Содержание
- 2. Upper Respiratory Infections: Otitis Media and Otitis Externa
- 3. Viral Upper Respiratory Infections Rhinovirus most common virus Adenovirus RSV Coronavirus Enteroviruses Children get 6 to
- 4. URI Symptoms Nasal congestion Rhinorrhea Malaise Scratchy or sore throat The nasal discharge typically starts out
- 5. URI Treatment Symptomatic care Fluids, antipyretics Nasal bulb suctioning in infants Decongestants in older children and
- 6. Decongestants Systemic Sympathomimetics Pseudoephedrine Phenylephrine Topical decongestants Phenylephrine (Neosynephrine) Oxymetazoline (Afrin)
- 7. Oral Decongestants Action: vasoconstriction of capillary vessels, theoretically decreasing congestion ADRs Tachycardia Hypertension Anxiety/restlessness/irritability There is
- 8. Cough Suppressants Dextromethorphan Codeine Action: centrally acting cough suppressant Evidence: Codeine no more effective than DM
- 9. Sinusitis Bacteria isolated in 70% of patients with sinusitis Strict criteria: persistent, not improving for at
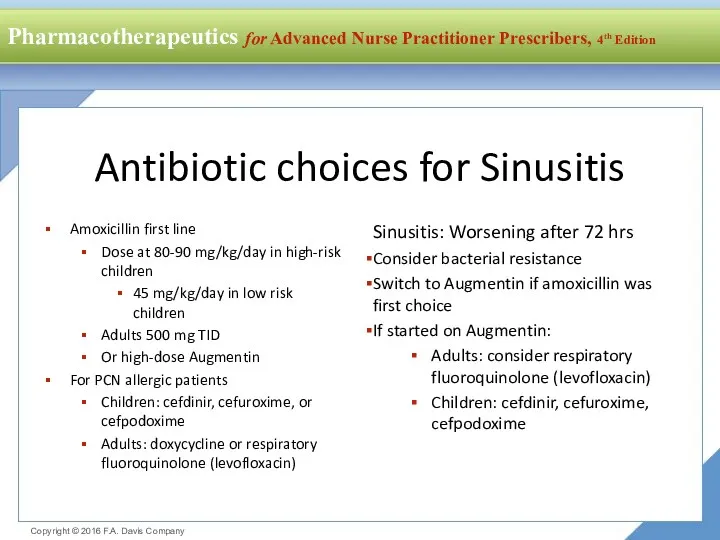
- 10. Antibiotic choices for Sinusitis Amoxicillin first line Dose at 80-90 mg/kg/day in high-risk children 45 mg/kg/day
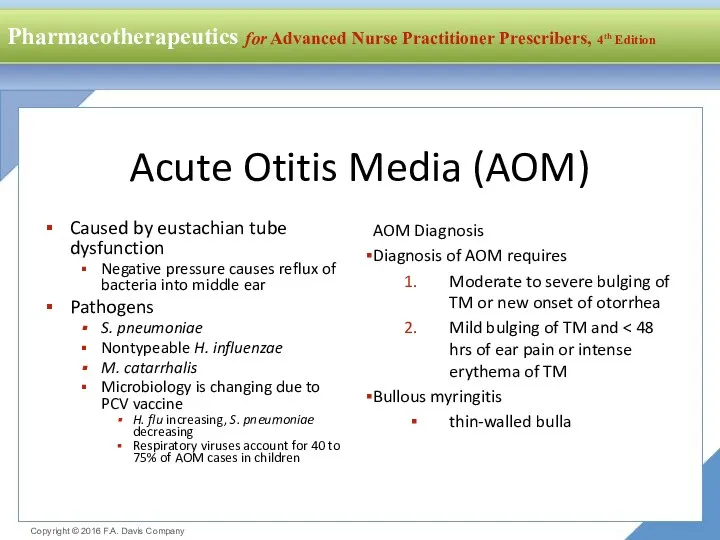
- 11. Acute Otitis Media (AOM) Caused by eustachian tube dysfunction Negative pressure causes reflux of bacteria into
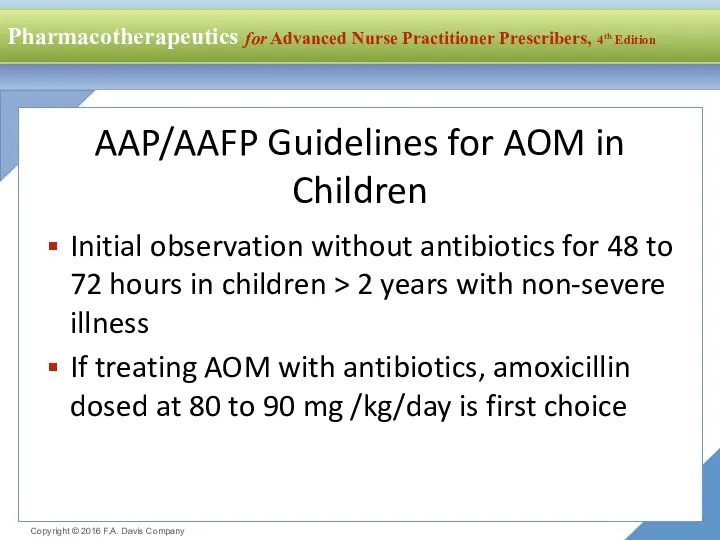
- 12. AAP/AAFP Guidelines for AOM in Children Initial observation without antibiotics for 48 to 72 hours in
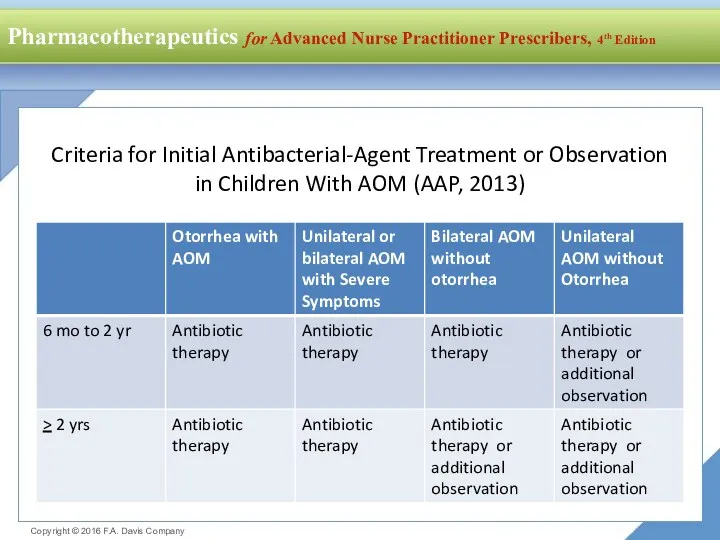
- 13. Criteria for Initial Antibacterial-Agent Treatment or Observation in Children With AOM (AAP, 2013)
- 14. AOM Antibiotic Choices Amoxicillin is first choice Or amoxicillin/clavulanate 90mg/kg/day of amoxicillin AOM antibiotics for PCN
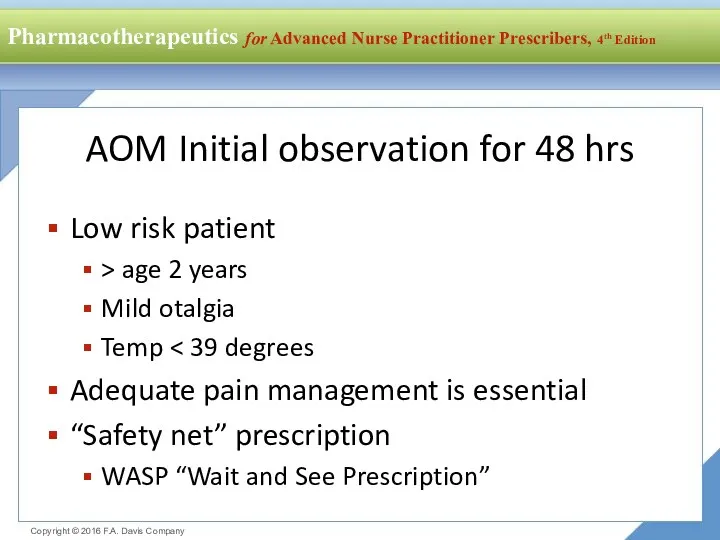
- 15. AOM Initial observation for 48 hrs Low risk patient > age 2 years Mild otalgia Temp
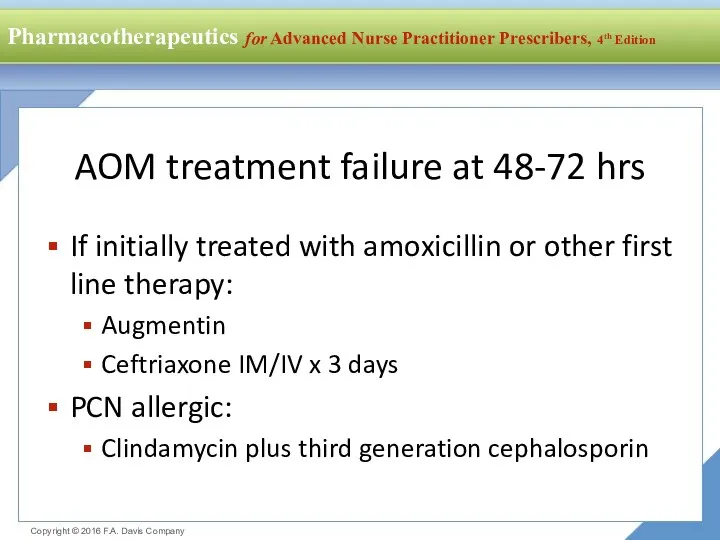
- 16. AOM treatment failure at 48-72 hrs If initially treated with amoxicillin or other first line therapy:
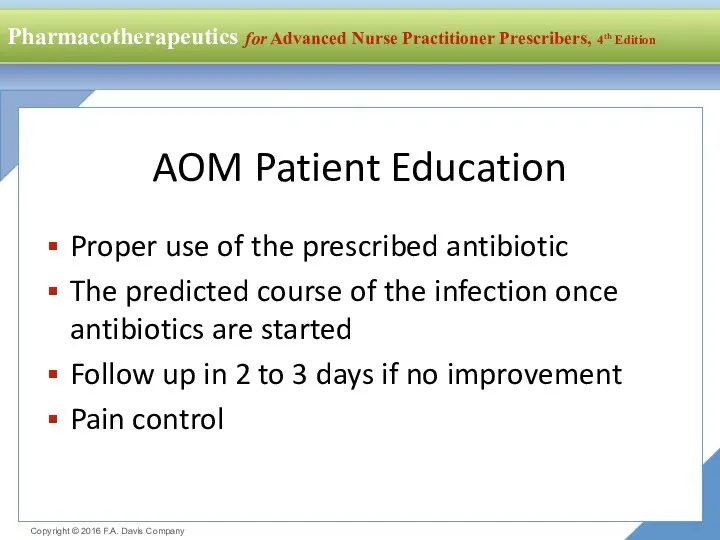
- 17. AOM Patient Education Proper use of the prescribed antibiotic The predicted course of the infection once
- 18. Asthma and COPD
- 19. Asthma Pathophysiology Chronic inflammatory disorder of the airways Recurrent episodes of wheezing, breathlessness and chest tightness
- 20. Asthma Goals of Therapy Reduce Impairment Prevent chronic symptoms Reduce use of inhaled short-acting beta agonists
- 21. Mild Intermittent Asthma Step 1 Therapy Use short-acting beta2 agonists as needed for symptoms Patients have
- 22. Beta2 Receptor Agonists Short-acting beta agonists Albuterol (ProAir, Ventolin, Proventil) metaproterenol (Alupent) terbutaline (Brethine, Brethaire) bitolterol
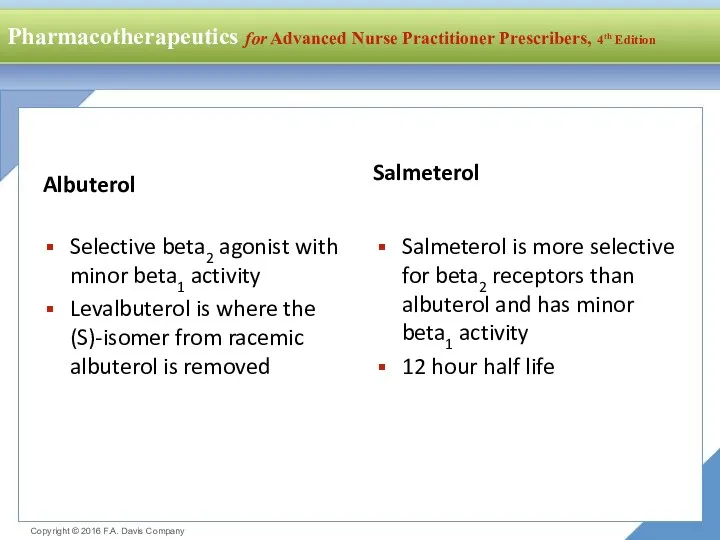
- 23. Albuterol Selective beta2 agonist with minor beta1 activity Levalbuterol is where the (S)-isomer from racemic albuterol
- 24. Beta Agonists Clinical Use Exercise induced bronchospasm Albuterol 2 puffs 15 min before exercise Salmeterol 2
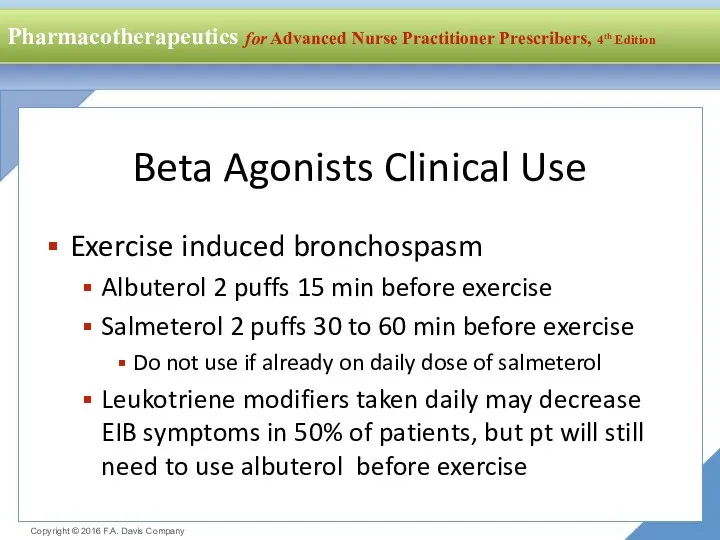
- 25. Beta2 Agonists Precautions and Contraindications Cardiac arrhythmias Diabetics: potential drug-induced hyperglycemia Long-acting beta agonists: Black Box
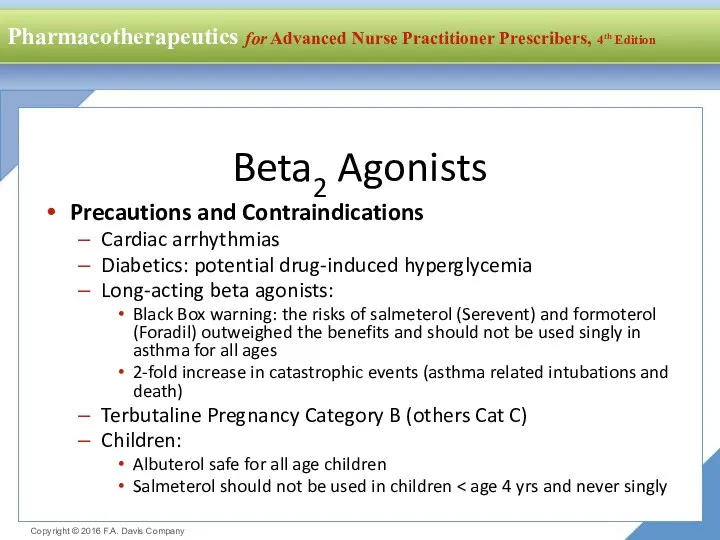
- 26. Beta Agonists: Drug Interactions Digitalis glycosides: increased risk of dysrhythmia Beta adrenergic blocking agents: direct competition
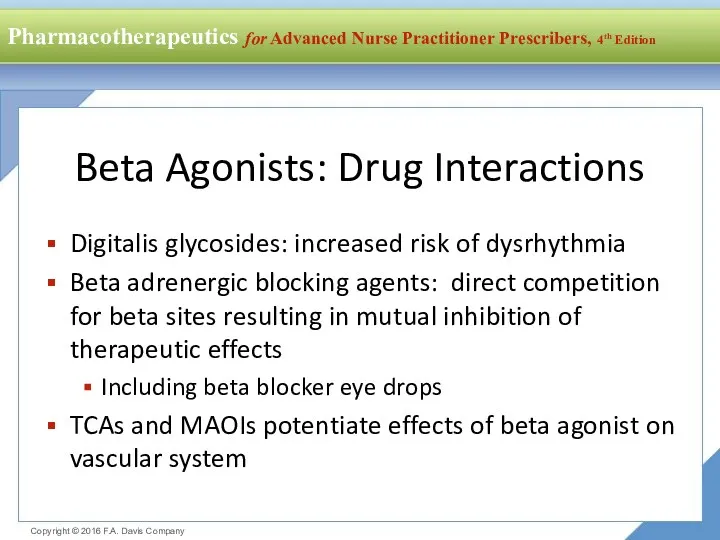
- 27. Monitoring Once control is achieved, the patient is seen every 1 to 6 months to determine
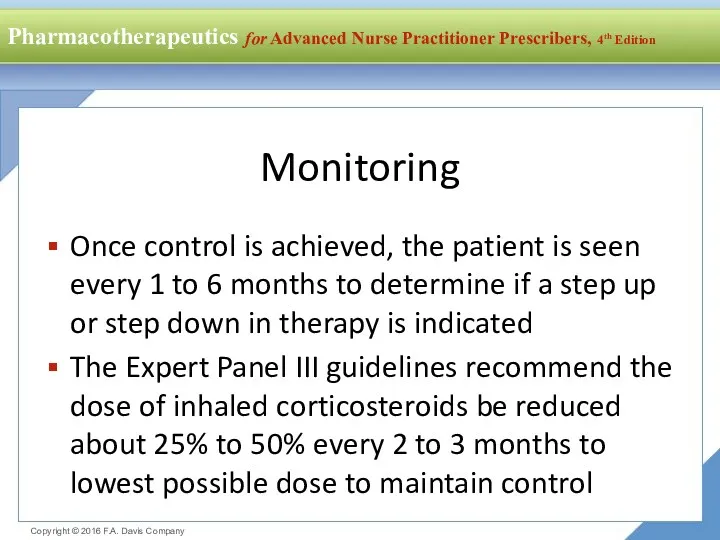
- 28. Managing Exacerbations Treat with oral steroids to regain control Use a short burst Adults: 40 to
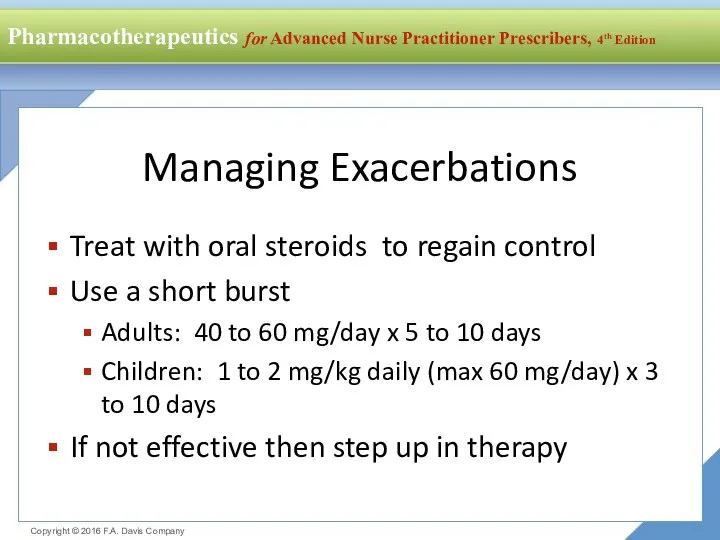
- 29. Mild Persistent Asthma Step 2 Therapy Treat with one long-term control medication daily Low dose inhaled
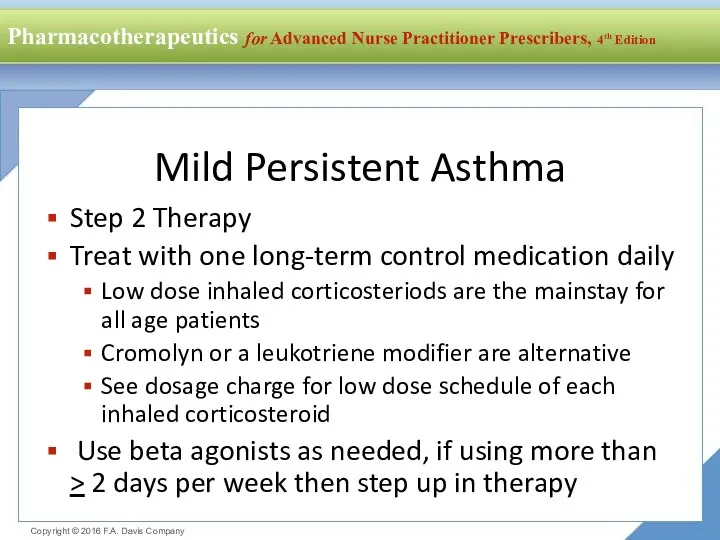
- 30. Moderate Persistent Asthma Step 3 Therapy Treat with medium-dose inhaled corticosteroids Or low-dose inhaled steroids plus
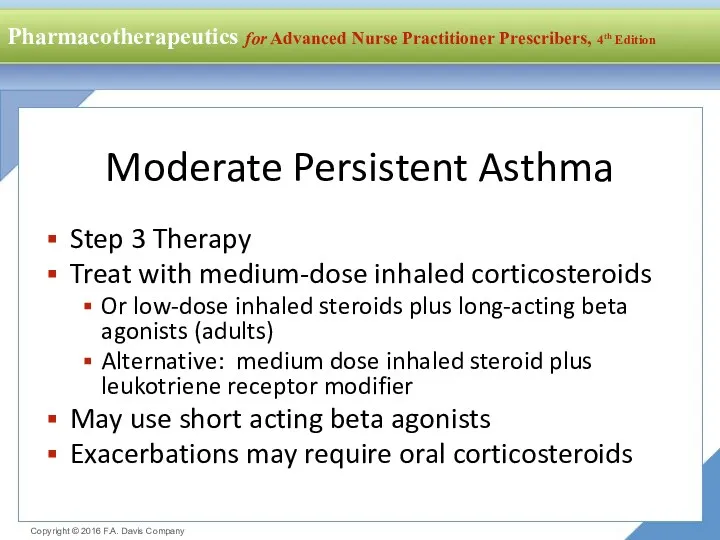
- 32. Скачать презентацию

 Особенности анестезиологии и интенсивной терапии в педиатрической практике
Особенности анестезиологии и интенсивной терапии в педиатрической практике Микобактерии. Возбудители туберкулеза
Микобактерии. Возбудители туберкулеза Болезнь Такаясу (неспецифический аортоартериит, синдром дуги аорты)
Болезнь Такаясу (неспецифический аортоартериит, синдром дуги аорты) Уход за телом умершего человека и транспортировка до места временного хранения
Уход за телом умершего человека и транспортировка до места временного хранения ОРВИ и грипп
ОРВИ и грипп Бактериальные инфекции
Бактериальные инфекции Поствакцинальные осложнения и реакции. Семинар 10
Поствакцинальные осложнения и реакции. Семинар 10 Ветеринарная вирусология. Вирус европейской чумы свиней
Ветеринарная вирусология. Вирус европейской чумы свиней Буйрек трансплантациясы
Буйрек трансплантациясы Диагностика отосклероза по данным МСКТ
Диагностика отосклероза по данным МСКТ Технология твердых лекарственных форм
Технология твердых лекарственных форм Инфекции мочевыводящих путей в практике участкового терапевта
Инфекции мочевыводящих путей в практике участкового терапевта Сестринский уход в офтальмологии. Лекция1
Сестринский уход в офтальмологии. Лекция1 Сестринский процесс при пиелонефрите
Сестринский процесс при пиелонефрите Синдром дисплазии соединительной ткани
Синдром дисплазии соединительной ткани О роли среднего медицинского звена в системе первичной медицинской помощи
О роли среднего медицинского звена в системе первичной медицинской помощи Диагностика и малоинвазивные методы лечения жидкостных образований брюшной полости
Диагностика и малоинвазивные методы лечения жидкостных образований брюшной полости В-лимфоциты – основные эффекторы гуморального иммунного ответа. Лекция 5
В-лимфоциты – основные эффекторы гуморального иммунного ответа. Лекция 5 Патогенные и условно-патогенные микроорганизмы. Пищевые интоксикации
Патогенные и условно-патогенные микроорганизмы. Пищевые интоксикации Патология красной крови
Патология красной крови Эпилепсия. Эпилептический статус
Эпилепсия. Эпилептический статус Псориаз. Классификация псориаза
Псориаз. Классификация псориаза Сыртқы тыныс патофизиологиясы
Сыртқы тыныс патофизиологиясы Особенности периферической крови и состояния эндотелия при инфаркте миокарда, ИБС и стенокардии
Особенности периферической крови и состояния эндотелия при инфаркте миокарда, ИБС и стенокардии Снотворные, противопаркинсонические, противоэпилептические средства
Снотворные, противопаркинсонические, противоэпилептические средства УЗИ почек
УЗИ почек Әйелдердің жүктілік мерзімі
Әйелдердің жүктілік мерзімі Новости COVID-2019
Новости COVID-2019