Слайд 2
Definition
Bronchial asthma is a chronic, inflammatory disease of the respiratory tract,
which is characterized by bronchial hyperreactivity and respiratory obstruction.
Слайд 3
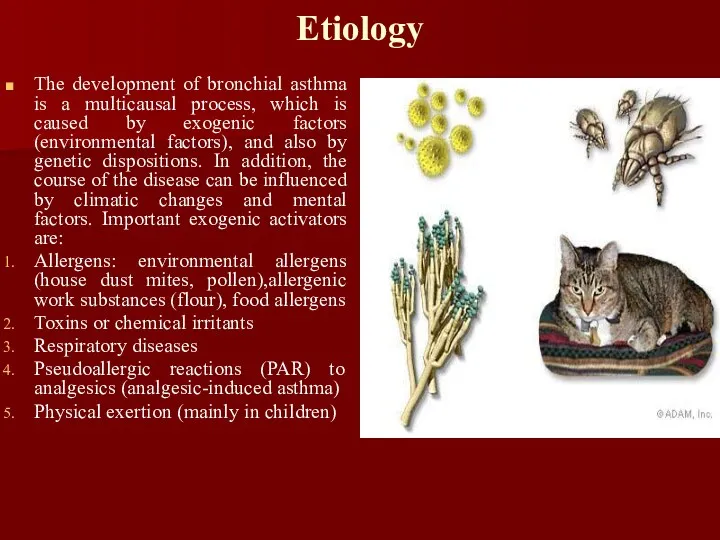
Etiology
The development of bronchial asthma is a multicausal process, which
is caused by exogenic factors (environmental factors), and also by genetic dispositions. In addition, the course of the disease can be influenced by climatic changes and mental factors. Important exogenic activators are:
Allergens: environmental allergens (house dust mites, pollen),allergenic work substances (flour), food allergens
Toxins or chemical irritants
Respiratory diseases
Pseudoallergic reactions (PAR) to analgesics (analgesic-induced asthma)
Physical exertion (mainly in children)
Слайд 4
Epidemiology
As a rule, bronchial asthma already occurs in infancy and is
the most common chronic disease of this stage of life.
Слайд 5
Classification
According to etiology
Allergic or extrinsic asthma
Non-allergic or intrinsic asthma
Mixed forms
According
to degree of severity
Grade 1: Intermittent
Grade 2: Persistent, mild (symptoms more than twice a week, but no more than once in a single day )
Grade 3: Persistent, moderate (symptoms once a day and more than one night a week )
Grade 4: Persistent, severe (symptoms throughout the day on most days and frequently at night )
Слайд 6
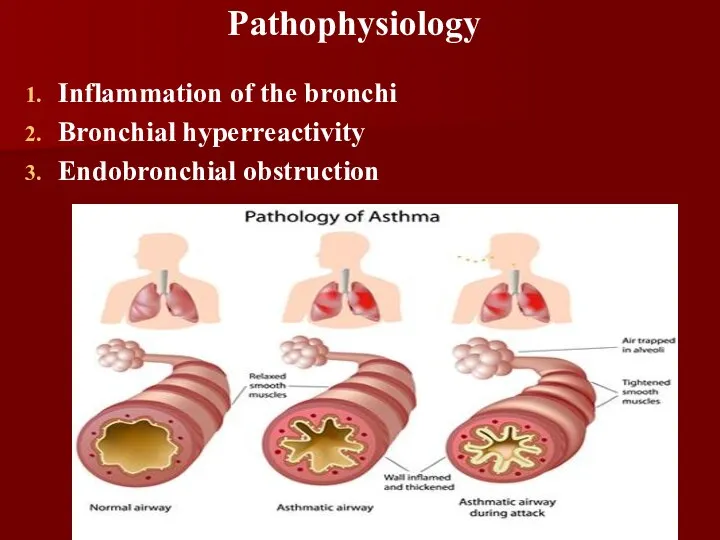
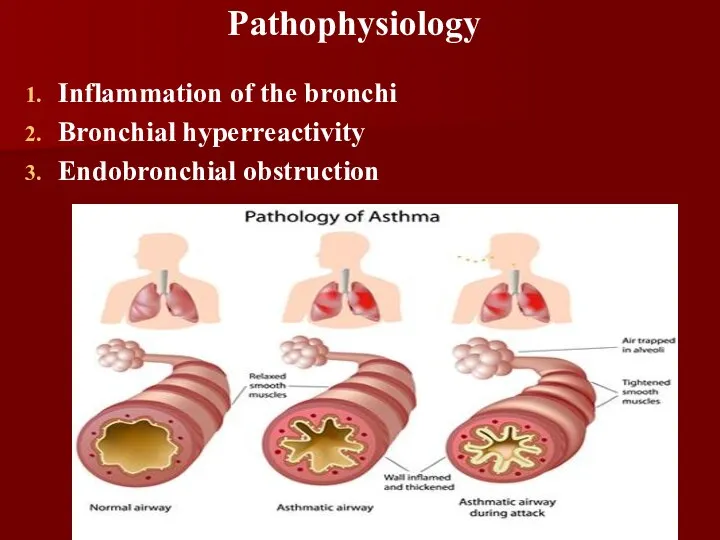
Pathophysiology
Inflammation of the bronchi
Bronchial hyperreactivity
Endobronchial obstruction
Слайд 7
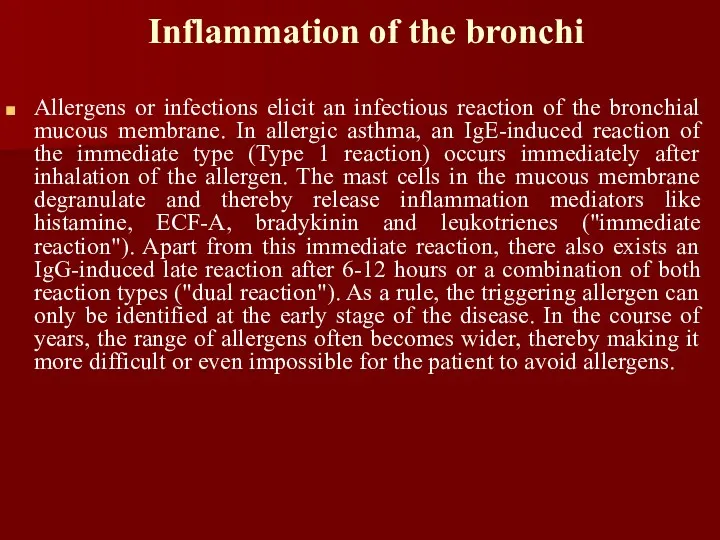
Inflammation of the bronchi
Allergens or infections elicit an infectious reaction of
the bronchial mucous membrane. In allergic asthma, an IgE-induced reaction of the immediate type (Type 1 reaction) occurs immediately after inhalation of the allergen. The mast cells in the mucous membrane degranulate and thereby release inflammation mediators like histamine, ECF-A, bradykinin and leukotrienes ("immediate reaction"). Apart from this immediate reaction, there also exists an IgG-induced late reaction after 6-12 hours or a combination of both reaction types ("dual reaction"). As a rule, the triggering allergen can only be identified at the early stage of the disease. In the course of years, the range of allergens often becomes wider, thereby making it more difficult or even impossible for the patient to avoid allergens.
Слайд 8
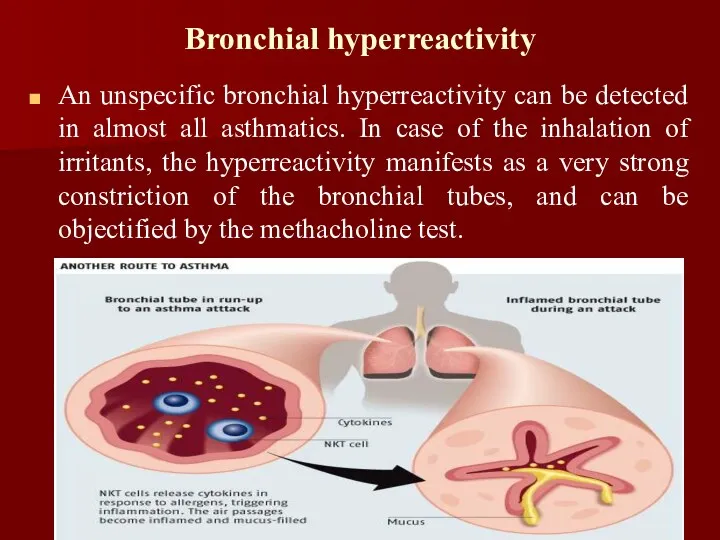
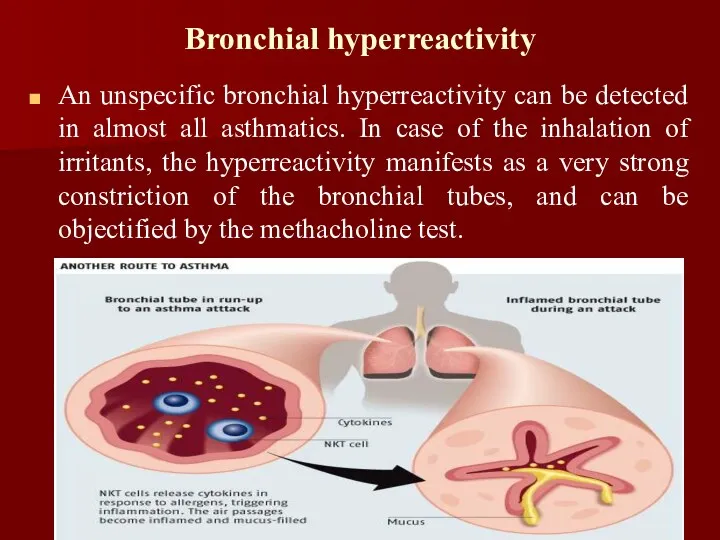
Bronchial hyperreactivity
An unspecific bronchial hyperreactivity can be detected in almost all
asthmatics. In case of the inhalation of irritants, the hyperreactivity manifests as a very strong constriction of the bronchial tubes, and can be objectified by the methacholine test.
Слайд 9
Endobronchial obstruction
The endobronchial obstruction is quasi the first clinically discernible
"end product" of the pathophysiological processes of bronchial asthma. It develops through the shift of the bronchial lumen as a consequence of mucosal edema, increased mucus secretion (dyscrinism) and bronchospasms.
Слайд 10
Symptoms
Cough with or without sputum (phlegm) production
Pulling in of the skin
between the ribs when breathing (intercostal retractions)
Shortness of breath that gets worse with exercise or activity
Wheezing
Emergency symptoms that need prompt medical help:
Bluish color to the lips and face
Decreased level of alertness, such as severe drowsiness or confusion, during an asthma attack
Extreme difficulty breathing
Rapid pulse
Severe anxiety due to shortness of breath
Sweating
Other symptoms that may occur:
Abnormal breathing pattern --breathing out takes more than twice as long as breathing in
Breathing temporarily stops
Chest pain
Tightness in the chest
Слайд 11

Слайд 12
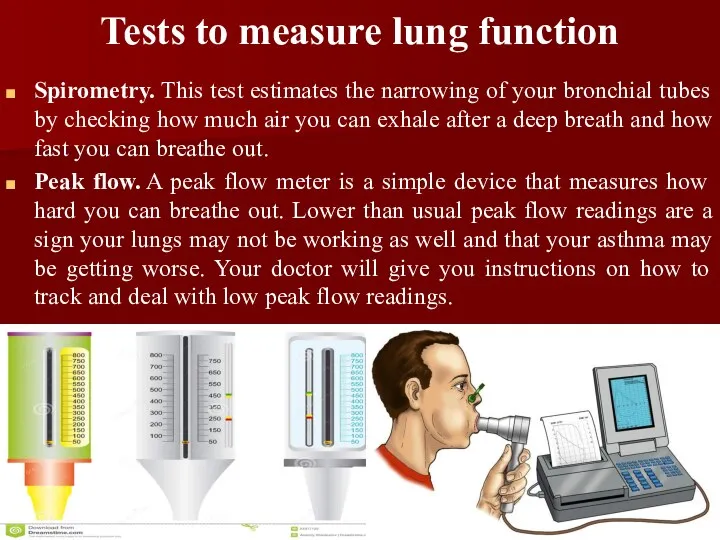
Tests to measure lung function
Spirometry. This test estimates the narrowing of your
bronchial tubes by checking how much air you can exhale after a deep breath and how fast you can breathe out.
Peak flow. A peak flow meter is a simple device that measures how hard you can breathe out. Lower than usual peak flow readings are a sign your lungs may not be working as well and that your asthma may be getting worse. Your doctor will give you instructions on how to track and deal with low peak flow readings.
Слайд 13
Additional tests
Methacholine challenge. Methacholine is a known asthma trigger that, when inhaled,
will cause mild constriction of your airways. If you react to the methacholine, you likely have asthma. This test may be used even if your initial lung function test is normal.
Imaging tests. A chest X-ray and high-resolution computerized tomography (CT) scan of your lungs and nose cavities (sinuses) can identify any structural abnormalities or diseases (such as infection) that can cause or aggravate breathing problems.
Слайд 14
Additional tests
Allergy testing. This can be performed by a skin test or
blood test. Allergy tests can identify allergy to pets, dust, mold and pollen. If important allergy triggers are identified, this can lead to a recommendation for allergen immunotherapy.
Provocative testing for exercise and cold-induced asthma.In these tests, your doctor measures your airway obstruction before and after you perform vigorous physical activity or take several breaths of cold air.
Слайд 15
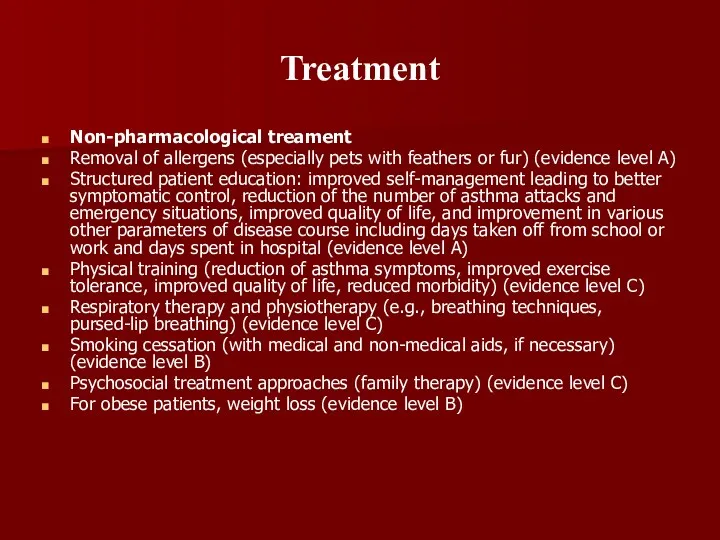
Treatment
Non-pharmacological treament
Removal of allergens (especially pets with feathers or fur) (evidence
level A)
Structured patient education: improved self-management leading to better symptomatic control, reduction of the number of asthma attacks and emergency situations, improved quality of life, and improvement in various other parameters of disease course including days taken off from school or work and days spent in hospital (evidence level A)
Physical training (reduction of asthma symptoms, improved exercise tolerance, improved quality of life, reduced morbidity) (evidence level C)
Respiratory therapy and physiotherapy (e.g., breathing techniques, pursed-lip breathing) (evidence level C)
Smoking cessation (with medical and non-medical aids, if necessary) (evidence level B)
Psychosocial treatment approaches (family therapy) (evidence level C)
For obese patients, weight loss (evidence level B)
Слайд 16
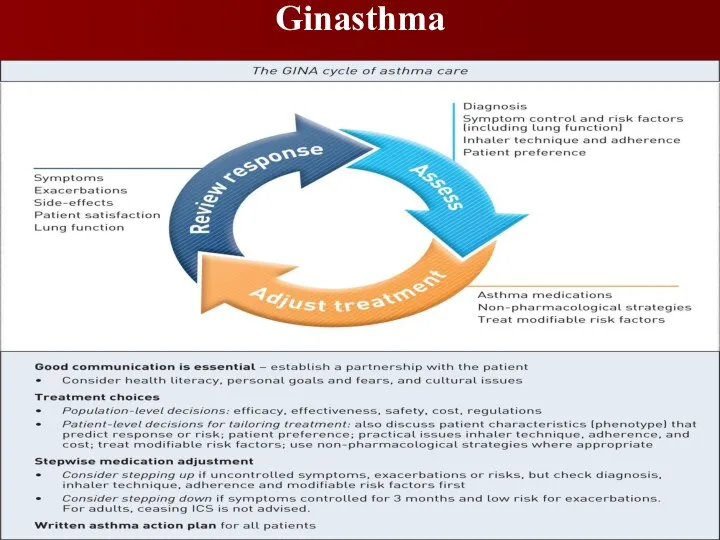
Слайд 17
GINA
The Global Initiative for Asthma (GINA) was established in 1993 by
the World Health Organization and National Heart Lung and Blood Institute to develop a global strategy for managing and preventing asthma. GINA reports, now funded independently through the sale of GINA products, have provided the foundation for many national guidelines. They are prepared by international experts from primary, secondary and tertiary care, and are annually updated following a review of evidence.

 Осложнения фармакотерапии противомикробными средствами
Осложнения фармакотерапии противомикробными средствами Charcot-Marie Tooth disease (CMT)
Charcot-Marie Tooth disease (CMT) Организация работы родильного дома, женской консультации
Организация работы родильного дома, женской консультации Гестационный пиелонефрит у беременных женщин
Гестационный пиелонефрит у беременных женщин Бронхиальді тал құрылысы
Бронхиальді тал құрылысы Анемиялық синдром. Этиологиясы. Классификациясы. Патоморфологиялық сипаттамасы
Анемиялық синдром. Этиологиясы. Классификациясы. Патоморфологиялық сипаттамасы Сахарный диабет. Определение
Сахарный диабет. Определение Опухолеподобные заболевания костей. Дифференциальная диагностика
Опухолеподобные заболевания костей. Дифференциальная диагностика Пиелонефрит. Классификация
Пиелонефрит. Классификация Различия профессиональной косметики (ПКП) по возрастным критериям
Различия профессиональной косметики (ПКП) по возрастным критериям Актуализированы списки детей категории: ребенок-инвалид
Актуализированы списки детей категории: ребенок-инвалид Костные опухоли
Костные опухоли Классификация и морфология опухолей
Классификация и морфология опухолей Осложнения на этапе установки дентальных имплантатов
Осложнения на этапе установки дентальных имплантатов Косоглазие. Глазодвигательный аппарат
Косоглазие. Глазодвигательный аппарат Рецидивирующие эрозии роговицы – особенности возникновения и лечения
Рецидивирующие эрозии роговицы – особенности возникновения и лечения Топографическая анатомия и оперативная хирургия нервов. (Лекция 5)
Топографическая анатомия и оперативная хирургия нервов. (Лекция 5) Ведение беременности и родов у ВИЧ-инфицированных
Ведение беременности и родов у ВИЧ-инфицированных Инфекциялық үрдістің патофизиологиясы
Инфекциялық үрдістің патофизиологиясы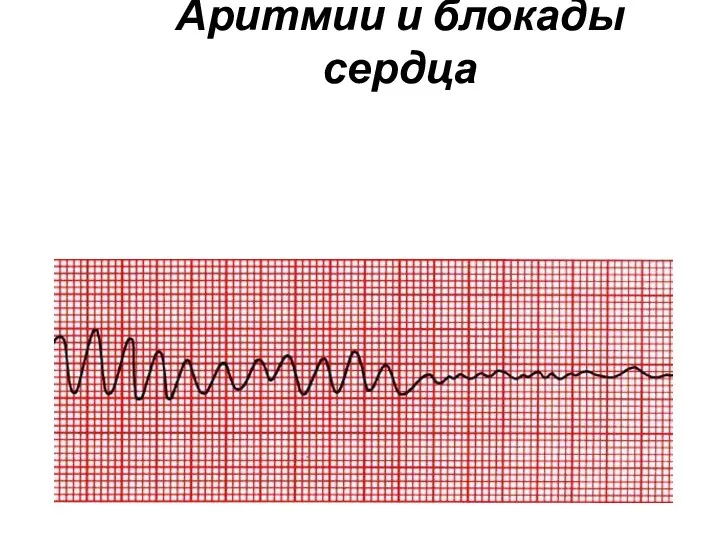 Аритмии и блокады сердца
Аритмии и блокады сердца Хирургиялық стоматологиядағы дәлелді медицина
Хирургиялық стоматологиядағы дәлелді медицина Асқазан ішек жолдарының эрозивті жаралы зақымдануына әкелетін ықпал ететін тіс жақ аймағының аурулары
Асқазан ішек жолдарының эрозивті жаралы зақымдануына әкелетін ықпал ететін тіс жақ аймағының аурулары Анафилактикалық шок
Анафилактикалық шок Неінфекційні захворювання. Урок №12. Здоров'я, безпека та добробут. 6 клас
Неінфекційні захворювання. Урок №12. Здоров'я, безпека та добробут. 6 клас Этика и деонтология фармацевтического работника
Этика и деонтология фармацевтического работника Первая помощь при ранениях и травмах
Первая помощь при ранениях и травмах Личностные особенности пациентов с различными хроническими соматическими заболеваниями
Личностные особенности пациентов с различными хроническими соматическими заболеваниями Физические основы электрокардиографии
Физические основы электрокардиографии