Содержание
- 3. Pain is a universally understood sign of disease; it is also the most common symptom that
- 4. The somatosensory system involves the conscious perception of touch, pressure, pain, temperature, position, movement, and vibration
- 5. Second-order neuron cell bodies are located in the dorsal horn and medullary nuclei. Third-order neurons are
- 6. Image courtesy of Legon et al.[6]
- 7. Pain Etiology The categories of pain nociceptive neuropathic psychogenic Different types of pain tend to respond
- 8. Nociceptive pain Nociception is a normal physiologic response to stimuli initiated by nociceptors, which detect mechanical,
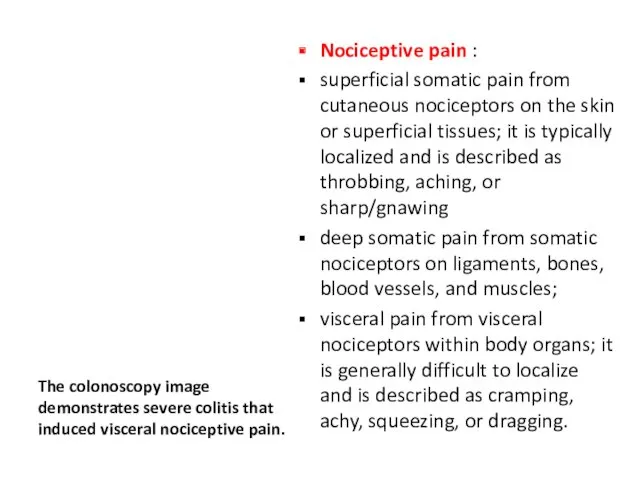
- 9. The colonoscopy image demonstrates severe colitis that induced visceral nociceptive pain. Nociceptive pain : superficial somatic
- 10. Neuropathic pain Neuropathic pain is pain induced by damage to the nerves themselves or by aberrant
- 11. Herpes zoster (shown) can cause neuropathic pain via growth and inflammation within dermatomal nerves.
- 12. Pain Etiology Sympathetically mediated pain is accompanied by evidence of edema, changes in skin blood flow,
- 13. Pain Etiology Radicular pain is evoked by stimulation of nociceptive afferent fibers in spinal nerves, their
- 14. Pain Etiology Psychogenic pain is inconsistent with the likely anatomic distribution of the presumed generator, or
- 15. Sensitization Sensitization is an adaptive process in which innocuous stimuli produce an excessive response. Repeated intense
- 16. For example, patients with sunburns often experience intense pain and discomfort with even very light touch
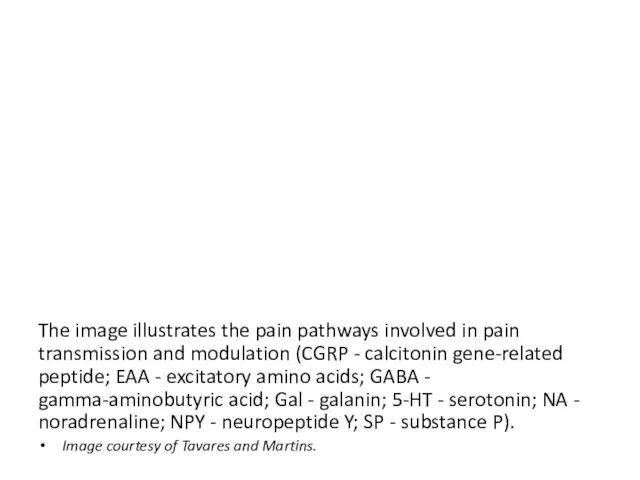
- 17. The image illustrates the pain pathways involved in pain transmission and modulation (CGRP - calcitonin gene-related
- 18. Pain modulation Pain modulation can both enhance and dampen pain signals. Placebo can have a significant
- 19. Pain assessment Pain assessment should be ongoing, individualized, and documented. Patients should be asked to describe
- 20. Pain must be assessed using a multidimensional approach, with determination of the following: Chronicity Severity Quality
- 21. Pain assessment. Chronicity of Pain Initial assessment of pain should always include the onset of pain
- 22. Pain assessment. Chronicity of Pain Chronic pain does not resolve within 3–6 months of its initiation
- 23. Pain assessment. Severity of Pain Pain is subjective expression. Objective quantification of pain has been one
- 24. Pain assessment. Quality of Pain The quality of pain is described by the patient in purely
- 25. Pain assessment. Contributing/Associated Factors Nociceptive symptoms often can be amplified by certain body positions and/or activities.
- 26. Pain assessment. Anatomical Etiology of Pain It is possible to describe different types of pain, and
- 27. Pain assessment. Mechanism of Injury If applicable, the mechanism of injury can direct the clinicians in
- 28. Pain assessment. Barriers to Pain Assessment Barriers to pain assessment occur because of the assessment’s heavy
- 29. Pain assessment. Barriers to Pain Assessment The pain perception threshold is the point at which the
- 30. Pain assessment Determining the best treatment course for pain management begins with identification of the intensity
- 31. Single-dimensional scales: These scales assess a single dimension of pain and, through patient self-reporting, measure only
- 32. Multidimensional scales Multidimensional scales (eg, McGill Pain Questionnaire, Brief Pain Inventory) measure the pain intensity, the
- 33. Although laboratory tests, imaging studies, and nerve or muscle conduction studies do not show pain in
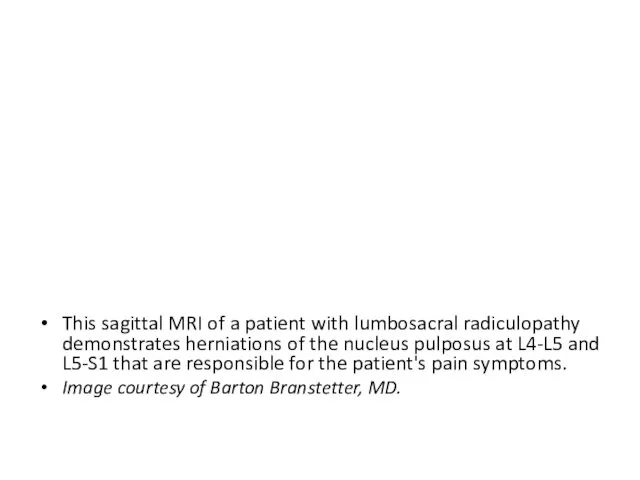
- 34. This sagittal MRI of a patient with lumbosacral radiculopathy demonstrates herniations of the nucleus pulposus at
- 35. Medical management of pain proceeds in a stepwise fashion, as shown here (adapted from the WHO
- 36. Pain management Acute pain is typically treated with short courses of pharmacotherapy, whereas chronic pain may
- 37. Medication 1. Analgesics are commonly used for many pain syndromes. Pain control is essential to quality
- 38. Medication 2. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) have analgesic, anti-inflammatory, and antipyretic activities. Their mechanism of action
- 39. Medication 3. Anticonvulsants. Certain antiepileptic drugs (eg, the gamma-aminobutyric acid [GABA] analogue gabapentin and pregabalin) have
- 40. Medication 4. Muscle spasmolytics are traditionally used to treat painful musculoskeletal disorders. As a class, they
- 41. Medication 5. Antidepressants. Tricyclic antidepressants (TCAs) are commonly used in chronic pain treatment to alleviate insomnia,
- 42. The pharmacology of pain control hinges on influencing one of several biochemical pathways. Many nonnarcotic analgesics
- 43. Image of a PCA infusion pump configured for epidural administration of fentanyl and bupivacaine for postoperative
- 44. Transdermal patches provide controlled drug delivery with a lower potential for abuse than is present with
- 45. Regional anesthesia with therapeutic injections can provide excellent relief for patients with localized pain and inflammation.
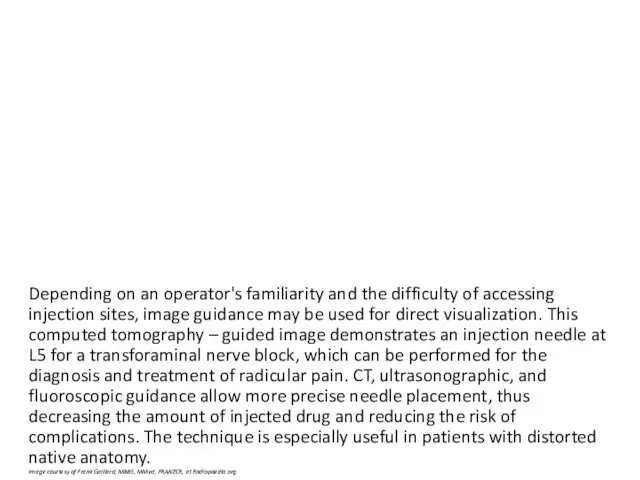
- 46. Depending on an operator's familiarity and the difficulty of accessing injection sites, image guidance may be
- 47. Surgical interventions are generally limited to patients with discrete deficits whose condition does not improve with
- 48. Spinal cord stimulation (SCS) is approved by the US FDA to relieve intractable pain. Indications include
- 49. A transcutaneous electrical nerve stimulation (TENS) unit is an adjuvant pain control device that provides pulsatile
- 51. Скачать презентацию

![Image courtesy of Legon et al.[6]](/_ipx/f_webp&q_80&fit_contain&s_1440x1080/imagesDir/jpg/45169/slide-5.jpg)

 Веры
Веры Төрт жылдық цикл мерзімімен өткізілетін сервистік қызмет көрсету (сқ-5 жыл) жалпы ережелер
Төрт жылдық цикл мерзімімен өткізілетін сервистік қызмет көрсету (сқ-5 жыл) жалпы ережелер Создание презентации
Создание презентации Презентация к уроку Природные уникумы Урала. Экологические проблемы.8 класс.
Презентация к уроку Природные уникумы Урала. Экологические проблемы.8 класс. Туберкулез кожи. Виды
Туберкулез кожи. Виды Презентация по технологии 3 класс ОС Школа 2100
Презентация по технологии 3 класс ОС Школа 2100 Первая медицинская помощь при травмах опорно-двигательного аппарата
Первая медицинская помощь при травмах опорно-двигательного аппарата Уважение и понимание: основы терпимости (толерантности)
Уважение и понимание: основы терпимости (толерантности) Автомобили будущего
Автомобили будущего физкультминутка для глаз
физкультминутка для глаз Локальная радиорелейная станция Стрела-0,45М
Локальная радиорелейная станция Стрела-0,45М Уход за больными с переломом шейки бедра
Уход за больными с переломом шейки бедра Briefing HEKO Kataloge
Briefing HEKO Kataloge Искусство Древней Руси Х – ХIV вв
Искусство Древней Руси Х – ХIV вв Корзинка на Пасху
Корзинка на Пасху Принципы работы телевизора и монитора на жидких кристаллах
Принципы работы телевизора и монитора на жидких кристаллах Недарвиновские концепции происхождения человека
Недарвиновские концепции происхождения человека Реконструкция электрических сетей здания. Технические решения и качество исполнения
Реконструкция электрических сетей здания. Технические решения и качество исполнения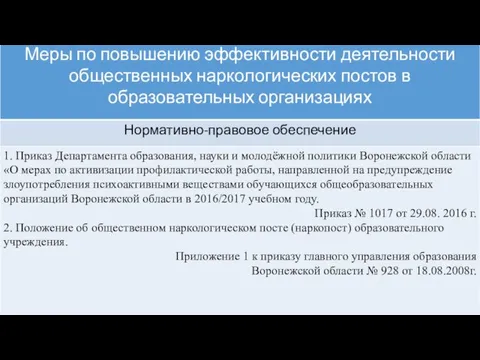 Меры по повышению эффективности деятельности общественных наркологических постов в образовательных организациях
Меры по повышению эффективности деятельности общественных наркологических постов в образовательных организациях Проект Цветущая клумба
Проект Цветущая клумба Наушники и колонки
Наушники и колонки основания
основания Почвы пустынных зон
Почвы пустынных зон Умные технологии в жилых помещениях. История появления. Технология и оборудование для систем умного дома
Умные технологии в жилых помещениях. История появления. Технология и оборудование для систем умного дома Изложение. До первого дождя
Изложение. До первого дождя Тыныс жүйесінің өмірге қауіпті зақымдануларын анықтау мен жедел көмек көрсетудің алгоритмі
Тыныс жүйесінің өмірге қауіпті зақымдануларын анықтау мен жедел көмек көрсетудің алгоритмі Ведение журнала вырабатываемой на предприятии продукции в Меркурий
Ведение журнала вырабатываемой на предприятии продукции в Меркурий Классный час Поговорим о дружбе
Классный час Поговорим о дружбе