Updating the guidelines for procedural sedation Dr. Jannicke Mellin-Olsen, Norway European Society of Anaesthesiology Secretary презентация
Содержание
- 4. Conflicts of Interest: Financial: none Secretary ESA Past President European Board of Anaesthesiology Deputy Secretary WFSA
- 5. Presentation Overview: Anaesthesiology and patient safety Procedural sedation and Patient Safety Developing guidelines on Procedural Sedation
- 7. Anaesthesiology and patient safety October 16, 1846 Morton’s ether operation The start of effective anaesthesia January
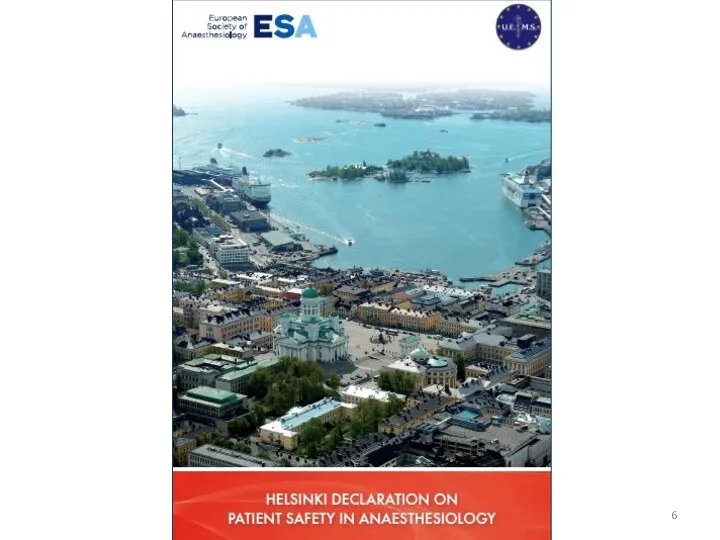
- 9. Launch Helsinki Declaration Helsinki, June 13, 2010 Seminar at the Euroanaesthesia Congress Presentations demonstrating our role
- 10. Helsinki Declaration on Patient Safety in Anaesthesiology “Patients have a right to expect to be safe
- 11. Queen Victoria’s 8th labour
- 12. Recent developments in medicine Enormous development of less traumatic surgical procedures ? Surgery may be associated
- 13. More potent medicines: Midazolam Short acting opioids with short onset time (alfentanil, remifentanil) IV hypnotics (propofol,
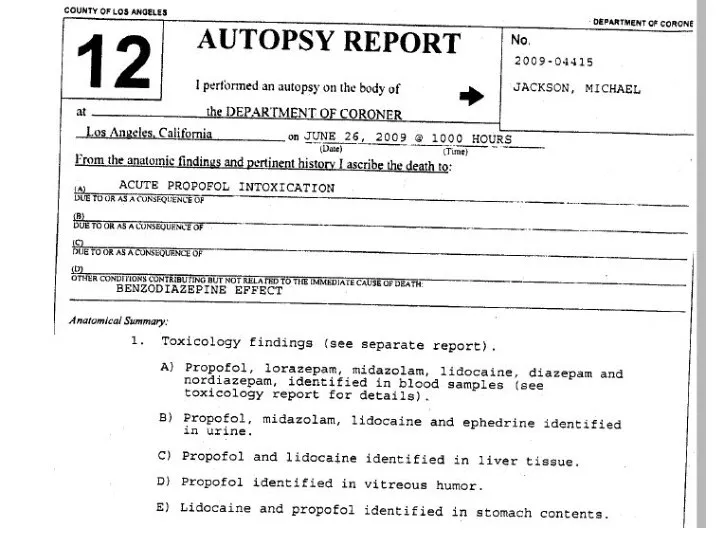
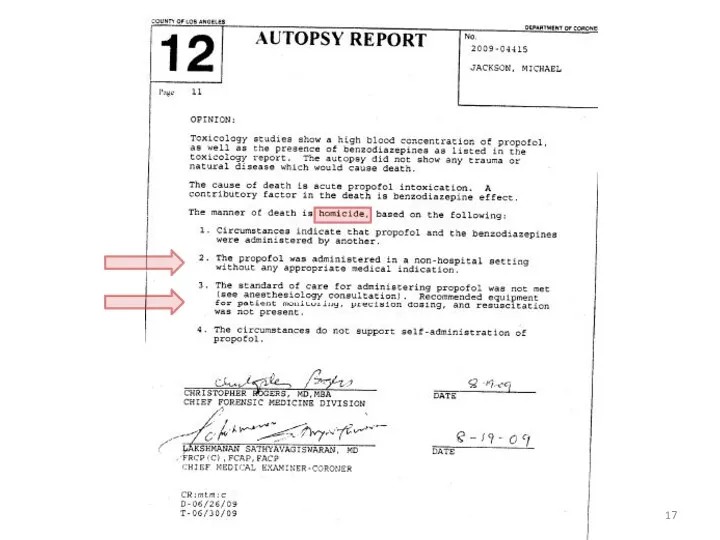
- 16. Why did Michael Jackson die? Wrong diagnosis. Wrong indication for Procedural Sedation Wrong PSA medicine administration
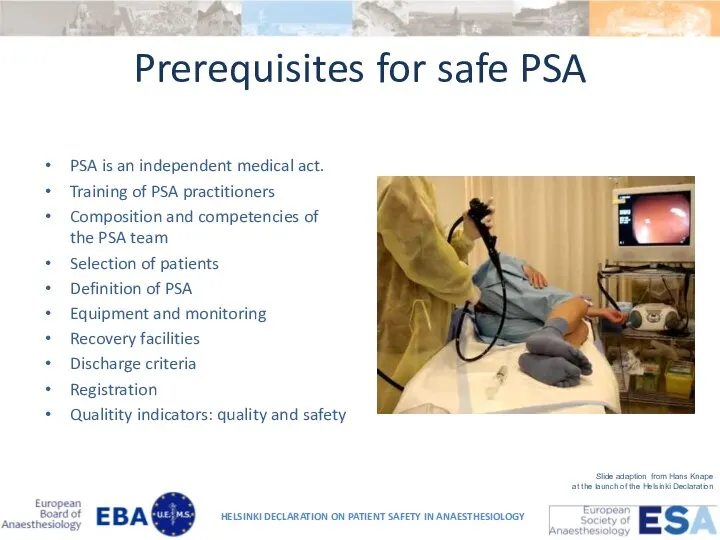
- 18. Prerequisites for safe PSA PSA is an independent medical act. Training of PSA practitioners Composition and
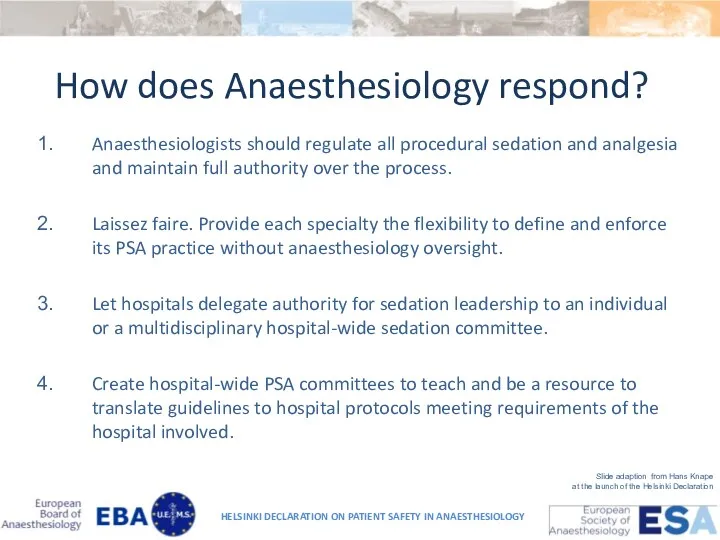
- 19. How does Anaesthesiology respond? Anaesthesiologists should regulate all procedural sedation and analgesia and maintain full authority
- 20. Guidelines on PSA by non-anaesthesiologists European Guidelines ESGE-ESGENA-ESA-Guideline: Non-anesthesiologist administration of propofol for GI endoscopy HELSINKI
- 22. In 2010, ESGE, ESGEN and ESA formulated guidelines for NAAP for GI endoscopy. However, the ESA
- 24. Controversy One group opposes the guideline through perceived lack of scientific validity and apparent abandonment of
- 25. Anaesthesiologists in every European nation have a unique opportunity to show leadership in shaping the practice
- 26. Questionnaire, 2012: National Associations of Nurse Anesthetists in Europe National Delegates of the European Section and
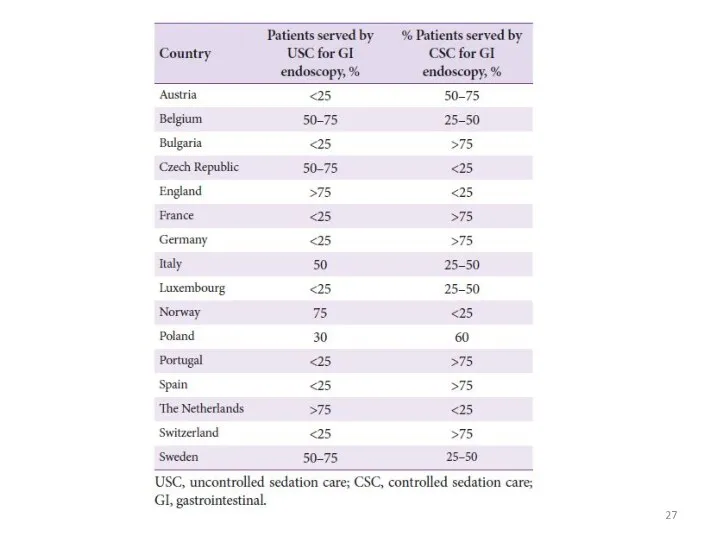
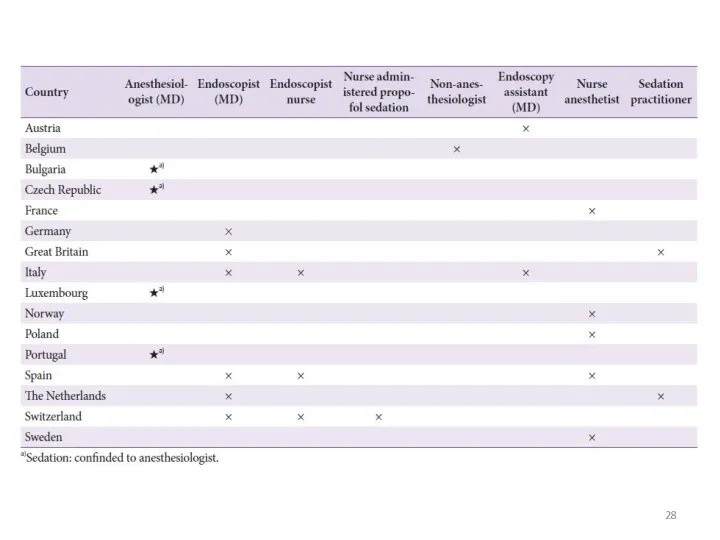
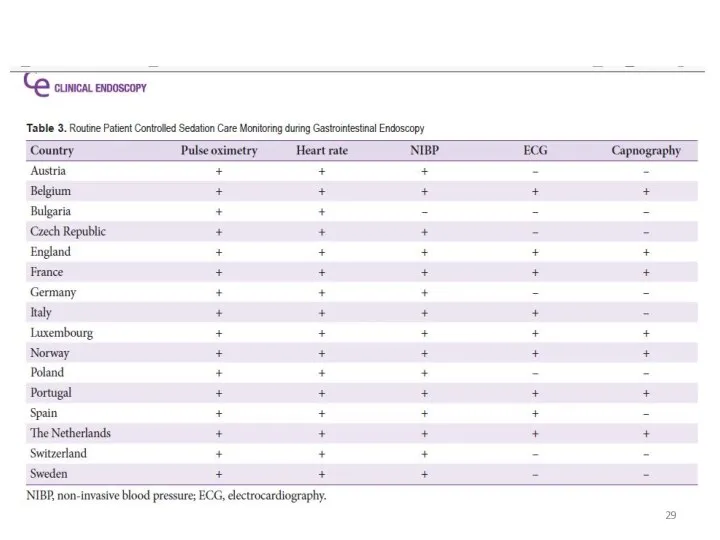
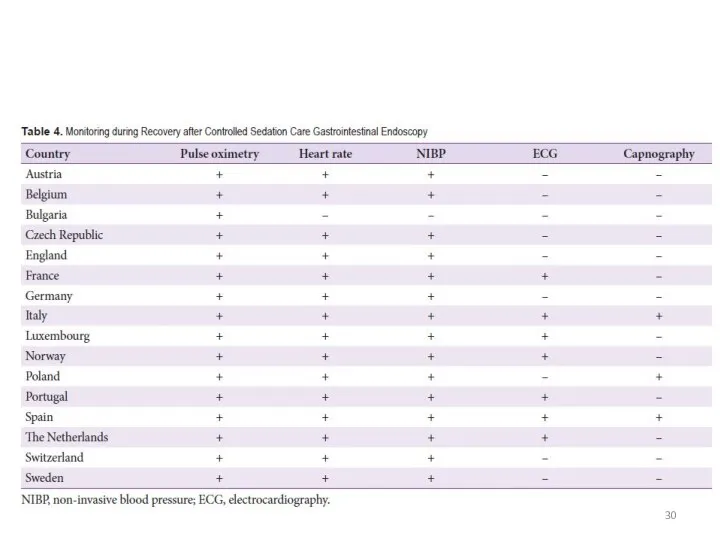
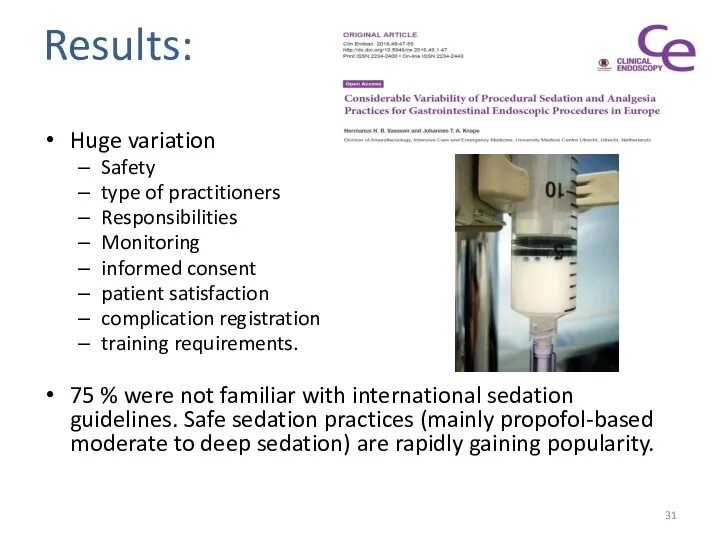
- 31. Results: Huge variation Safety type of practitioners Responsibilities Monitoring informed consent patient satisfaction complication registration training
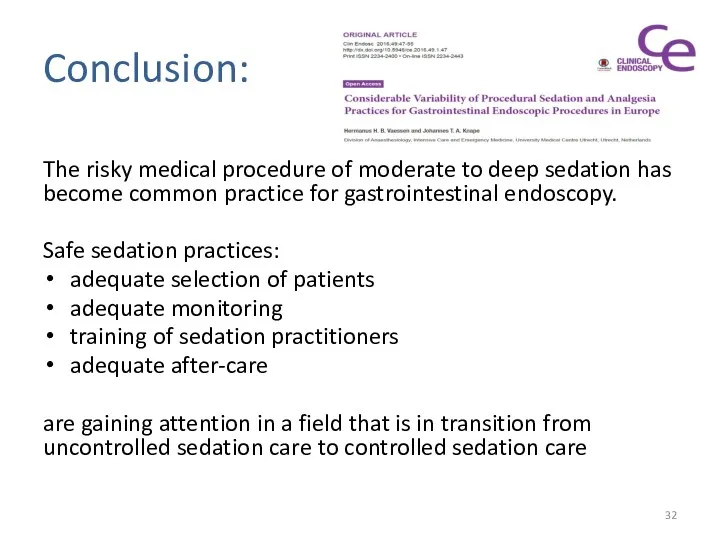
- 32. Conclusion: The risky medical procedure of moderate to deep sedation has become common practice for gastrointestinal
- 33. Conclusion: International guidelines in existence. Lack of formal implementation processes has limited the development of uniform
- 34. Conclusion: For a risky medical procedure such as moderate-to-deep sedation further improvement of quality by harmonization
- 35. Evidence based Guidelines on adult Procedural Sedation
- 36. Task force – six subcommittees Competences Medicines and adverse effects Monitoring Patient selection Quality and follow-up
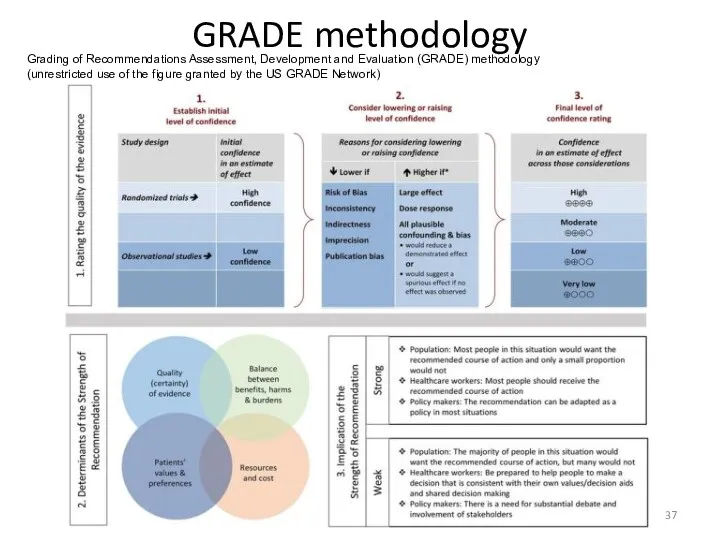
- 37. GRADE methodology Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology (unrestricted use of the figure
- 38. Literature search MEDLINE, EMBASE, Cochrane : Conscious sedation Deep sedation Procedure Intervention Exam 12,263 records Second
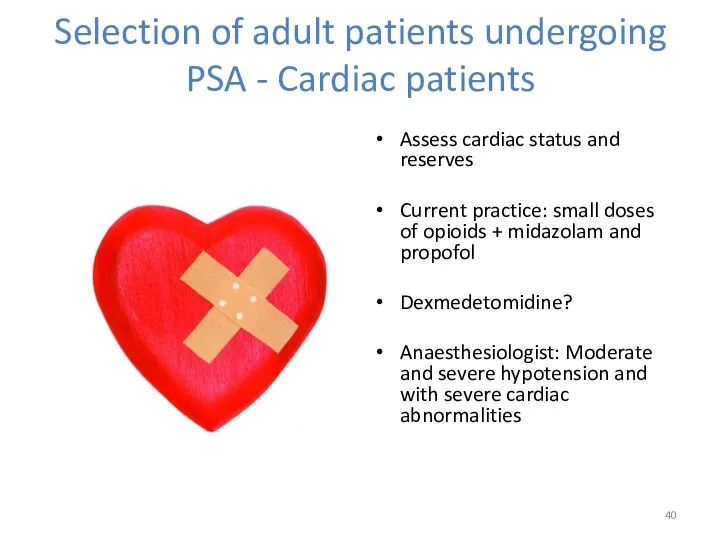
- 40. Selection of adult patients undergoing PSA - Cardiac patients Assess cardiac status and reserves Current practice:
- 41. Obstructive Sleep Apnoea OSAS not per se predictive of anaesthesia related cardiopulm complications during deep sedation.
- 42. Chronic Renal Failure Increased risk of developing respiratory problems during sedation Midazolam and fentanyl –metabolised in
- 43. Chronic Liver Disease Propofol
- 44. Morbidly Obese High risk of respiratory complications Beach chair positioning ET-tubes preferred airway management Reminfentanil and
- 45. ASA III and IV and old patients Increased risk of hypoxaemia, hypotension, arrythmias. Reduce dose, go
- 46. Airway Assessment Always part of the procedure. PSA relatively contraindicated in patients who are likely to
- 47. Fasting ASA guidelines: Patients undergoing PSA for "elective procedures" fast according to the standards used for
- 48. Monitoring NIBP ECG Pulse oximetry Capnography BIS? Spectral entropy? Auditory evoked potentials?
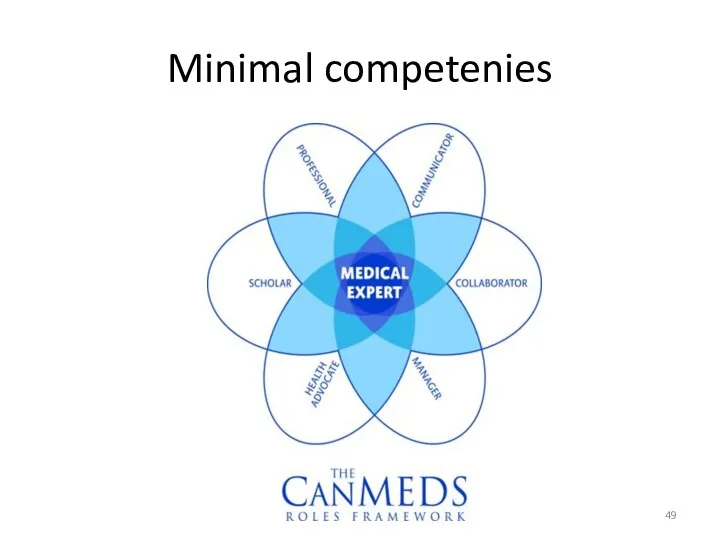
- 49. Minimal competenies
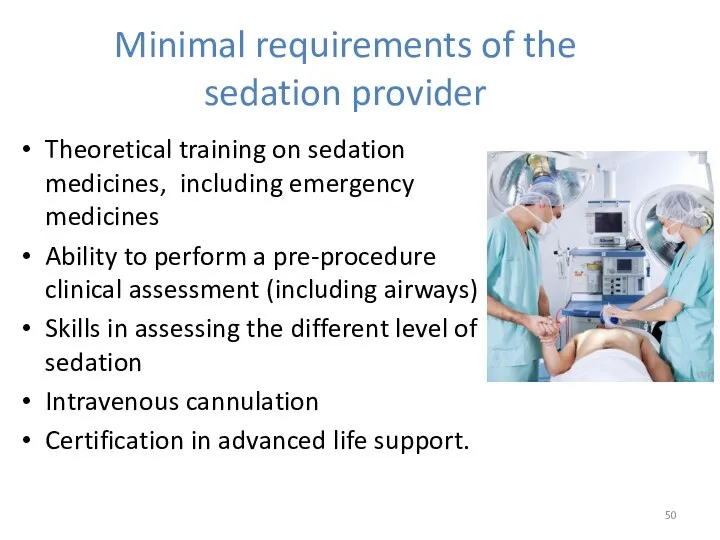
- 50. Minimal requirements of the sedation provider Theoretical training on sedation medicines, including emergency medicines Ability to
- 51. http://www.uptodate.com/contents/procedural-sedation-in-adults Procedural sedation in adults Robert L Frank, Allan B Wolfson, Jonathan Grayzel Literature review current
- 52. Sedation medicines – often used Pethidine Morphine and other opioids Benzodiazepines Propofol Ketamine Ketofol Etomidate Etc…
- 53. Post sedation care - discharge: Safe for discharge: The procedure should be of sufficiently low risk
- 54. Discharge Safely discharged within 30 minutes of receiving their last dose of sedative provided that no
- 58. Скачать презентацию




 Патологиялық анатомия
Патологиялық анатомия Оба қоздырғышы
Оба қоздырғышы Microscopic colitis
Microscopic colitis Сосудистые анастомозы РУС
Сосудистые анастомозы РУС Нарушение половых функций. Климакс
Нарушение половых функций. Климакс Мeningeal a syndrome in clinic of infectious diseases
Мeningeal a syndrome in clinic of infectious diseases Медсестринський процес – історичний нарис. Професійні організації медичних сестер
Медсестринський процес – історичний нарис. Професійні організації медичних сестер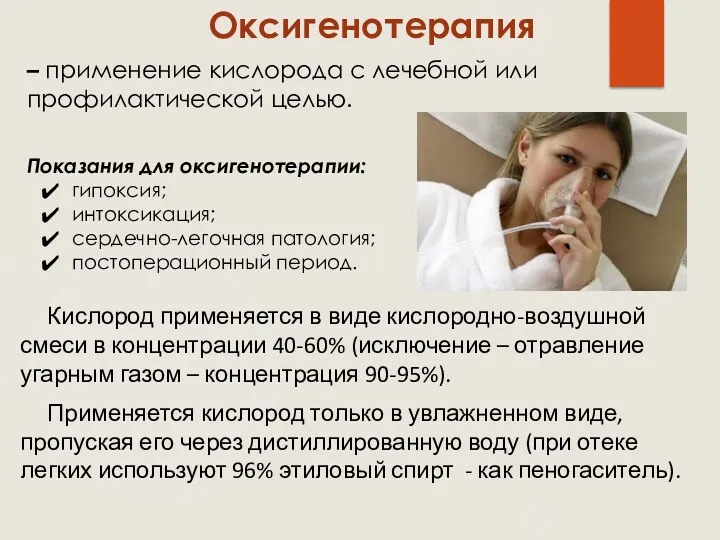 Оксигенотерапия. Виды оксигенотерапии
Оксигенотерапия. Виды оксигенотерапии Потребность в нормальном дыхании
Потребность в нормальном дыхании Cardiovascular system
Cardiovascular system Первая помощь детям при травмах и несчастных случаях. Общие советы для детей и взрослых
Первая помощь детям при травмах и несчастных случаях. Общие советы для детей и взрослых Медикаментозды остеопороз: алдын алудағы және түзетуге негізгі ұстанымдар
Медикаментозды остеопороз: алдын алудағы және түзетуге негізгі ұстанымдар Первая помощь при отморожении, общем охлаждении организма
Первая помощь при отморожении, общем охлаждении организма Обследование зубных рядов, зубов и периодонта в детском возрасте
Обследование зубных рядов, зубов и периодонта в детском возрасте Терапиялық стоматология клиникасындағы ауру сезімі және жансыздандыру
Терапиялық стоматология клиникасындағы ауру сезімі және жансыздандыру Общие вопросы лучевой диагностики. Ультразвуковое исследование
Общие вопросы лучевой диагностики. Ультразвуковое исследование Концепция обеспечения качества лекарственных средств
Концепция обеспечения качества лекарственных средств Клиническая симптоматология рака и абсцесса легких. Синдром полости в легком. (Тема 21)
Клиническая симптоматология рака и абсцесса легких. Синдром полости в легком. (Тема 21) Острая почечная и острая печеночная недостаточность
Острая почечная и острая печеночная недостаточность Ранний детский аутизм
Ранний детский аутизм Технические регламенты и национальные стандарты оказания оздоровительных услуг гостиничными организациями. (Лекция 6.1)
Технические регламенты и национальные стандарты оказания оздоровительных услуг гостиничными организациями. (Лекция 6.1) Уход за больными хирургического профиля
Уход за больными хирургического профиля Требования к организации и проведению профилактической дератизации и дезинсекции
Требования к организации и проведению профилактической дератизации и дезинсекции Периферические венозные катетеры
Периферические венозные катетеры Ортаңғы және ішкі құлақ аурулары. Саңыраулық және мылқаулық орта кұлактың жедел және созылмалы кабынуы мастоидит
Ортаңғы және ішкі құлақ аурулары. Саңыраулық және мылқаулық орта кұлактың жедел және созылмалы кабынуы мастоидит Нейропротезирование. История нейропротезирования
Нейропротезирование. История нейропротезирования Синдромы при заболеваниях дыхательной системы
Синдромы при заболеваниях дыхательной системы Первая медицинская помощь
Первая медицинская помощь