Содержание
- 2. Benzodiazepines adverse effects
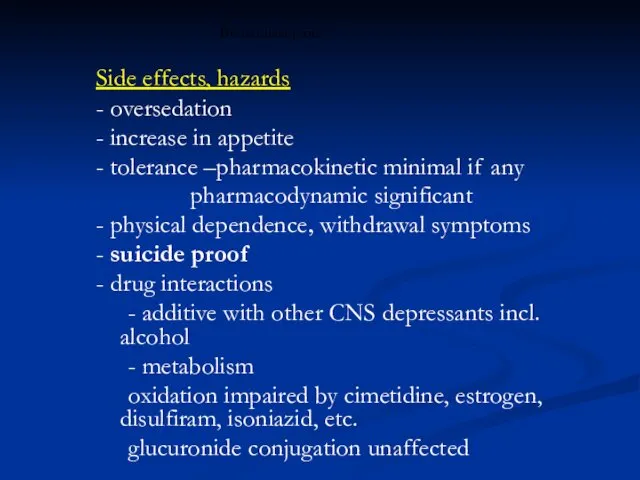
- 3. Benzodiazepines Side effects, hazards - oversedation - increase in appetite - tolerance –pharmacokinetic minimal if any
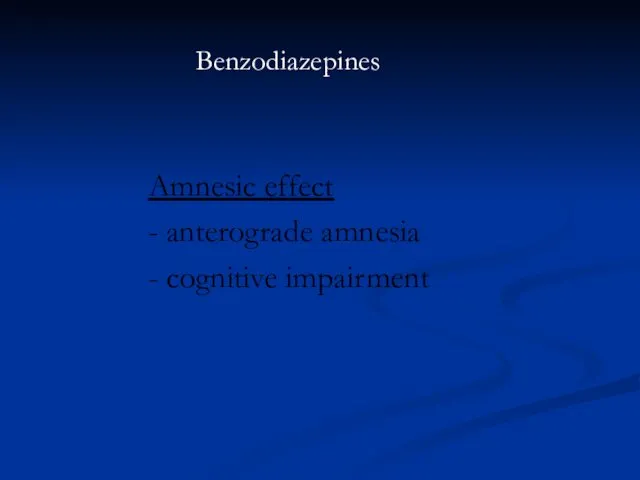
- 4. Benzodiazepines Amnesic effect - anterograde amnesia - cognitive impairment
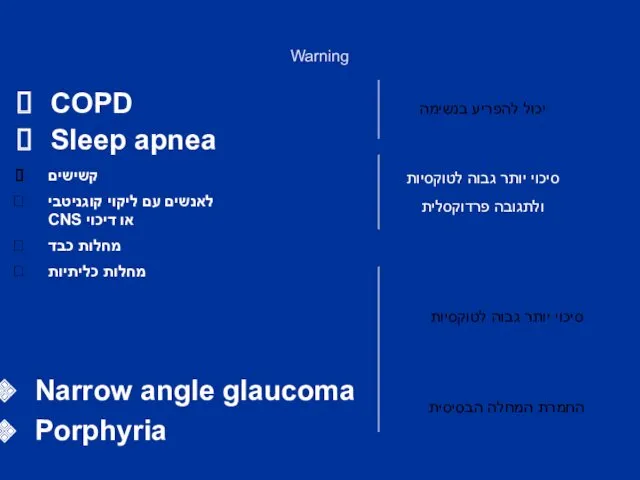
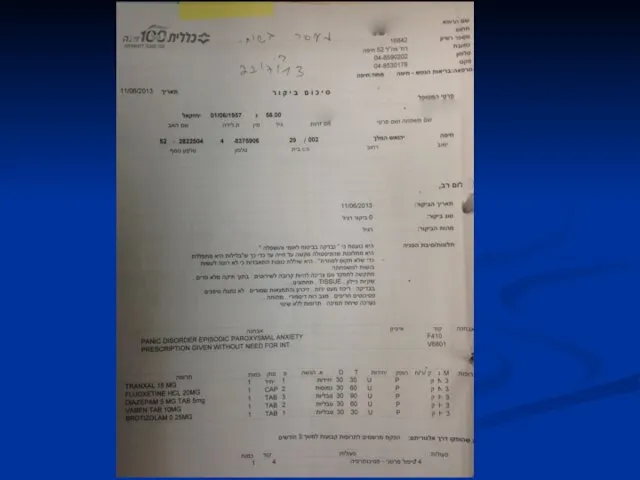
- 5. Warning קשישים לאנשים עם ליקוי קוגניטבי CNS או דיכוי מחלות כבד מחלות כליתיות יכול להפריע בנשימה
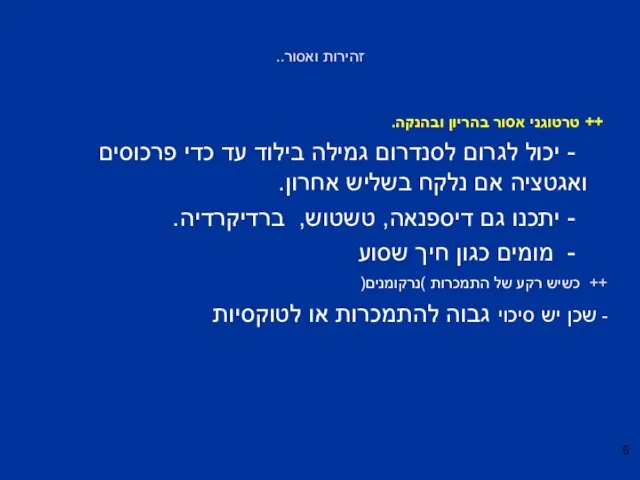
- 6. זהירות ואסור.. ++ טרטוגני אסור בהריון ובהנקה. - יכול לגרום לסנדרום גמילה בילוד עד כדי פרכוסים
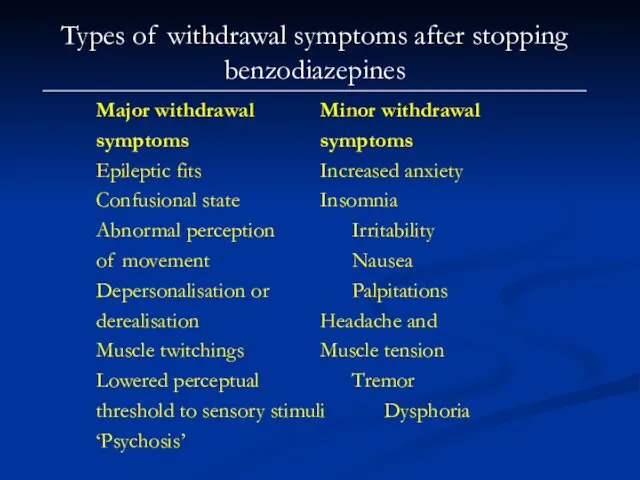
- 7. Types of withdrawal symptoms after stopping benzodiazepines Major withdrawal Minor withdrawal symptoms symptoms Epileptic fits Increased
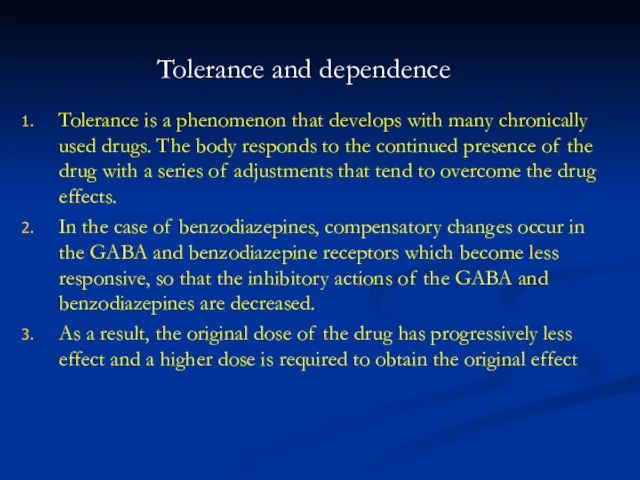
- 8. Tolerance and dependence Tolerance is a phenomenon that develops with many chronically used drugs. The body
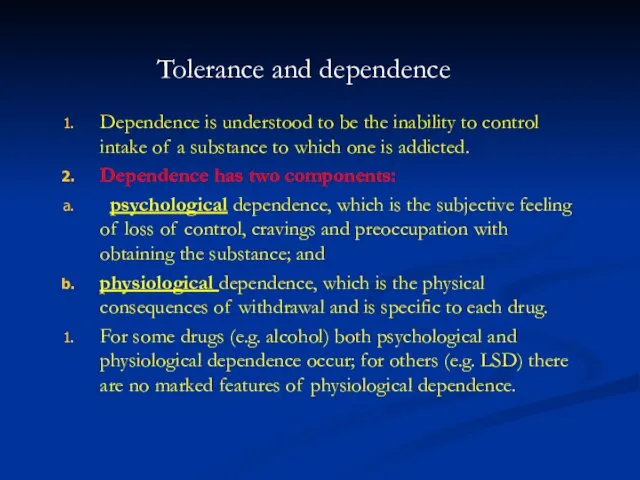
- 9. Tolerance and dependence Dependence is understood to be the inability to control intake of a substance
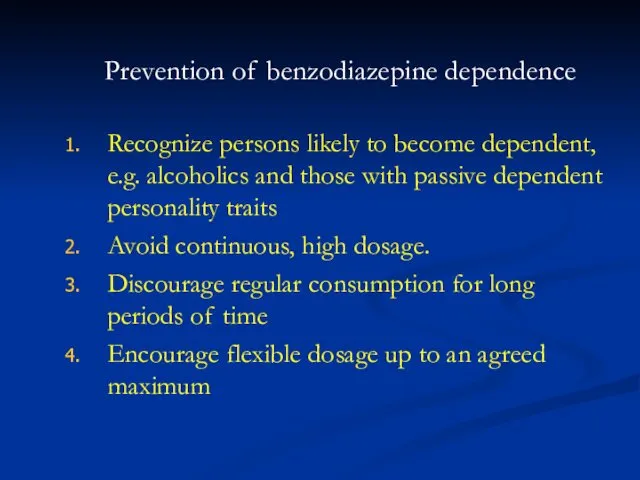
- 10. Prevention of benzodiazepine dependence Recognize persons likely to become dependent, e.g. alcoholics and those with passive
- 11. Withdrawal syndrome and discontinuation syndrome Any drug consumed regularly and heavily can be associated with withdrawal
- 12. Benzodiazepine Withdrawal Symptoms Psychological symptoms – excitability, sleep disturbances, increased anxiety, panic attacks, agoraphobia, social phobia,
- 13. Benzodiazepine Withdrawal Symptoms Physical symptoms – Headache, pain, stiffness, tingling, numbness, altered sensation, weakness, fatigue, influenza-like
- 14. Mechanisms of withdrawal reactions Drug withdrawal reactions in general tend to consist of a mirror image
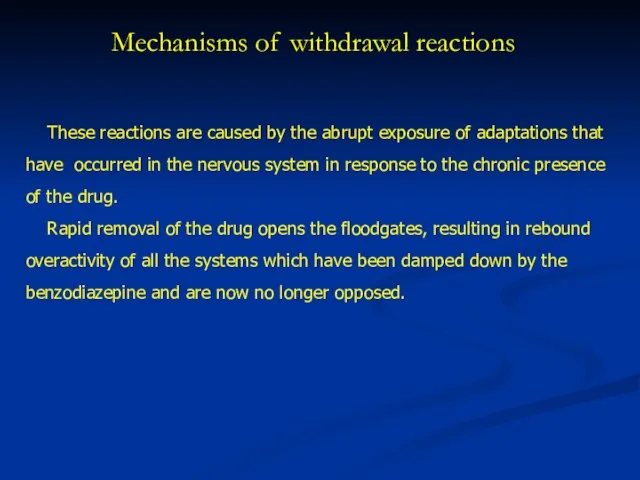
- 15. Mechanisms of withdrawal reactions These reactions are caused by the abrupt exposure of adaptations that have
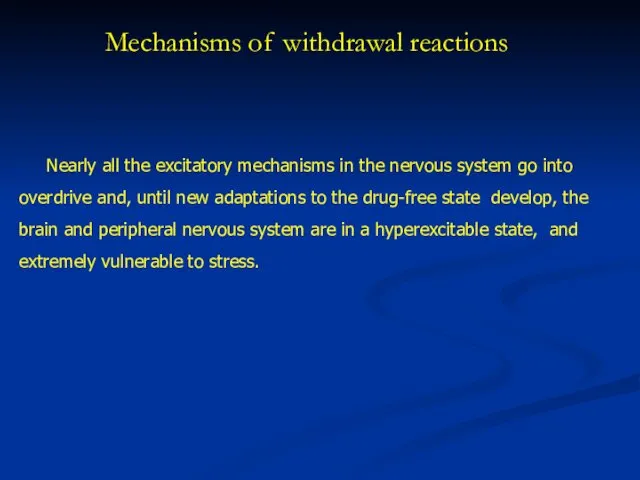
- 16. Mechanisms of withdrawal reactions Nearly all the excitatory mechanisms in the nervous system go into overdrive
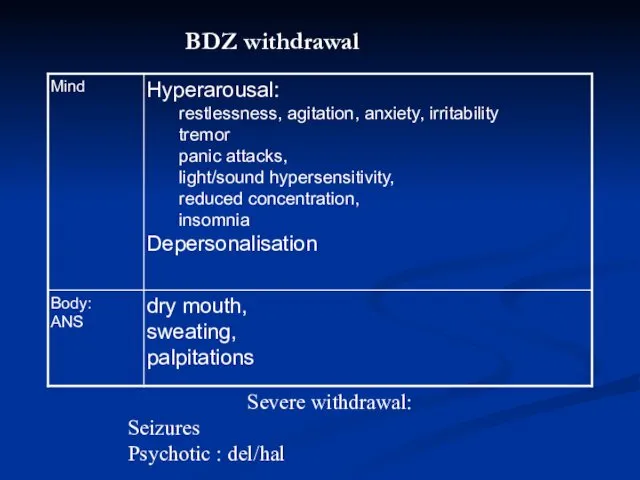
- 17. BDZ withdrawal Severe withdrawal: Seizures Psychotic : del/hal
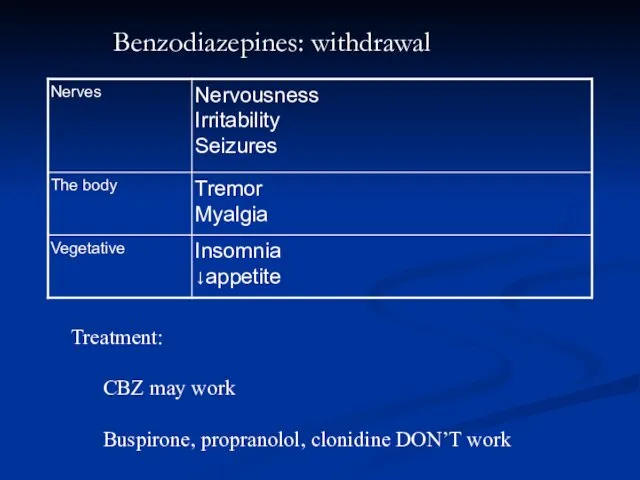
- 18. Benzodiazepines: withdrawal Treatment: CBZ may work Buspirone, propranolol, clonidine DON’T work
- 19. Management of benzodiazepine withdrawal 1. Withdrawal of the benzodiazepine drug can be managed in primary care
- 20. Management of benzodiazepine withdrawal Switching to diazepam 1. Diazepam is preferred because it possesses a long
- 21. Management of benzodiazepine withdrawal Gradual Dosage Reduction 1. It is generally recommended that the dosage should
- 22. The rate of withdrawal 1. The rate of withdrawal be tailored to the patient's individual needs
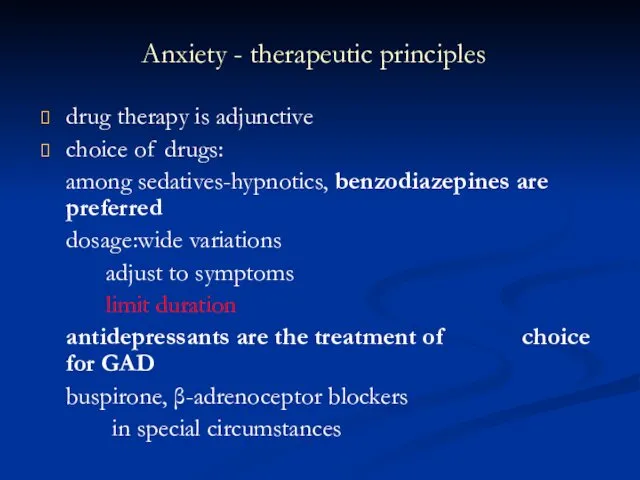
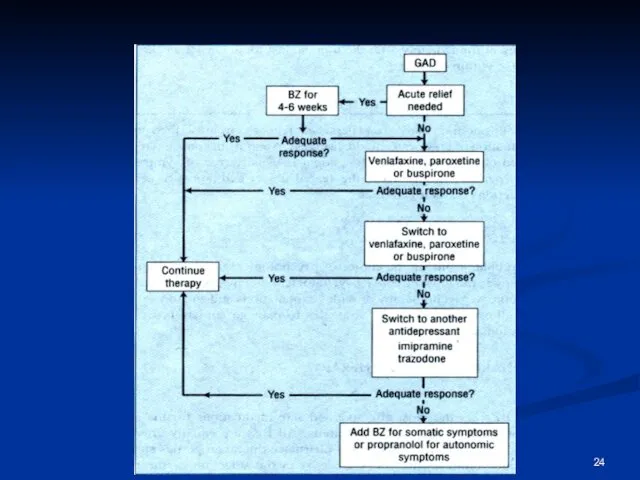
- 23. Anxiety - therapeutic principles drug therapy is adjunctive choice of drugs: among sedatives-hypnotics, benzodiazepines are preferred
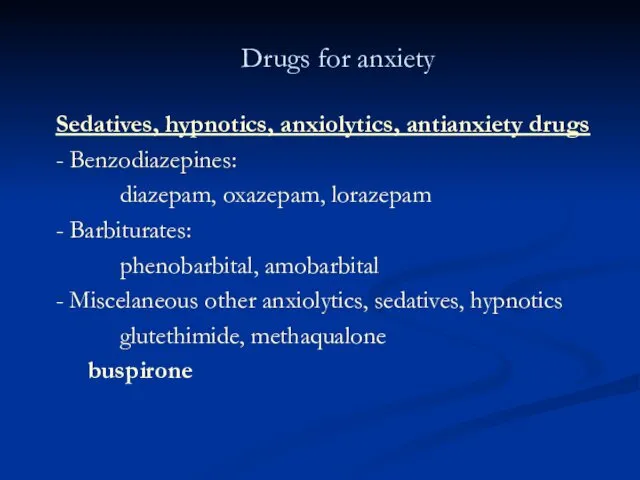
- 25. Drugs for anxiety Sedatives, hypnotics, anxiolytics, antianxiety drugs - Benzodiazepines: diazepam, oxazepam, lorazepam - Barbiturates: phenobarbital,
- 26. Drugs for anxiety Antidepressants venlafaxine, paroxetine Miscellaneous - β-adrenoceptor blockers: propranolol - Sedative antihistaminics: diphenhydramine -
- 29. Скачать презентацию

 Металеві конструкції. Частина 3
Металеві конструкції. Частина 3 Влияние стилей педагогического общения на психологический комфорт в группе
Влияние стилей педагогического общения на психологический комфорт в группе Социальный проект Христианский подвиг Святой блаженной Ксении Петербургской
Социальный проект Христианский подвиг Святой блаженной Ксении Петербургской Легенды старого Кенигсберга
Легенды старого Кенигсберга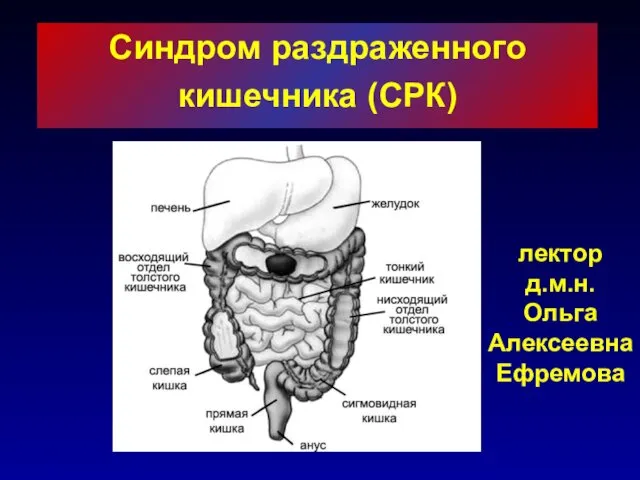 Синдром раздраженного кишечника (СРК)
Синдром раздраженного кишечника (СРК) Жестокое обращение с детьми
Жестокое обращение с детьми Навыки персональной безопасности
Навыки персональной безопасности Біріншілік туберкулез
Біріншілік туберкулез Инструкция по обновлению программного обеспечения планшета МегаФон V9+
Инструкция по обновлению программного обеспечения планшета МегаФон V9+ Создание заменителя древесного угля для производства кристаллического кремния и высококачественного чугуна (Н3)
Создание заменителя древесного угля для производства кристаллического кремния и высококачественного чугуна (Н3) Условия организации воспитания и обучения с нарушениями слуха
Условия организации воспитания и обучения с нарушениями слуха Неделя Игры и игрушки с 17ноября по 21 ноября 2014года. Средняя группа № 8 Гномики
Неделя Игры и игрушки с 17ноября по 21 ноября 2014года. Средняя группа № 8 Гномики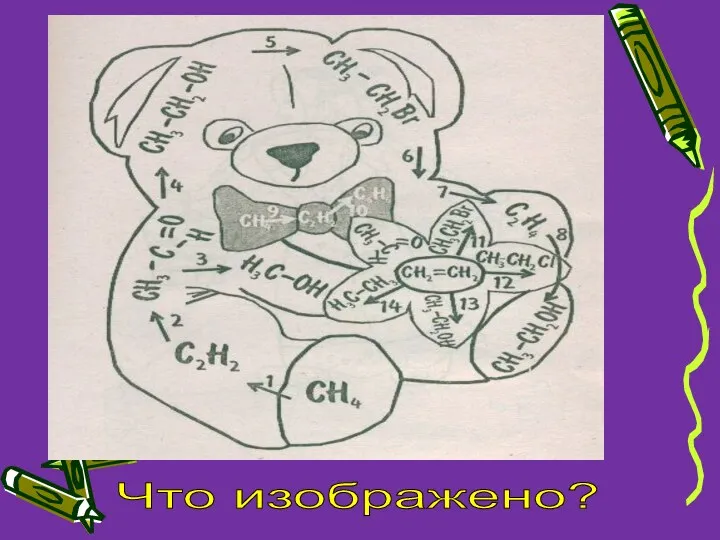 Классификация органических соединений в химии
Классификация органических соединений в химии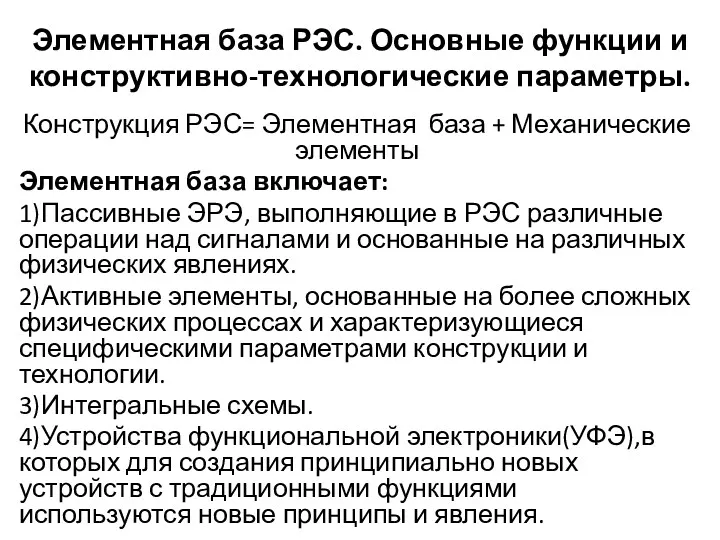 Интегральные утройства. Элементная база РЭС. Основные функции и конструктивно-технологические параметры
Интегральные утройства. Элементная база РЭС. Основные функции и конструктивно-технологические параметры Научная конференция в АСОУ г.Москва
Научная конференция в АСОУ г.Москва Операционные системы
Операционные системы Социальные сети
Социальные сети Графовые модели систем защиты информации. Лекция
Графовые модели систем защиты информации. Лекция Принципы менеджмента в Японии
Принципы менеджмента в Японии Автокөлік жүргізушілерінің еңбек гигиенасы
Автокөлік жүргізушілерінің еңбек гигиенасы Тематическое занятие, посвящённое П.И. Чайковскому(для детей подготовительной группы)
Тематическое занятие, посвящённое П.И. Чайковскому(для детей подготовительной группы) Объединение юных журналистов Проба пера
Объединение юных журналистов Проба пера Государственная система промышленных приборов и средств автоматизации (ГСП)
Государственная система промышленных приборов и средств автоматизации (ГСП) Диабетическая нефропатия
Диабетическая нефропатия Уточнение методики автоматизированного расчета НДС сварной конструкции рештака шахтного конвейера
Уточнение методики автоматизированного расчета НДС сварной конструкции рештака шахтного конвейера Nike. How the brand survived until today
Nike. How the brand survived until today ВЫСТУПЛЕНИЕ 05.11.2014 Биологические причины неуспеваемости учащихся общеобразовательной школы
ВЫСТУПЛЕНИЕ 05.11.2014 Биологические причины неуспеваемости учащихся общеобразовательной школы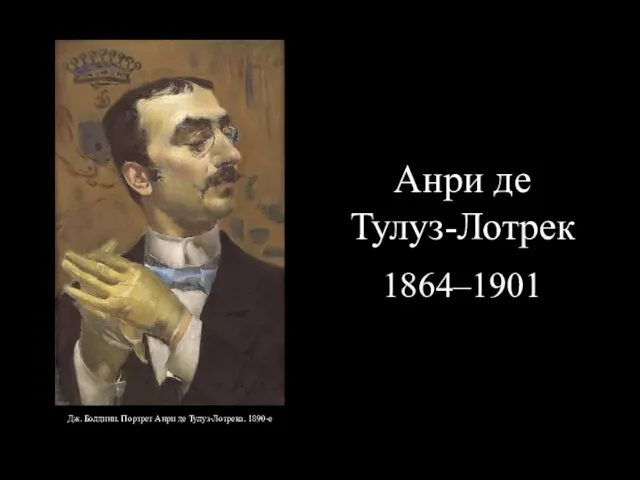 Анри де Тулуз-Лотрек 1864–1901
Анри де Тулуз-Лотрек 1864–1901