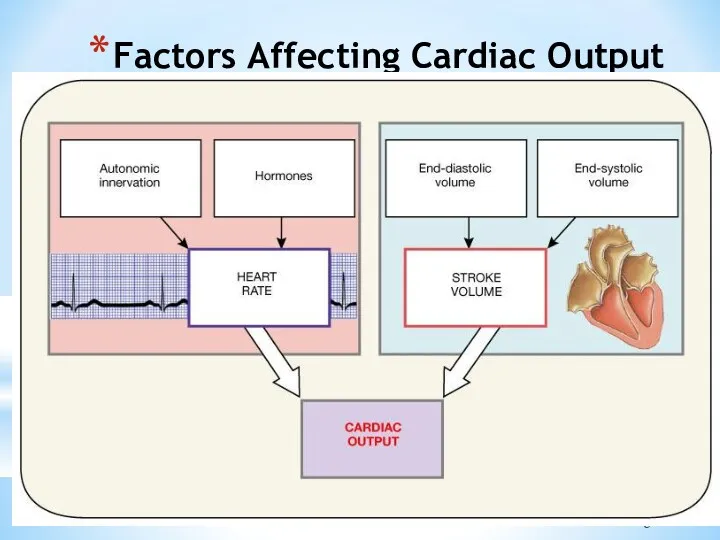
- 32. Factors Affecting Cardiac Output Figure 20.20
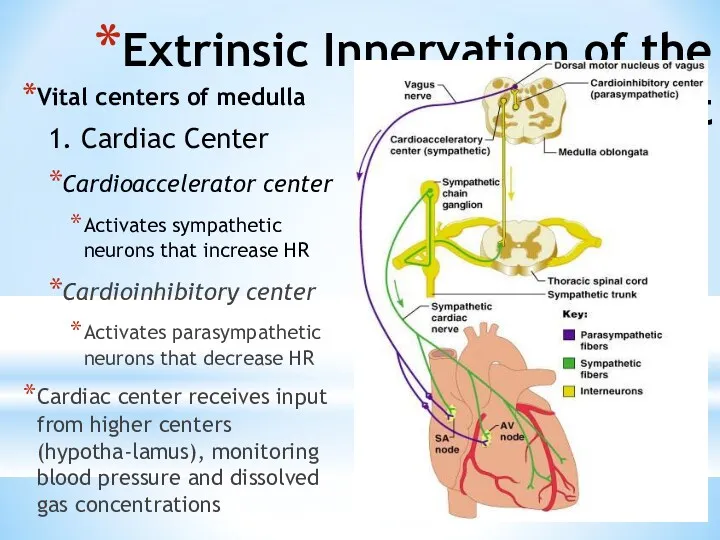
- 33. Extrinsic Innervation of the Heart Vital centers of medulla 1. Cardiac Center Cardioaccelerator center Activates sympathetic
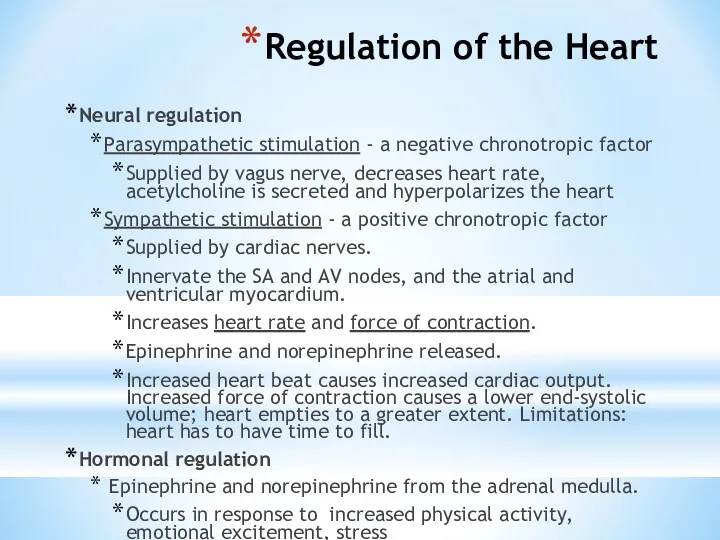
- 34. Regulation of the Heart Neural regulation Parasympathetic stimulation - a negative chronotropic factor Supplied by vagus
- 35. Basic heart rate established by pacemaker cells SA node establishes baseline (sinus rhythmn) Modified by ANS
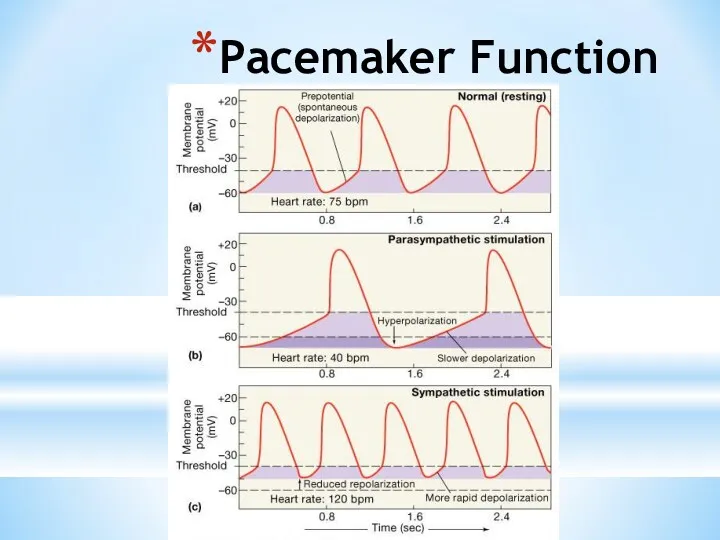
- 36. Pacemaker Function
- 37. Chemical Regulation of the Heart The hormones epinephrine and thyroxine increase heart rate Intra- and extracellular
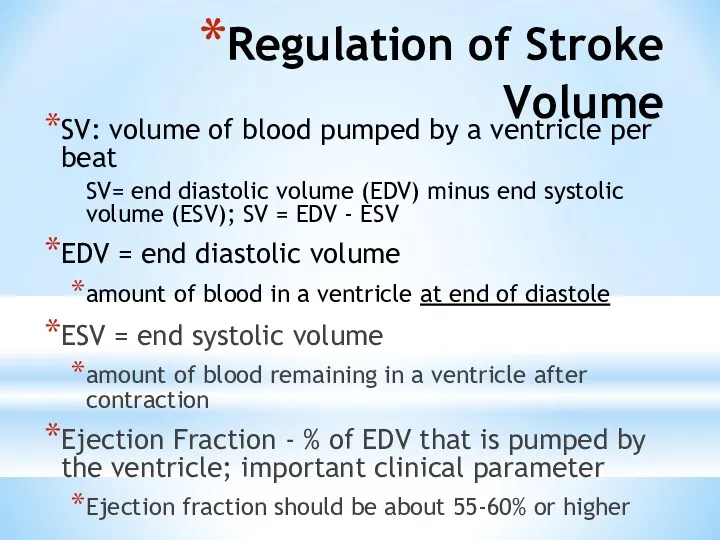
- 38. Regulation of Stroke Volume SV: volume of blood pumped by a ventricle per beat SV= end
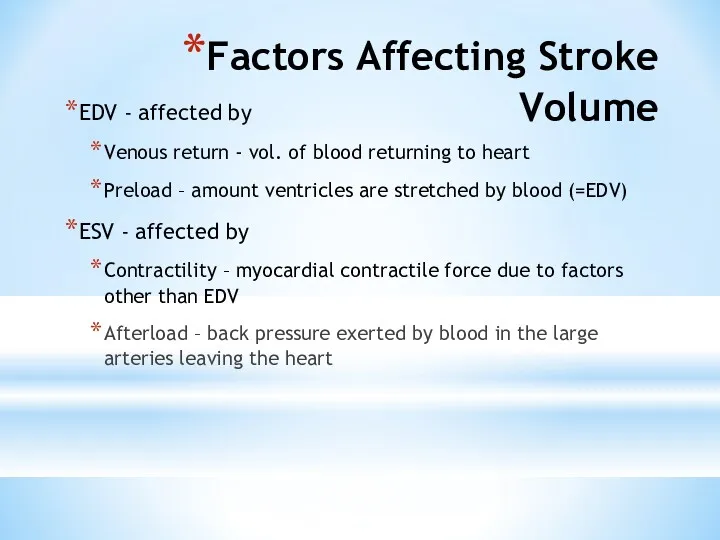
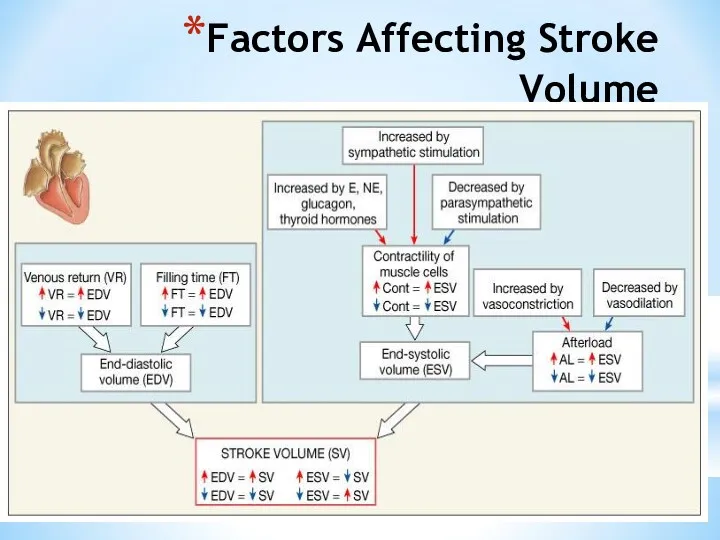
- 39. Factors Affecting Stroke Volume EDV - affected by Venous return - vol. of blood returning to
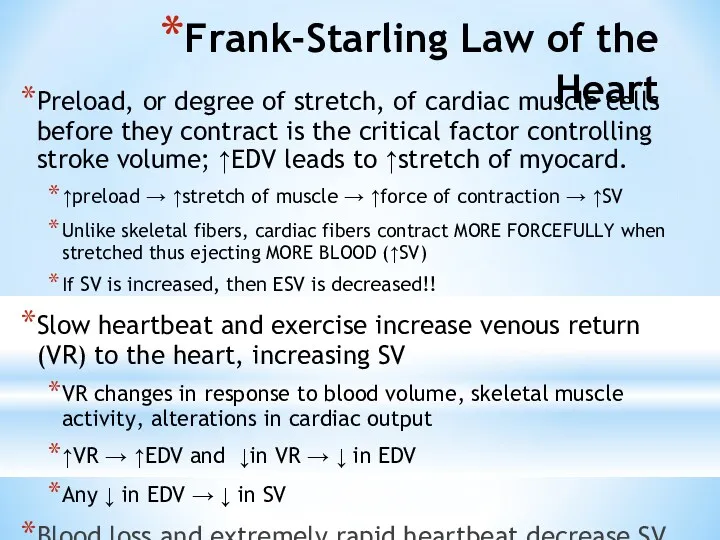
- 40. Frank-Starling Law of the Heart Preload, or degree of stretch, of cardiac muscle cells before they
- 41. Factors Affecting Stroke Volume
- 42. Extrinsic Factors Influencing Stroke Volume Contractility is the increase in contractile strength, independent of stretch and
- 43. Effects of Autonomic Activity on Contractility Sympathetic stimulation Release norepinephrine from symp. postganglionic fiber Also, EP
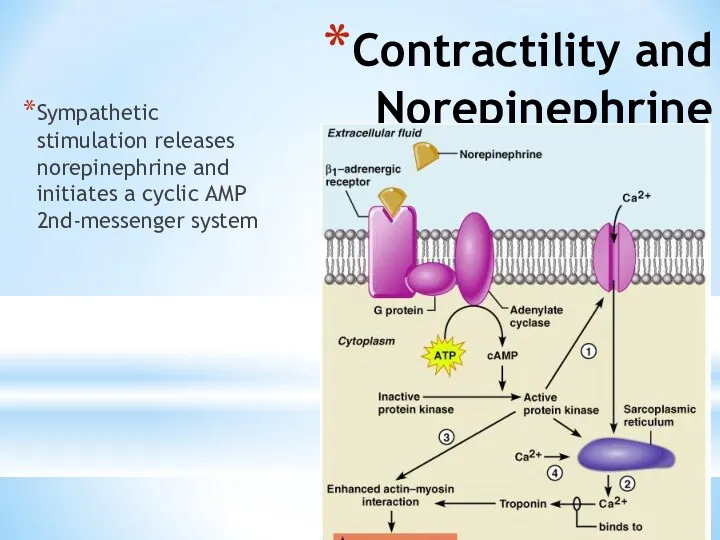
- 44. Contractility and Norepinephrine Sympathetic stimulation releases norepinephrine and initiates a cyclic AMP 2nd-messenger system Figure 18.22
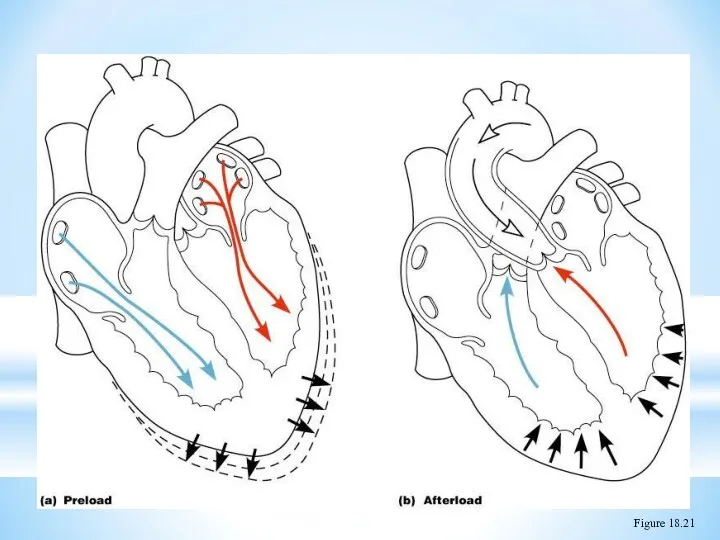
- 45. Preload and Afterload Figure 18.21
- 46. Effects of Hormones on Contractility Epi, NE, and Thyroxine all have positive ionotropic effects and thus
- 48. Скачать презентацию
 Разбор клинического случая
Разбор клинического случая Хронический гастрит
Хронический гастрит Травматические повреждения костей и суставов
Травматические повреждения костей и суставов Принципы нормирования опасных и вредных факторов
Принципы нормирования опасных и вредных факторов Хирургиялык жане тану кабинеті
Хирургиялык жане тану кабинеті Основные проблемы гигиены детей и подростков
Основные проблемы гигиены детей и подростков Экспертиза временной нетрудоспособности терапевтических больных в поликлинике
Экспертиза временной нетрудоспособности терапевтических больных в поликлинике Иммобилизденген ферменттер
Иммобилизденген ферменттер Cестринский уход за новорождёнными при многоплодной беременности
Cестринский уход за новорождёнными при многоплодной беременности Dentists in Canada
Dentists in Canada Частная патологическая анатомия. Болезни ССС
Частная патологическая анатомия. Болезни ССС Adult Nursing Care I
Adult Nursing Care I Ветряная оспа
Ветряная оспа Острые лейкозы. Основные методы исследования при ОЛ
Острые лейкозы. Основные методы исследования при ОЛ Совершенствование системы оплаты труда в здравоохранении - как по-новому запланировать расходы
Совершенствование системы оплаты труда в здравоохранении - как по-новому запланировать расходы Есту және тепе-теңдік мүшесі
Есту және тепе-теңдік мүшесі Инфекциялық емес патологиядағы менингеальды синдром. Туберкулезді менингитпен екшеу диагностикасы
Инфекциялық емес патологиядағы менингеальды синдром. Туберкулезді менингитпен екшеу диагностикасы Балалардың асқазан - ішек аурулары туралы түсінік беру. Балаларда ішек жұқпасының көріністері
Балалардың асқазан - ішек аурулары туралы түсінік беру. Балаларда ішек жұқпасының көріністері Серонегативные спондилоартриты
Серонегативные спондилоартриты Актуальные вопросы профилактики, диагностики коронавирусной инфекции
Актуальные вопросы профилактики, диагностики коронавирусной инфекции Перитонеальный диализ
Перитонеальный диализ Сульфаниламидные препараты
Сульфаниламидные препараты OMS - Organizaţia Mondială a Sănătăţii
OMS - Organizaţia Mondială a Sănătăţii Гепатит С
Гепатит С Бактерия Helicobacter pylori
Бактерия Helicobacter pylori Острая печеночная недостаточность
Острая печеночная недостаточность Термические повреждения
Термические повреждения Жай және күрделі ұнтақтардың дайындалуы. Улы және күшті әсер ететін дәрілік заттары бар ұнтақтардың технологиясы. Тритурация
Жай және күрделі ұнтақтардың дайындалуы. Улы және күшті әсер ететін дәрілік заттары бар ұнтақтардың технологиясы. Тритурация