Содержание
- 2. Answer: Acute myocardial infarction is the most likely diagnosis. Based on this history alone, electrocardiographic monitoring
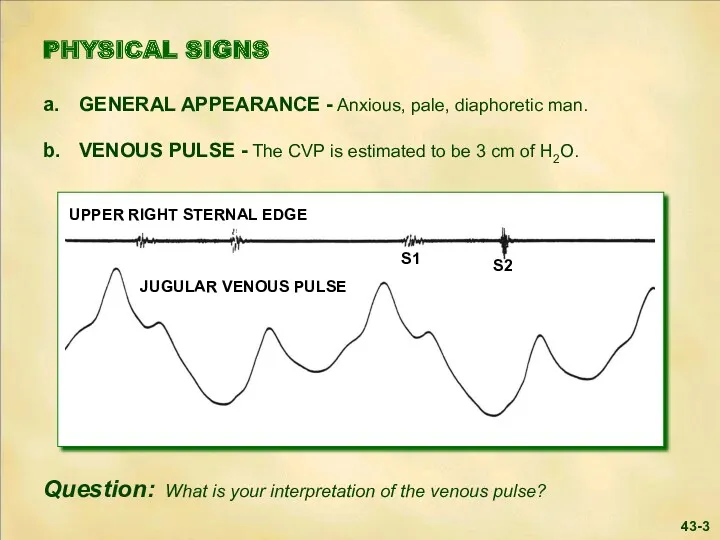
- 3. 43-3
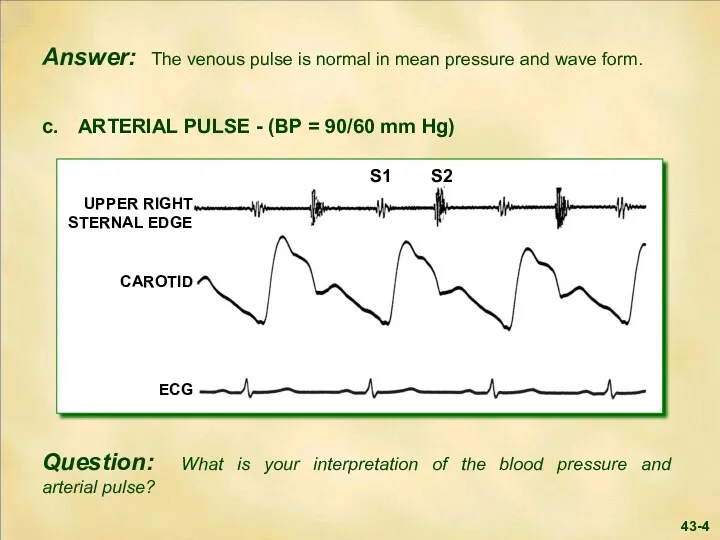
- 4. 43-4
- 5. Answer: The blood pressure is mildly decreased, while the arterial pulse contour is normal. Parasympathetic overactivity
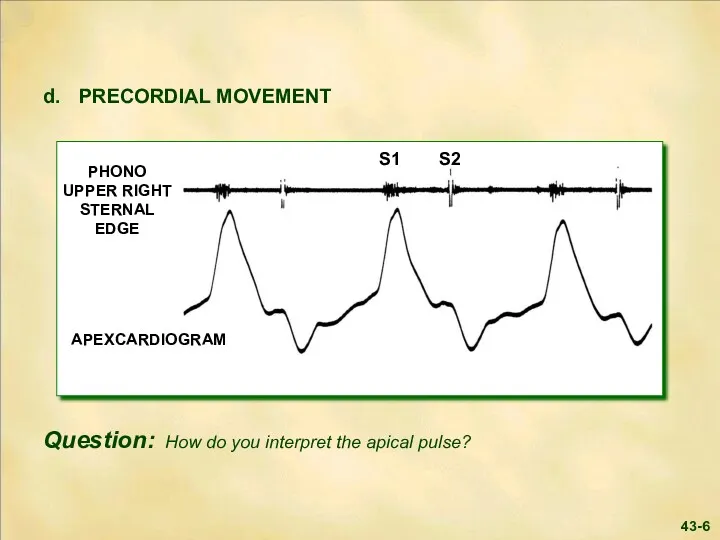
- 6. 43-6 S1 S2
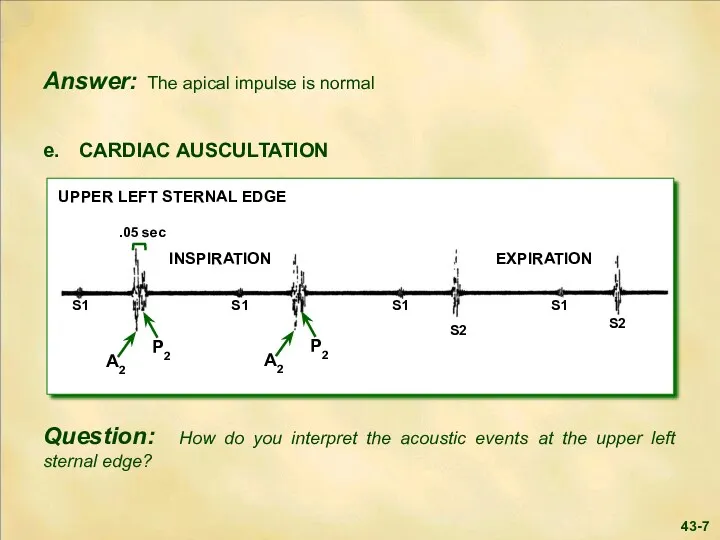
- 7. 43-7
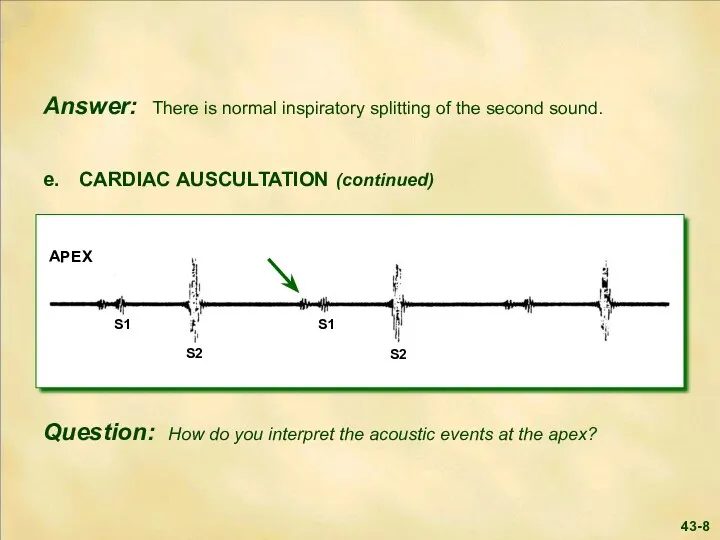
- 8. 43-8
- 9. Answer: The first heart sound at the apex is diminished in intensity. In this clinical setting,
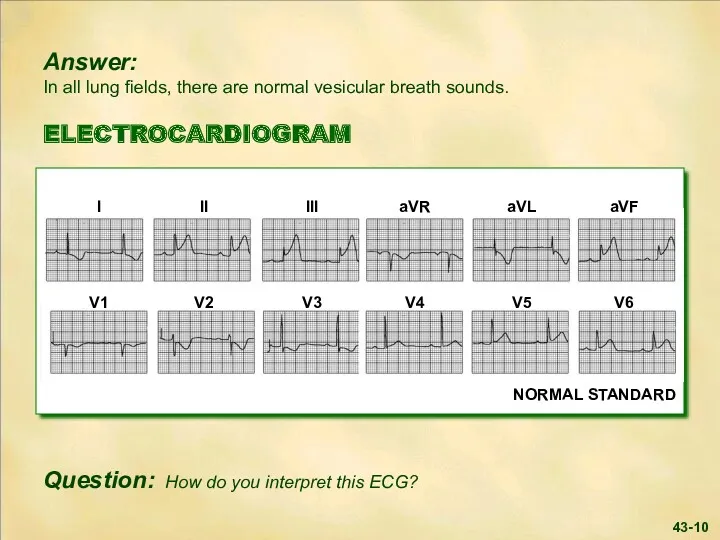
- 10. 43-10
- 11. Answer: The ECG shows marked ST segment elevation in the inferior leads with lesser elevation in
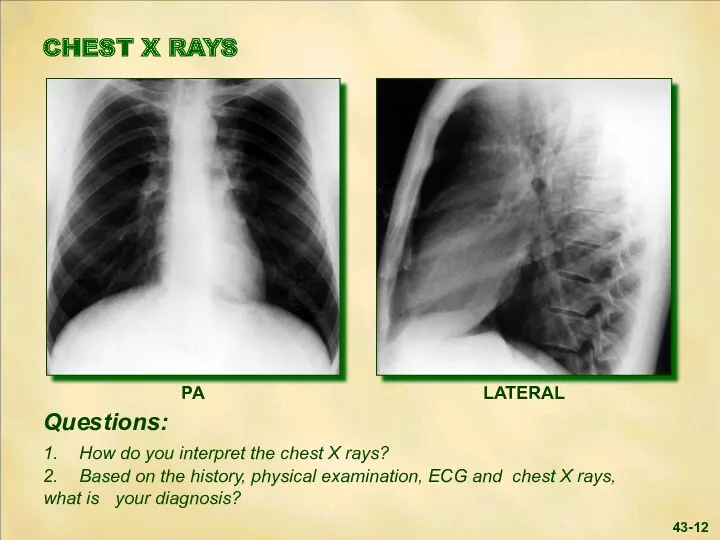
- 12. 43-12
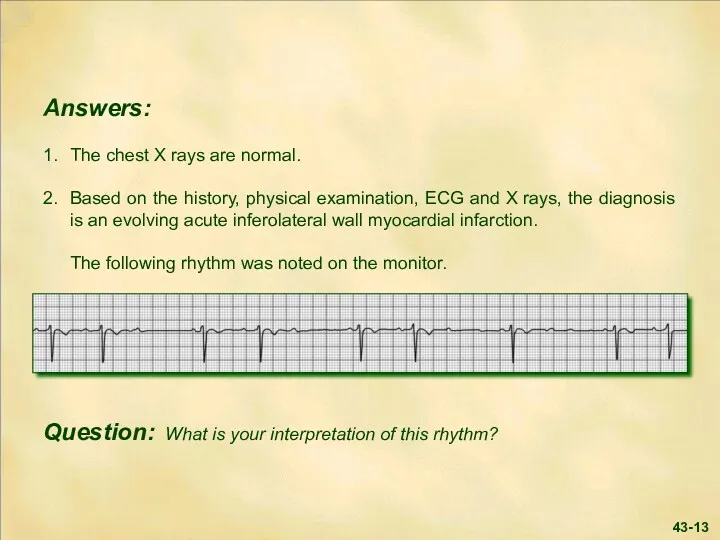
- 13. 43-13
- 14. Answer: The rhythm strip shows sinus rhythm with Mobitz Type I second degree A-V block (
- 15. Answer: Thrombosis plays an important role in ST-elevation myocardial infarction. Timely reperfusion of the occluded coronary
- 16. 43-16 Answer (continued): If full catheterization facilities are available, urgent study and percutaneous intervention is most
- 17. LABORATORY Myocardial biomarkers ordered on admission confirmed the diagnosis of infarction. Necrosis of myocardial tissue results
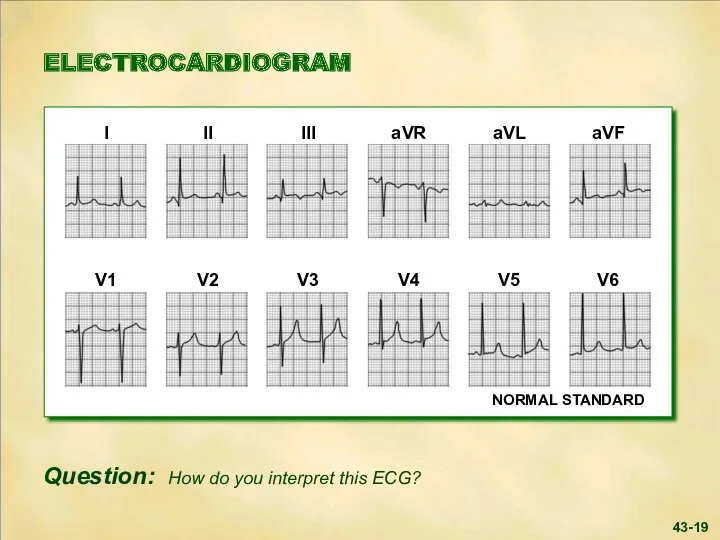
- 18. The patient was placed at bed rest in the CCU. Ninety minutes following thrombolytic therapy, the
- 19. 43-19
- 20. Answer: Typical evolutionary changes of an acute inferior wall myocardial infarction are present: Q waves and
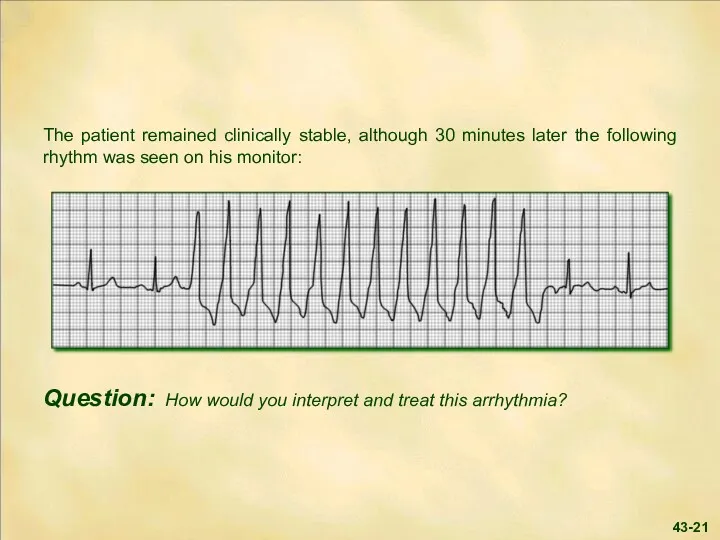
- 21. 43-21
- 22. Answer: There is a run of non-sustained ventricular tachycardia, i.e., three or more ventricular beats in
- 23. Two hours later the patient became cool and clammy, and his blood pressure dropped to 85/50
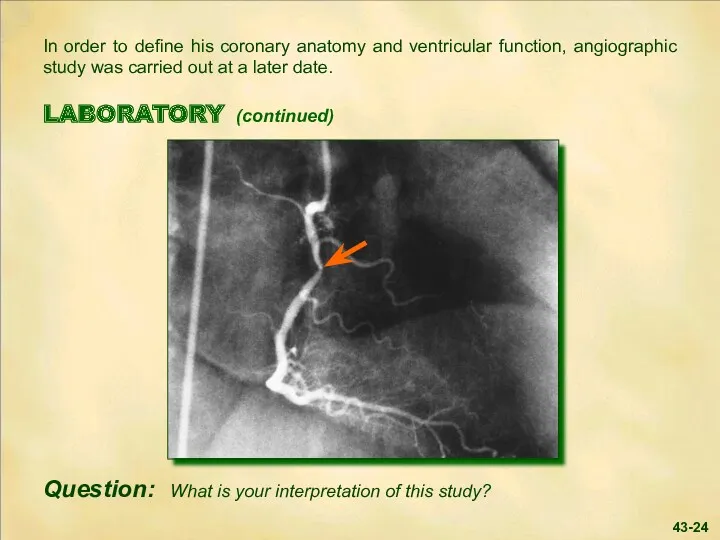
- 24. In order to define his coronary anatomy and ventricular function, angiographic study was carried out at
- 25. Answer: The right coronary angiogram shows an isolated non-critical stenosis (arrow) in the proximal right coronary
- 26. SUMMARY Coronary artery lesions range from the stable atheroma to complex lesions with thrombotic occlusion. The
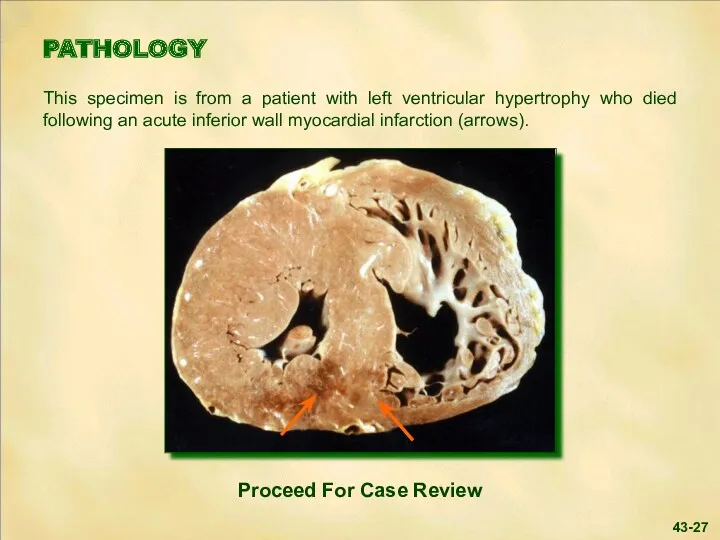
- 27. PATHOLOGY This specimen is from a patient with left ventricular hypertrophy who died following an acute
- 28. 43-28
- 29. 43-29
- 31. Скачать презентацию
 Артериальная гипертензия у беременных
Артериальная гипертензия у беременных Проблема качества жизни в контексте современной трансплантологии
Проблема качества жизни в контексте современной трансплантологии Les inlays-onlays esthétiques Procédures d’assemblage
Les inlays-onlays esthétiques Procédures d’assemblage ВКР: Сравнительная характеристика различных видов коронок и мостовидных протезов
ВКР: Сравнительная характеристика различных видов коронок и мостовидных протезов Hemolytic anemia
Hemolytic anemia Эндоскопические методы диагностики онкологических больных
Эндоскопические методы диагностики онкологических больных Leishmaniasis. Department of Infectious Diseases Leishmaniasis
Leishmaniasis. Department of Infectious Diseases Leishmaniasis ВКР: Деятельность медицинской сестры по уходу и наблюдению за пациентами при ОРВИ
ВКР: Деятельность медицинской сестры по уходу и наблюдению за пациентами при ОРВИ Острые нейроинфекции. Менингиты
Острые нейроинфекции. Менингиты Репродуктивне здоров’я молоді
Репродуктивне здоров’я молоді Оснащение формирований службы медицины катастроф по оказанию медицинской помощи в чрезвычайных ситуациях
Оснащение формирований службы медицины катастроф по оказанию медицинской помощи в чрезвычайных ситуациях Masaje al tejido conectivo
Masaje al tejido conectivo Синдром острой и хронической печеночной недостаточности
Синдром острой и хронической печеночной недостаточности Долікарська допомога
Долікарська допомога Эпилепсия
Эпилепсия Мимические мышцы лица
Мимические мышцы лица Вирусы, друзья и враги
Вирусы, друзья и враги Сестринский уход при различных заболеваниях и состояниях раздел Сестринская помощь в хирургии
Сестринский уход при различных заболеваниях и состояниях раздел Сестринская помощь в хирургии Методы обследования пациентов с патологией органов сердечно-сосудистой системы: пальпация, перкуссия, аускультация
Методы обследования пациентов с патологией органов сердечно-сосудистой системы: пальпация, перкуссия, аускультация Организация и содержание государственного ветеринарного надзора
Организация и содержание государственного ветеринарного надзора Острый живот в гинекологии
Острый живот в гинекологии Питание кормящей матери
Питание кормящей матери Анксиолитики (транквилизаторы)
Анксиолитики (транквилизаторы) Инфекционные болезни собак
Инфекционные болезни собак Токсические поражения печени
Токсические поражения печени Система здравоохранения в России
Система здравоохранения в России Тиреоидиты. Классификация
Тиреоидиты. Классификация Выделительная система
Выделительная система