Содержание
- 2. Definition Bronchiectasis - uncommon disease, most often secondary to an infectious process, that results in the
- 3. ERS guidelines for the management of adult bronchiectasis (Eva Polverino, Pieter C. Goeminne, Melissa J. European
- 4. Classification by etiology 1. Genetic disorders (cystic fibrosis, primary ciliary dyskinesia, alpha1-antitrypsin deficiency) 2. Post infectious
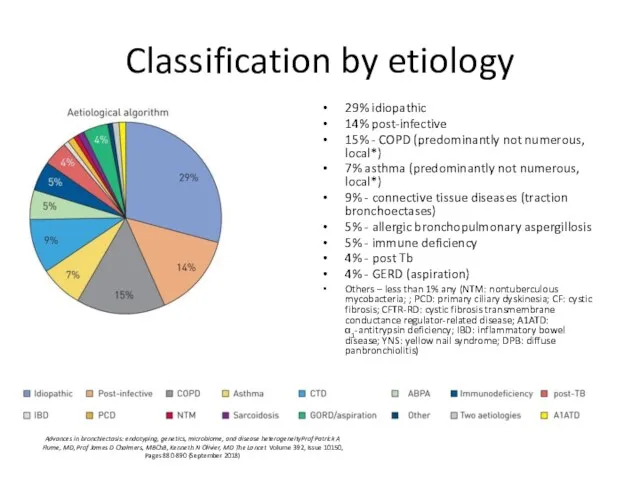
- 5. Classification by etiology 29% idiopathic 14% post-infective 15% - COPD (predominantly not numerous, local*) 7% asthma
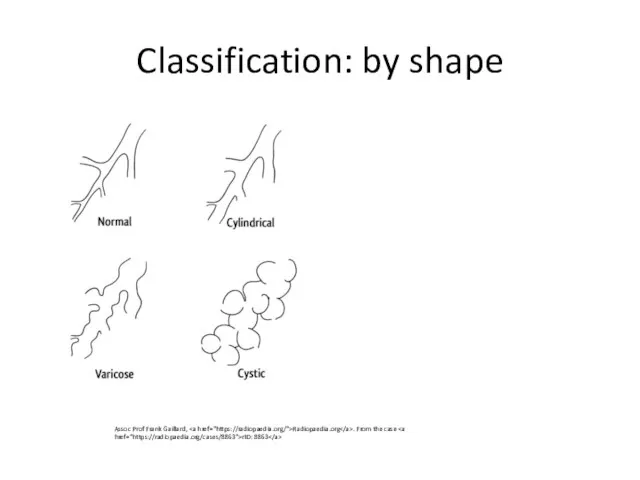
- 6. Classification: by shape Assoc Prof Frank Gaillard, Radiopaedia.org . From the case rID: 8863
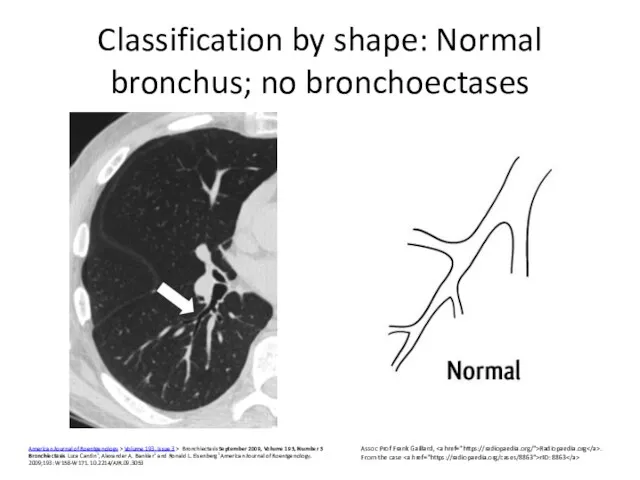
- 7. Classification by shape: Normal bronchus; no bronchoectases American Journal of Roentgenology > Volume 193, Issue 3
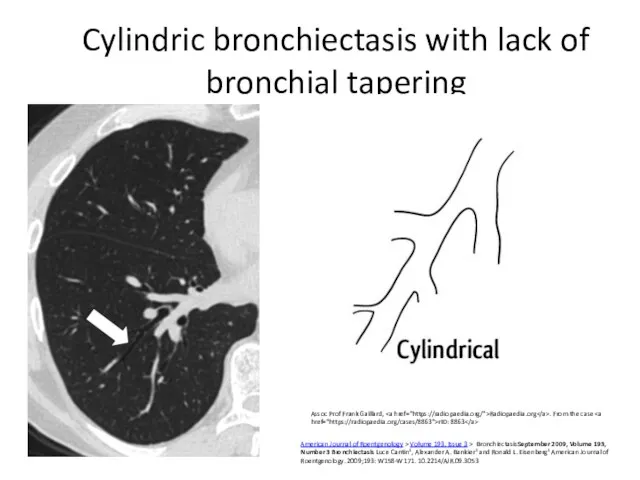
- 8. Cylindric bronchiectasis with lack of bronchial tapering Assoc Prof Frank Gaillard, Radiopaedia.org . From the case
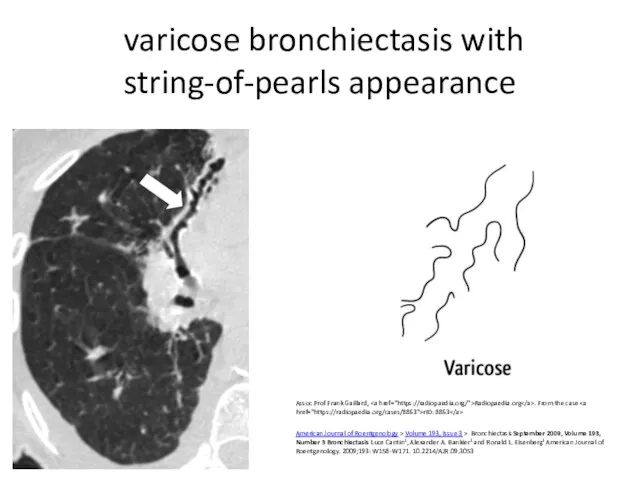
- 9. varicose bronchiectasis with string-of-pearls appearance Assoc Prof Frank Gaillard, Radiopaedia.org . From the case rID: 8863
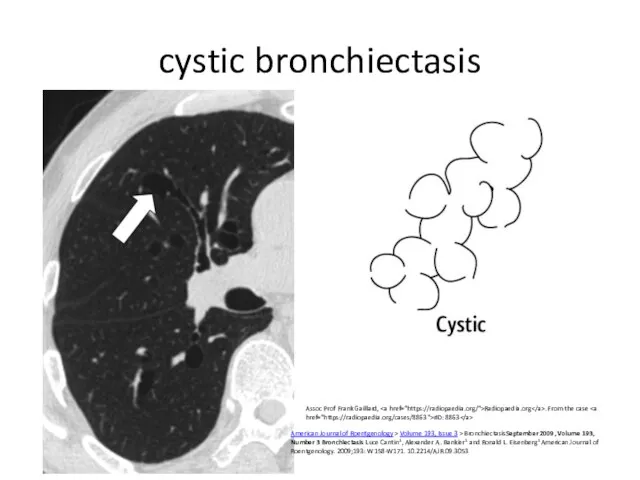
- 10. cystic bronchiectasis American Journal of Roentgenology > Volume 193, Issue 3 > BronchiectasisSeptember 2009, Volume 193,
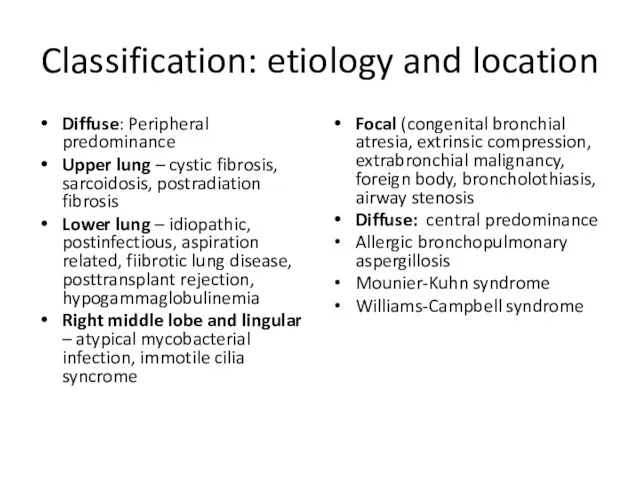
- 11. Classification: etiology and location Focal (congenital bronchial atresia, extrinsic compression, extrabronchial malignancy, foreign body, broncholothiasis, airway
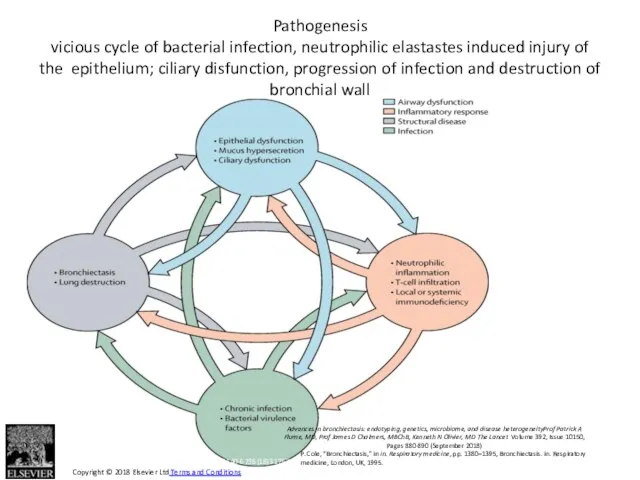
- 12. Figure 1 The Lancet 2018 392, 880-890DOI: (10.1016/S0140-6736(18)31767-7) Copyright © 2018 Elsevier Ltd Terms and Conditions
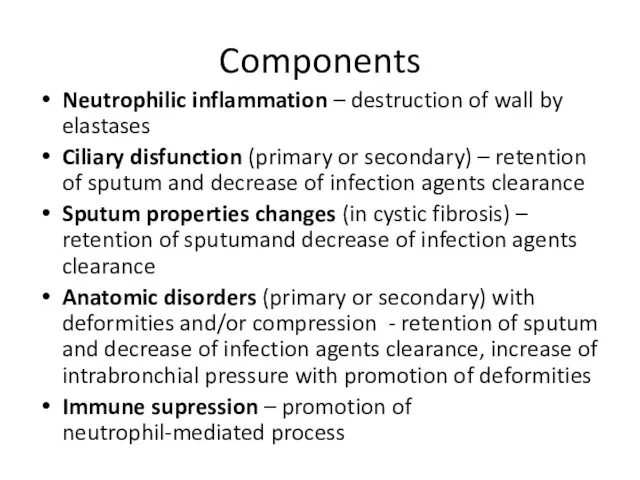
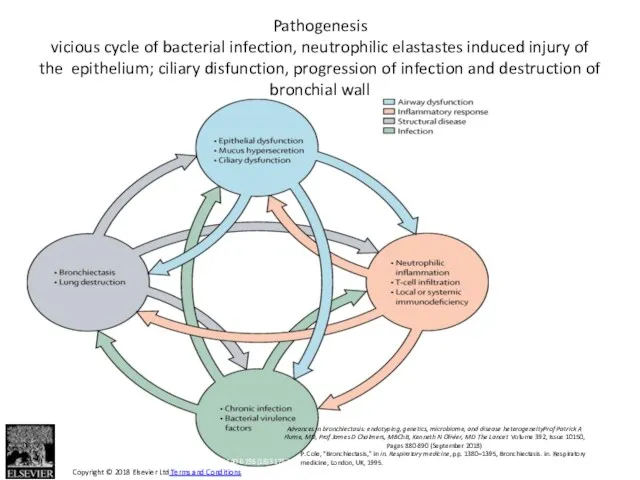
- 13. Components Neutrophilic inflammation – destruction of wall by elastases Ciliary disfunction (primary or secondary) – retention
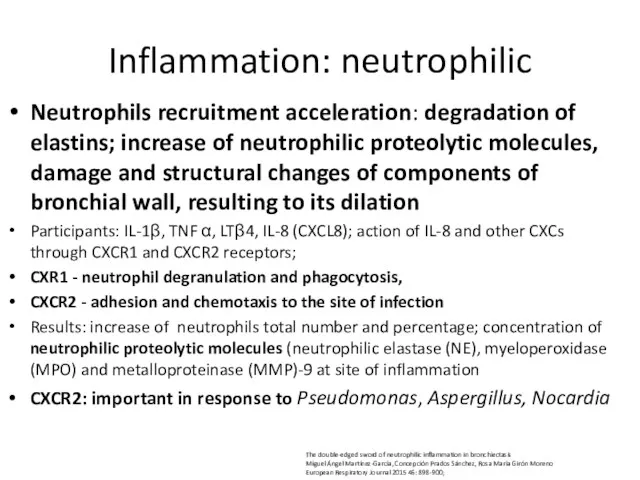
- 14. Inflammation: neutrophilic Neutrophils recruitment acceleration: degradation of elastins; increase of neutrophilic proteolytic molecules, damage and structural
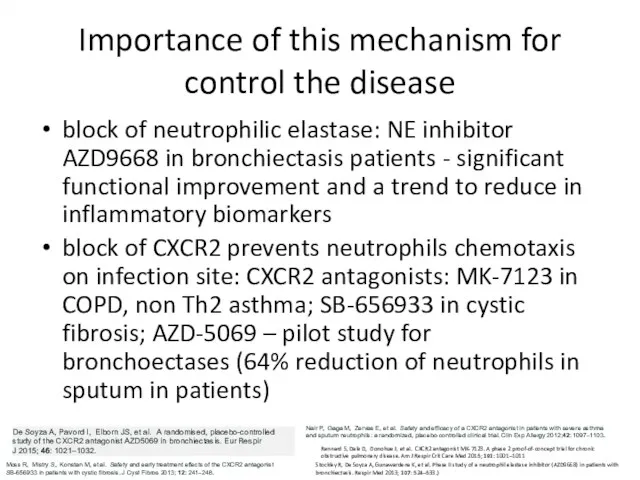
- 15. Importance of this mechanism for control the disease block of neutrophilic elastase: NE inhibitor AZD9668 in
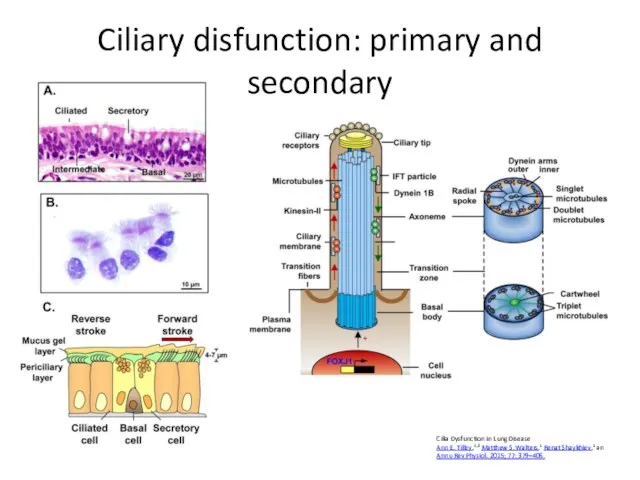
- 16. Ciliary disfunction: primary and secondary Cilia Dysfunction in Lung Disease Ann E. Tilley,1,2 Matthew S. Walters,1
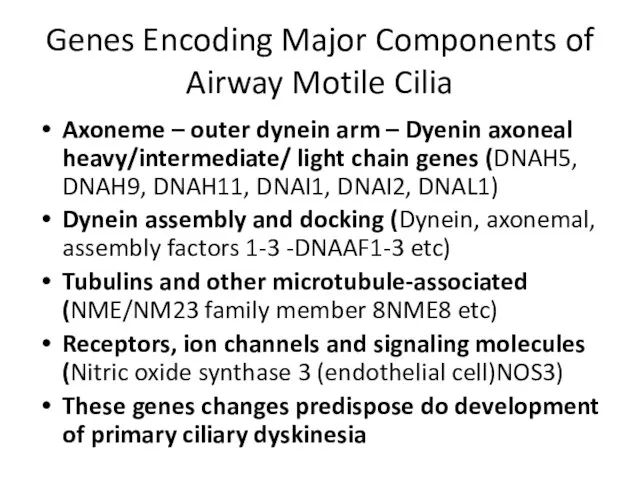
- 17. Genes Encoding Major Components of Airway Motile Cilia Axoneme – outer dynein arm – Dyenin axoneal
- 18. Secondary ciliary disfunction Viruses Bacterial mediators - H. influenzae, P. aeruginosa, Streptococcus pneumoniae (direct damage) Smoking
- 19. Primary and secondary mucociliary clearance disturbance leads to airway dehydration, excess mucus volume and viscosity. Increase
- 20. Primary anatomical changes, promoting clearance disorders due to bronchi deformities or compression Traction bronchoectases – advanced
- 21. Flora Haemophilus influenzae (29%–70%) Pseudomonas aeruginosa (12%–31%). No pathogenic bacteria (30%–40% ) Best preserved lung function:
- 22. Effects of flora promoting bronchoectases inhibition of the mucociliary clearance: mediators of H. influenzae, P. aeruginosa,
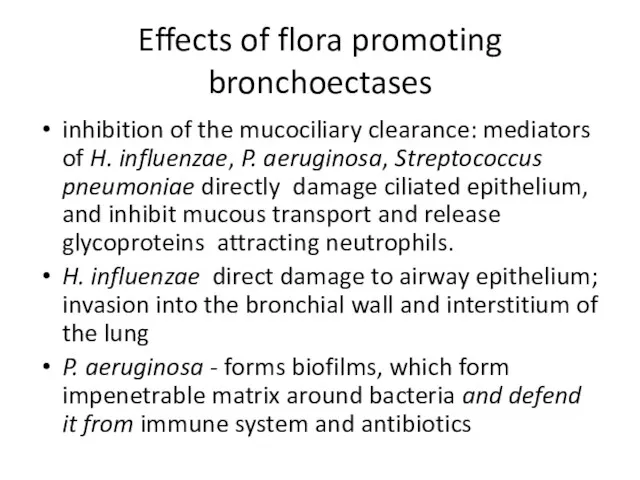
- 23. Immune dysfunction Malnutrition Extremes of age hypogammaglobulinemia, human immunodeficiency virus (HIV), interferon gamma receptor deficiency, type
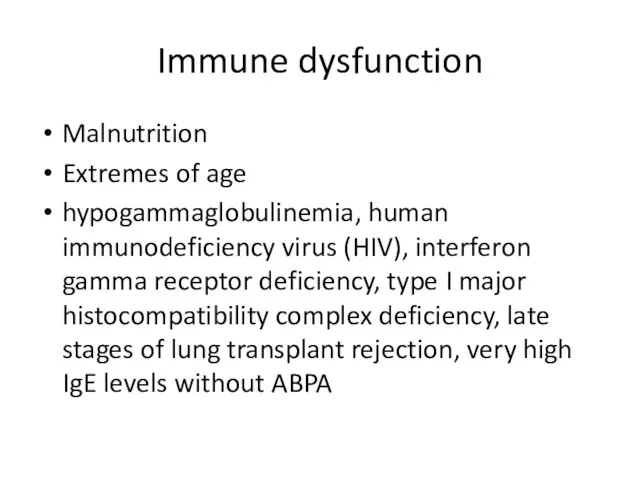
- 24. Figure 1 The Lancet 2018 392, 880-890DOI: (10.1016/S0140-6736(18)31767-7) Copyright © 2018 Elsevier Ltd Terms and Conditions
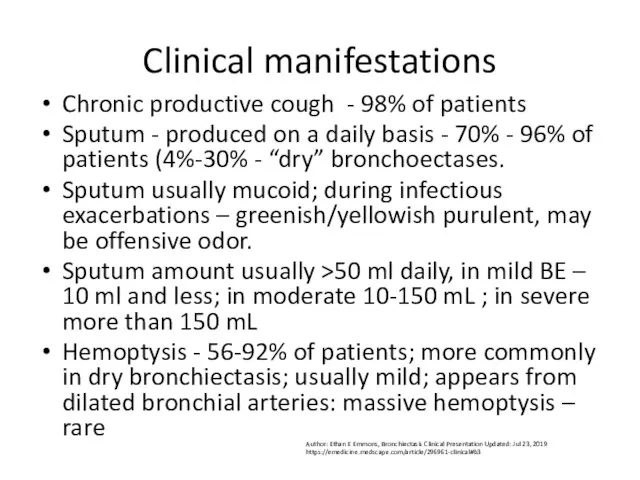
- 25. Clinical manifestations Chronic productive cough - 98% of patients Sputum - produced on a daily basis
- 26. Dyspnea – 62%-72% of patients, mixed (obstruction + restriction due to fibrosis) Wheezing – rare (more
- 27. In whom should be suspected? Persistent mucopurulent/purulent sputum + risk factors rheumatoid arthritis + chronic productive
- 28. Diagnosis: to confirm baseline chest X-ray in patients with suspected bronchiectasis. Thin section computed tomography scan
- 29. CT features of bronchiectasis bronchial dilatation as suggested by one or more of the following: Bronchoarterial
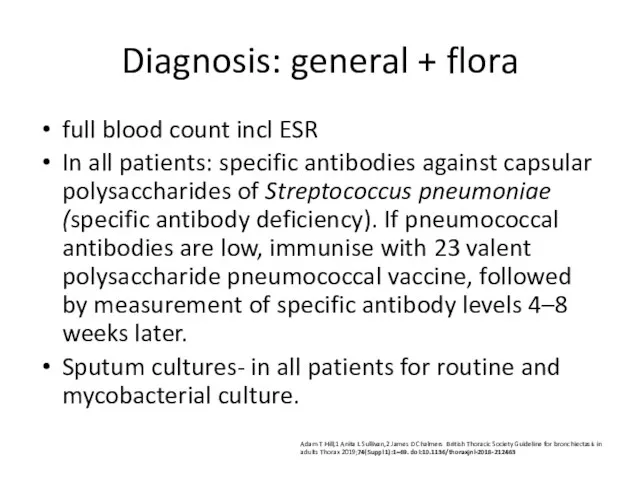
- 30. Diagnosis: general + flora full blood count incl ESR In all patients: specific antibodies against capsular
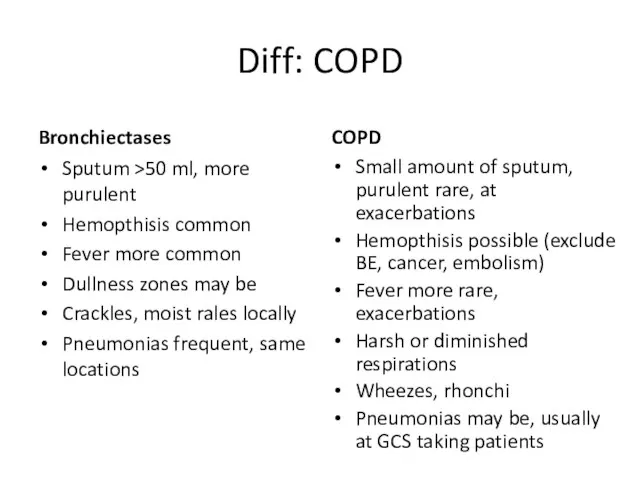
- 31. Diff: COPD Bronchiectases Sputum >50 ml, more purulent Hemopthisis common Fever more common Dullness zones may
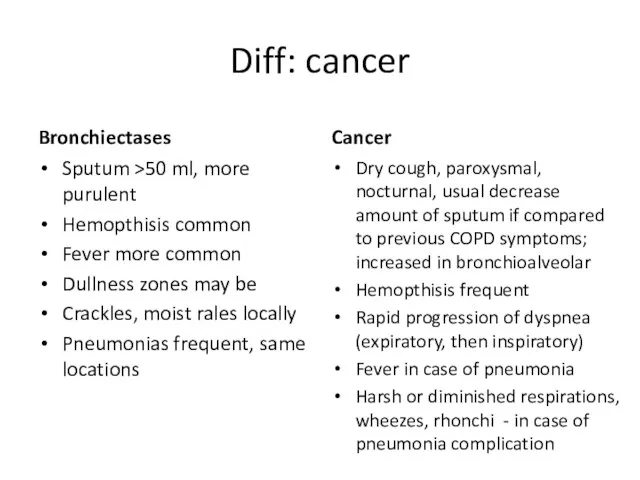
- 32. Diff: cancer Bronchiectases Sputum >50 ml, more purulent Hemopthisis common Fever more common Dullness zones may
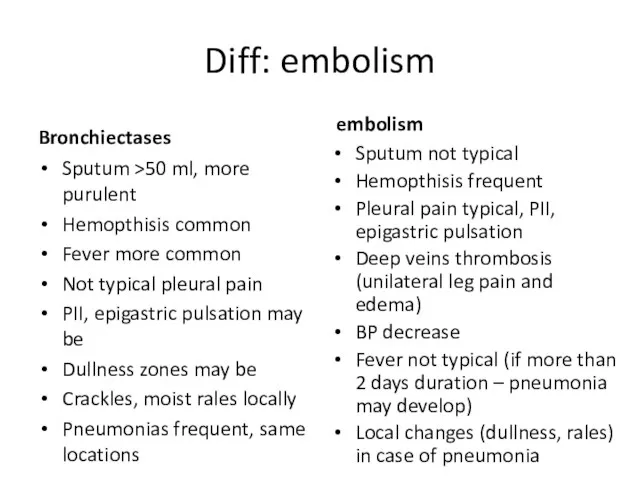
- 33. Diff: embolism Bronchiectases Sputum >50 ml, more purulent Hemopthisis common Fever more common Not typical pleural
- 34. Rare syndroms (ciliary disfunction, cystic fibrosis) Cystic fibrosis Fetal meconium ilius may be Start in early
- 35. Cystic fibrosis predominance of cystic bronchiectasis (arrows) volume loss (fibrosis) diffuse heterogeneous attenuation enlarged lung volumes
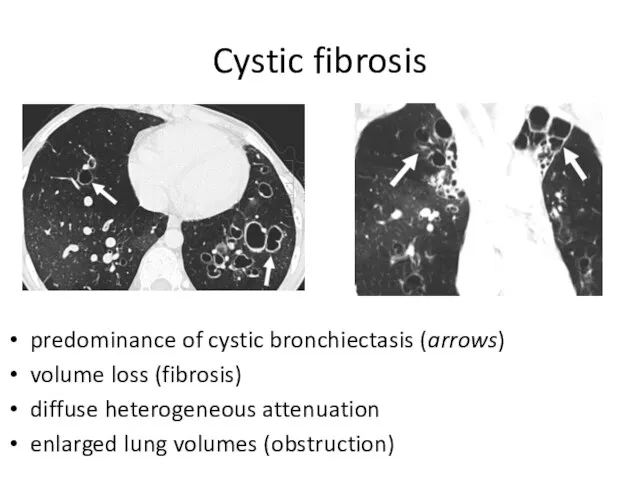
- 36. Adult cystic fibrosis (milder case) cylindric bronchiectasis (white arrows) bronchiolitis (black arrows) – tree in bud
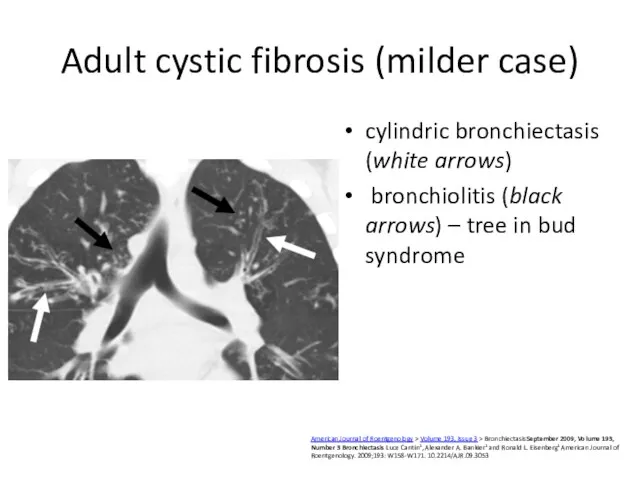
- 37. Kartagener's syndrome Dextrocardia (here + cardiomegaly) Here - left middle lobe bronchiectasis, volume loss. Arrow points
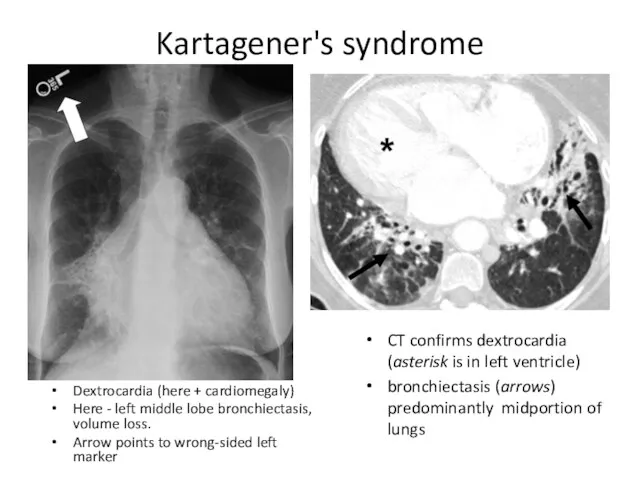
- 38. Other endotypes Alpha -1 antitripsin deficiency Panacinar basal emphysema in non-smokers Liver cirrhosis Non-TB mycobacteria post-menopausal
- 39. Sarcoidosis Diffuse fibrosis traction bronchiectasis (arrows, B) predominantly upper lobes. American Journal of Roentgenology > Volume
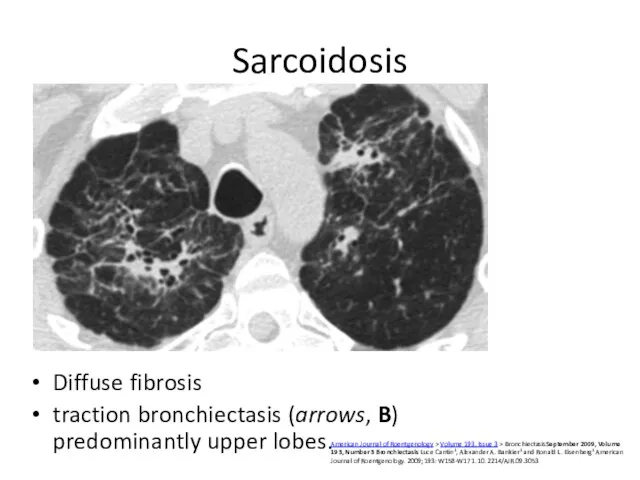
- 40. Usual interstitial pneumonia (idiopathic pulmonary fibrosis; rheumatoid arthritis, more rare Sjogren, scleroderma) Bibasilar and subpleural reticulation
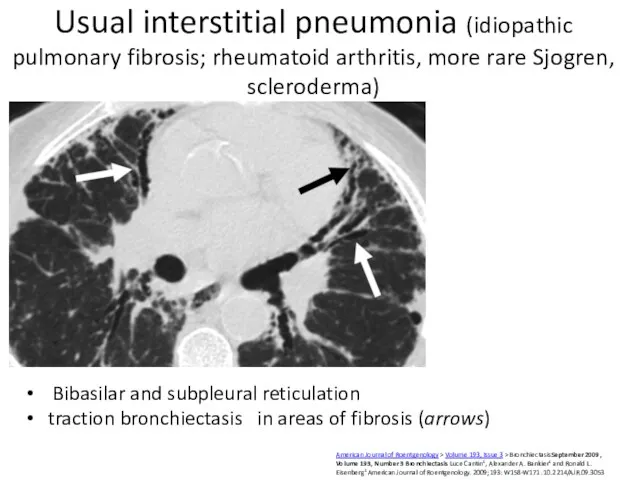
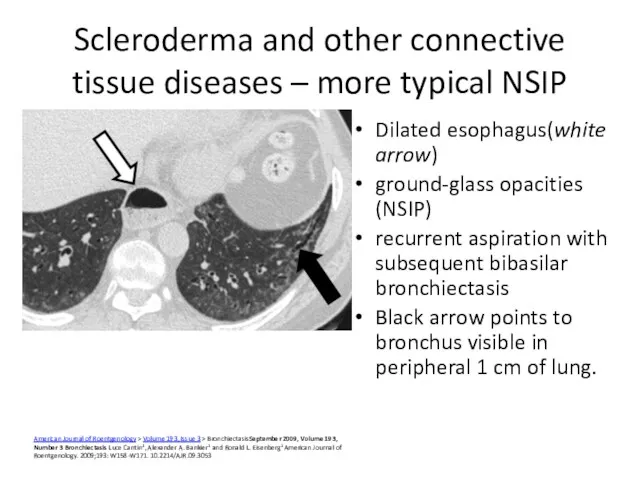
- 41. Scleroderma and other connective tissue diseases – more typical NSIP Dilated esophagus(white arrow) ground-glass opacities (NSIP)
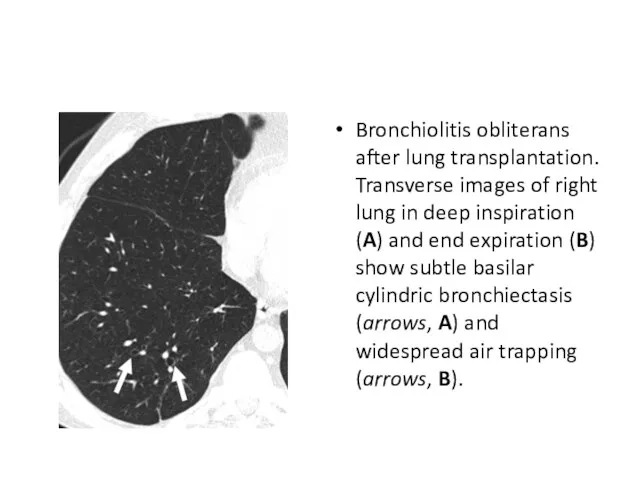
- 42. Bronchiolitis obliterans after lung transplantation. Transverse images of right lung in deep inspiration (A) and end
- 43. Other endotypes ABPA Blood eosinophilia thick sputum with black Bronchial obstruction with wheeze, Asthma in case
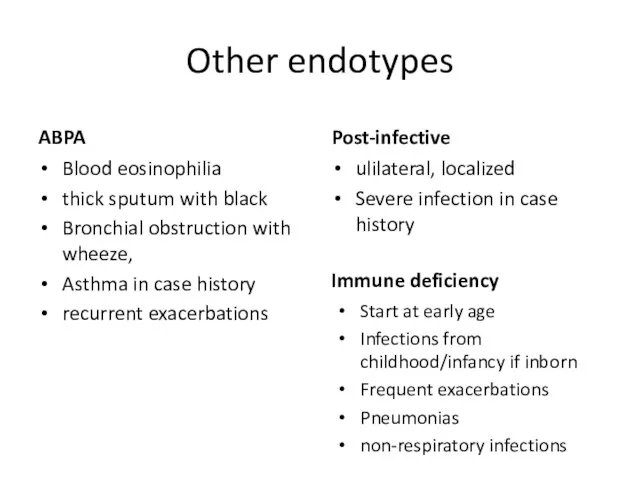
- 44. Allergic bronchopulmonary aspergillosis Asthma Presence of transient pulmonary infiltrates (fleeting shadows) Elevated total serum IgE Peripheral
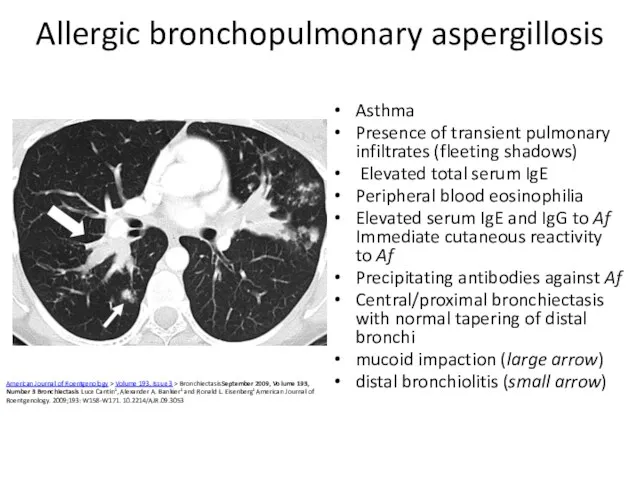
- 45. Same central bronchiectasis and mucoid impaction, so-called finger-in-glove appearance
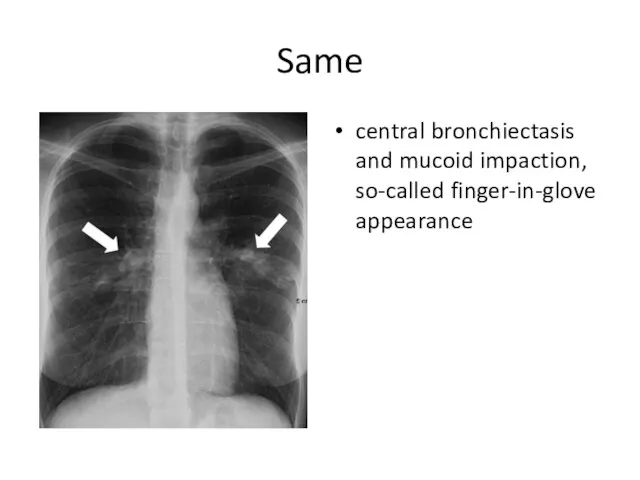
- 46. Other investigations: endotypes assessment Co-morbidities and past medical history to identify relevant and possibly causative disease
- 47. Tests for: cystic fibrosis - early onset, male infertility, malabsorption, pancreatitis Primary Ciliary Dyskinesia if supporting
- 48. Other investigations Spirogram/functional investigation of lungs, oxygen saturation, blood gases Daily protein loss, GFR, urine analysis
- 49. Focal idiopathic in left lower lobe non-TB mycobacteria Perimenopausal females Usually dry bronchoectases Focal bronchiectasis frequently
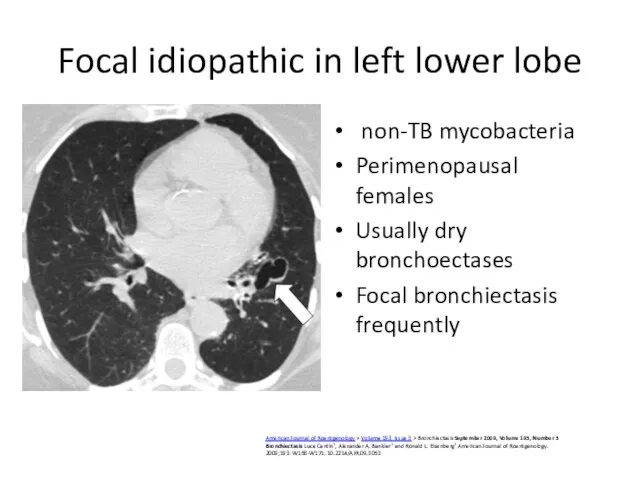
- 50. subtle idiopathic bibasilar cylindric bronchiectasis shows signet-ring sign (arrows). https://www.ajronline.org/doi/10.2214/AJR.09.3053 marked idiopathic left lower bronchiectasis with
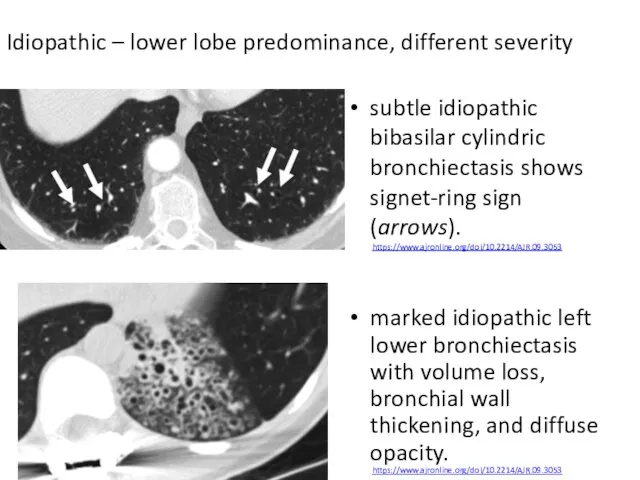
- 51. Mycobacterium avium- intracellulare infection Bronchiectasis (arrows) predominantly involves right middle lobe and lingula. American Journal of
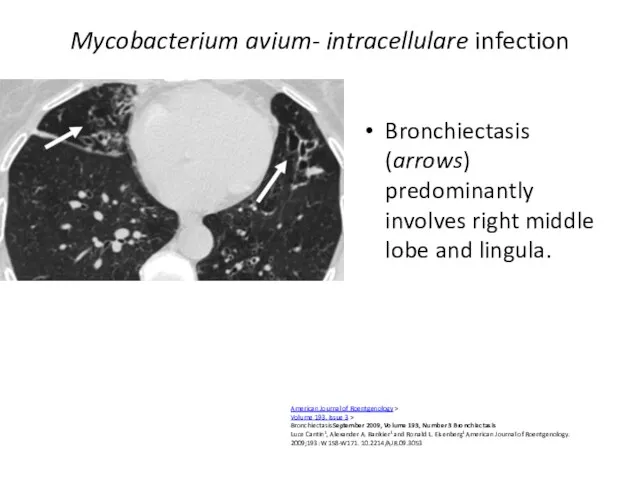
- 52. Obstruction Tumor More gradual onset (1-3 mo) Dyspnea progression from expiratory to inspiratory Dry cough, hemopthisis
- 53. Carcinoid. Endobronchial growth May arise berofe bifurcation of lobar bronchi Serotonin secretion symptoms as following: Flushes
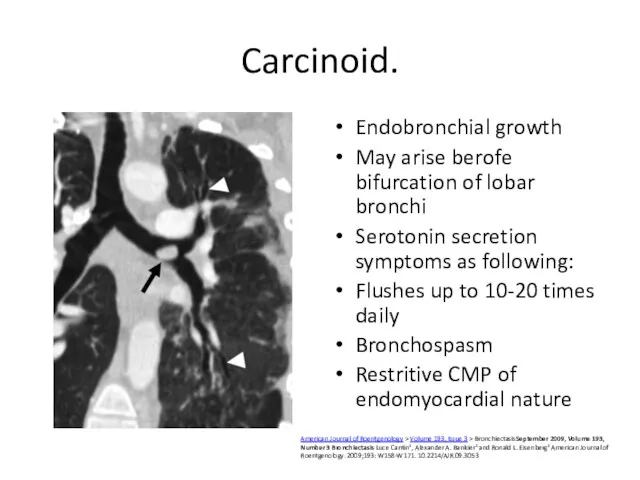
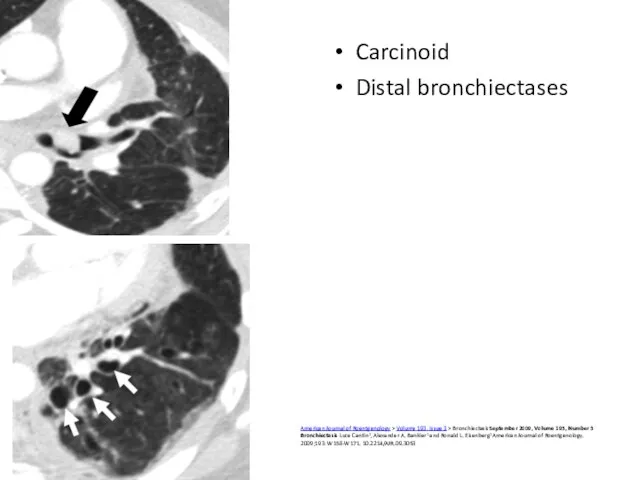
- 54. Carcinoid Distal bronchiectases American Journal of Roentgenology > Volume 193, Issue 3 > BronchiectasisSeptember 2009, Volume
- 55. Tumors: postradiation fibrosis Right paramediastinal fibrotic changes, developed after treatment of lung cancer, are associated with
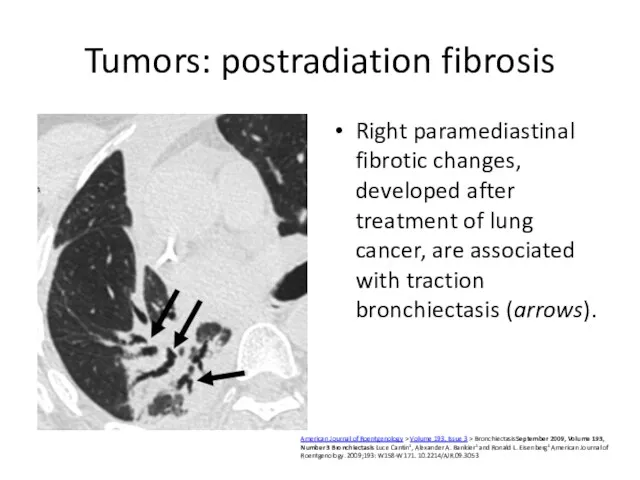
- 56. Broncholithiasis: post TB Calcified left upper lobe endobronchial broncholithiasis Results of lymph node calcification (compression and
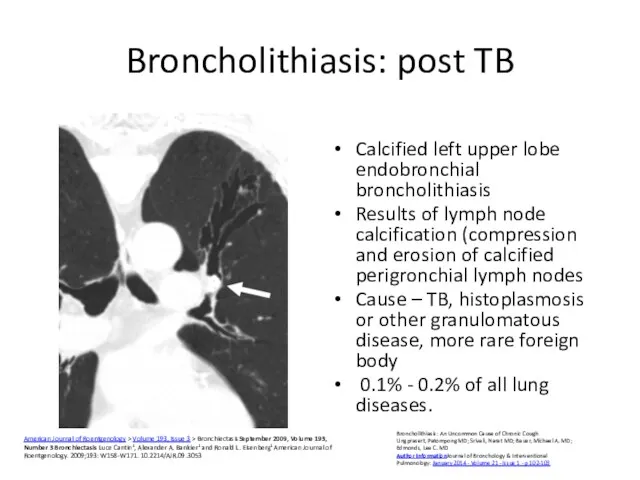
- 57. Congenital abnormalities Congenital stenosis (left mainstem bronchus Bronchial atresia focal bronchiectasis (arrow) distal to bronchial atresia
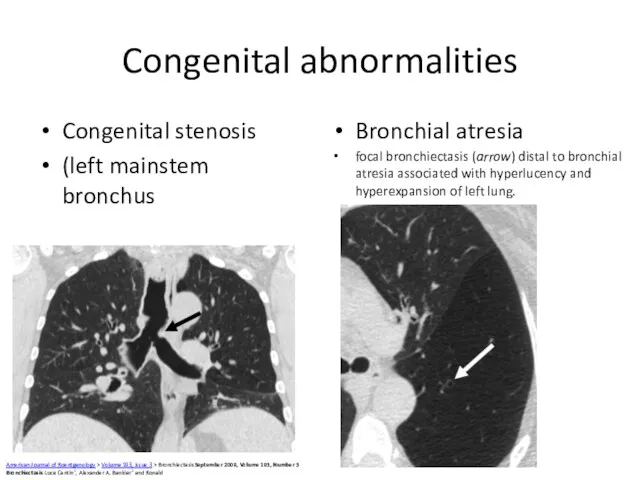
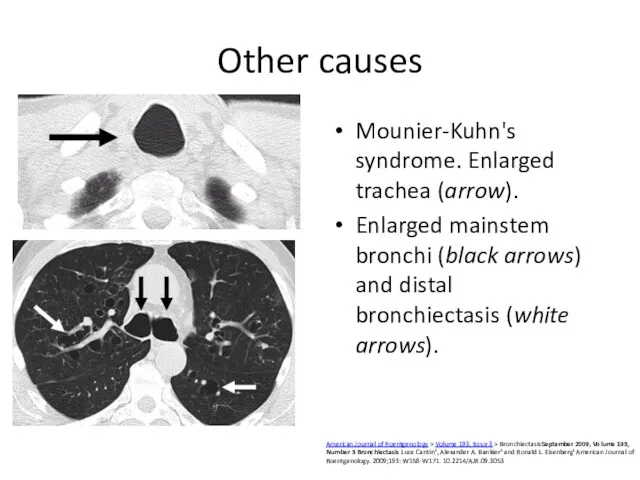
- 58. Other causes Mounier-Kuhn's syndrome. Enlarged trachea (arrow). Enlarged mainstem bronchi (black arrows) and distal bronchiectasis (white
- 59. Williams-Campbell mostly varicose and cystic central bronchiectasis (arrows). American Journal of Roentgenology > Volume 193, Issue
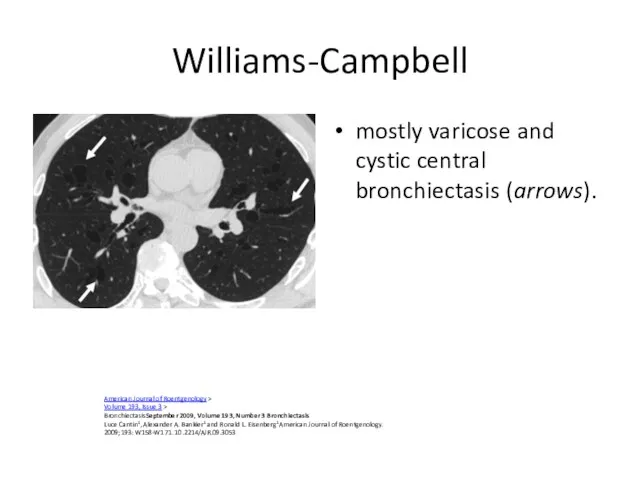
- 60. Advances in bronchiectasis: endotyping, genetics, microbiome, and disease heterogeneityProf Patrick A Flume, MD, Prof James D
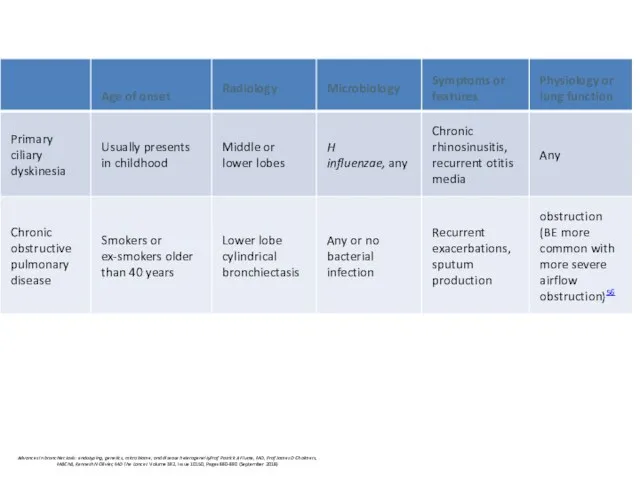
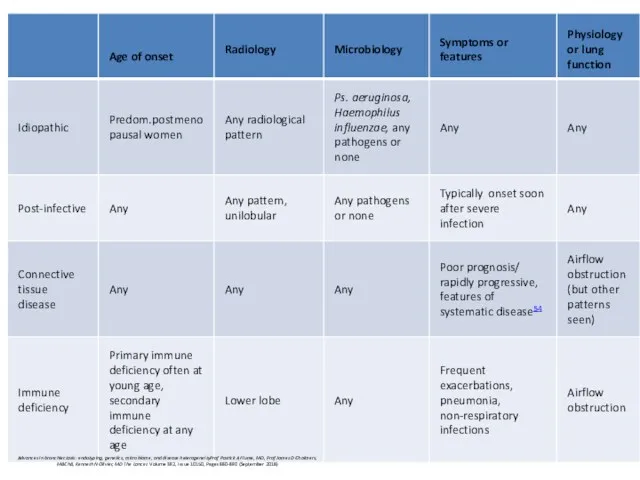
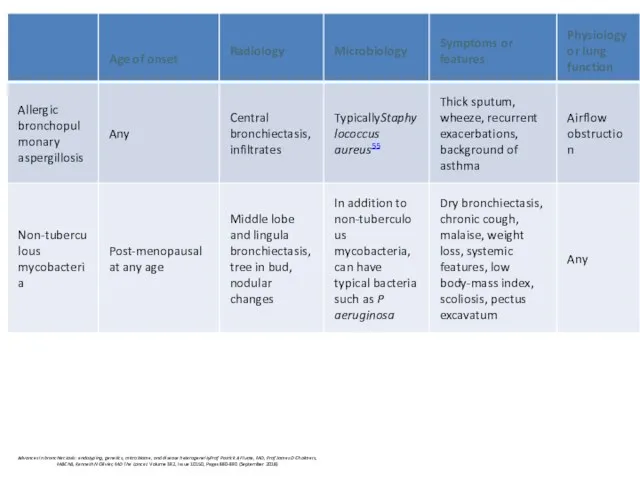
- 61. Advances in bronchiectasis: endotyping, genetics, microbiome, and disease heterogeneityProf Patrick A Flume, MD, Prof James D
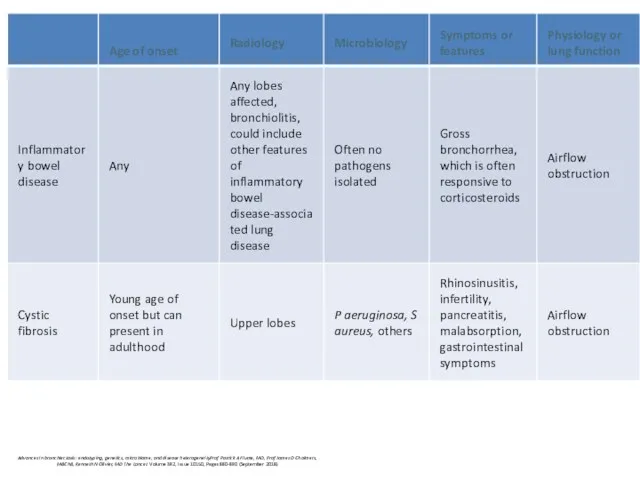
- 62. Cystic fibrosis Cystic fibrosis (CF) is an autosomal recessive disease Loss of function of the cystic
- 63. Pathogenesis: hypothesis chemical shield’ hypothesis: in normal condition airway epithelium produces low salt ( importance of
- 64. Periciliary liquid layer The mucus layer as a liquid reservoir. Upper panel depicts normal geometry of
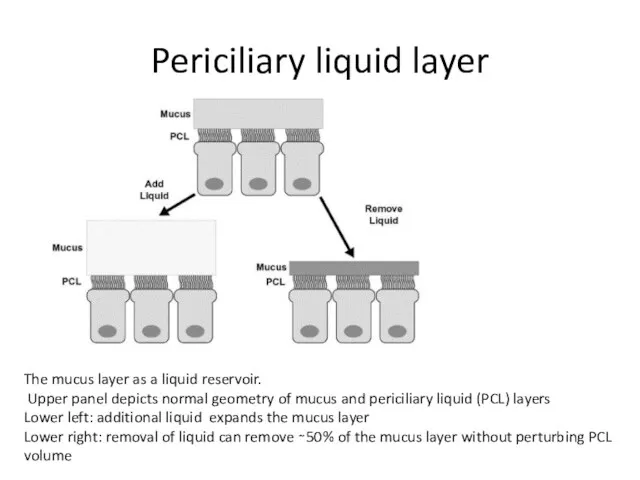
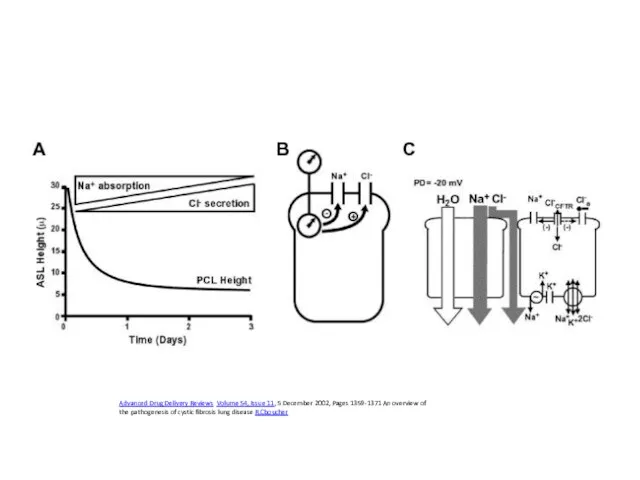
- 65. Advanced Drug Delivery Reviews Volume 54, Issue 11, 5 December 2002, Pages 1359-1371 An overview of
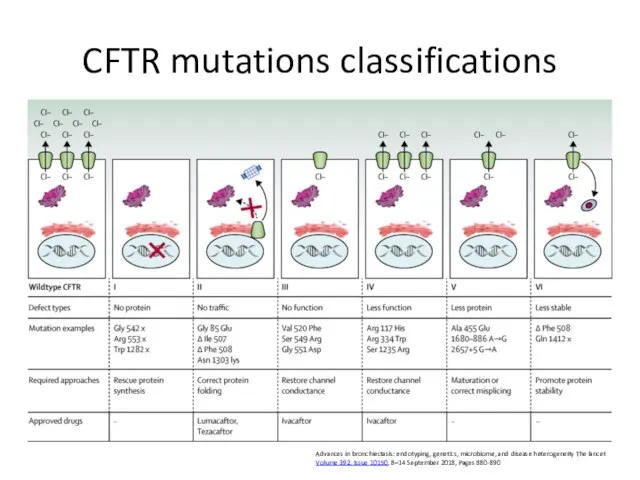
- 66. CFTR mutations classifications Advances in bronchiectasis: endotyping, genetics, microbiome, and disease heterogeneity The lancet Volume 392,
- 67. Median age at diagnosis- 6-8 months; two thirds of patients are diagnosed by 1 year of
- 68. Primary ciliary dyskinesia multiple genes
- 69. Idiopathic bronchiectasis associated with non-tuberculous mycobacteria (NTM) post-menopausal non-smoker females chronic cough No predisposing factors share
- 70. Advances in bronchiectasis: endotyping, genetics, microbiome, and disease heterogeneityProf Patrick A Flume, MD, Prof James D
- 71. Advances in bronchiectasis: endotyping, genetics, microbiome, and disease heterogeneityProf Patrick A Flume, MD, Prof James D
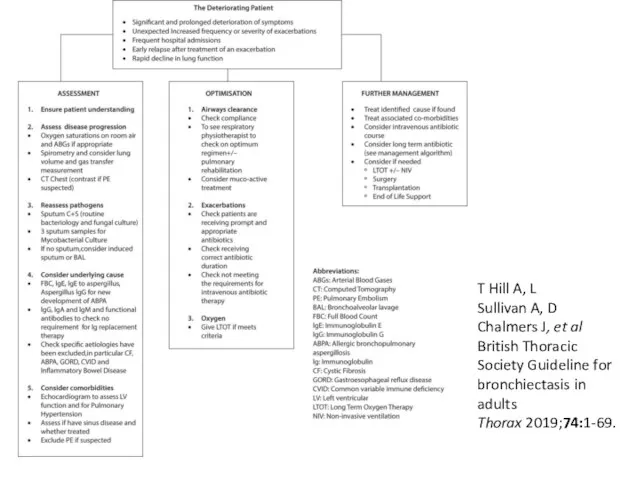
- 72. T Hill A, L Sullivan A, D Chalmers J, et al British Thoracic Society Guideline for
- 73. Initial treatment European Respiratory Society guidelines for the management of adult bronchiectasis Eva Polverino, Pieter C.
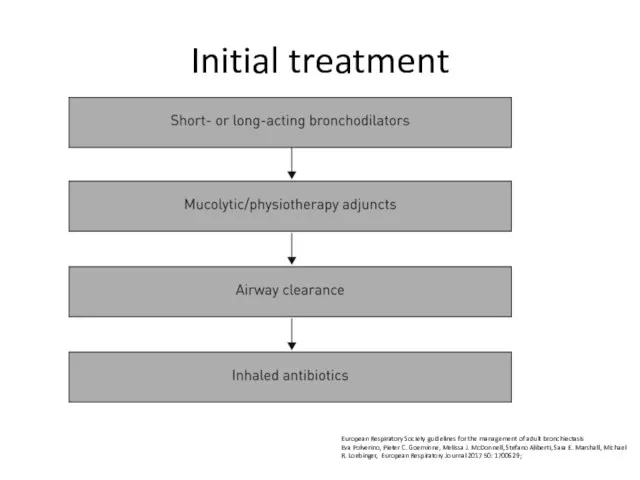
- 74. Offer annual influenza immunisation to all patients with bronchiectasis. (D) Offer polysaccharide pneumococcal vaccination to all
- 75. Physiotherapy – drainage promotion AD: autogenic drainage; ELTGOL: total slow expiration with open glottis and infralateral
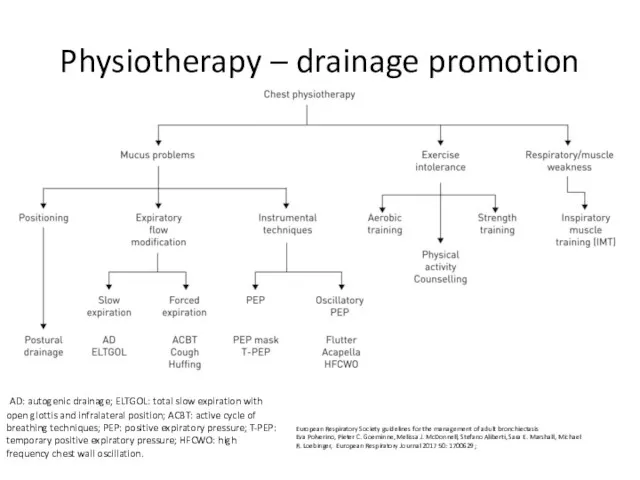
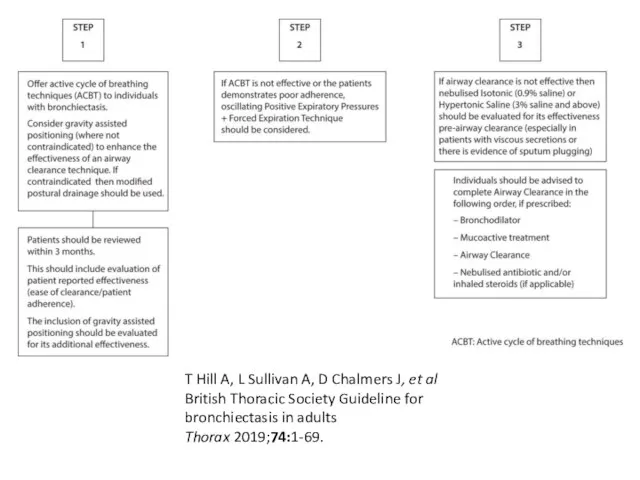
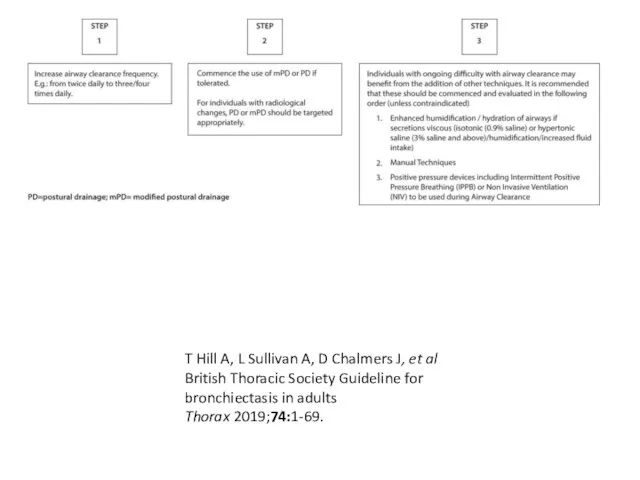
- 76. Airway clearance techniques should be taught by a respiratory physiotherapist. Patients admitted with an exacerbation of
- 77. Consider autogenic drainage, positive expiratory pressure, high frequency chest wall oscillation and intrapulmonary percussive ventilation as
- 78. Airway clearance techniques during an acute exacerbation Manual techniques may be offered to enhance sputum clearance
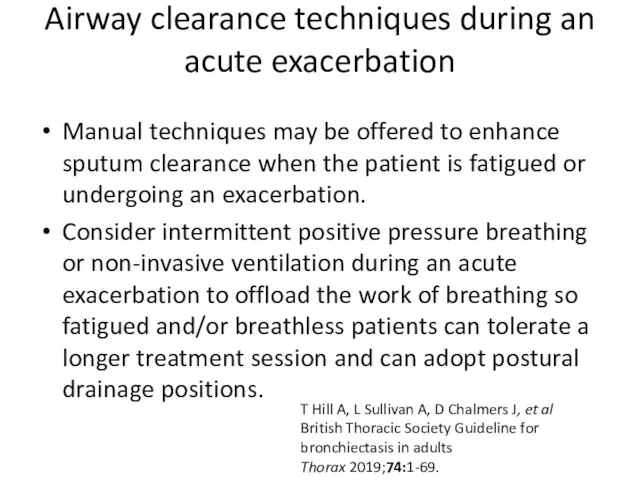
- 79. Mucoactives in bronchiectasis Do not routinely use recombinant human DNase in adults with bronchiectasis. Consider the
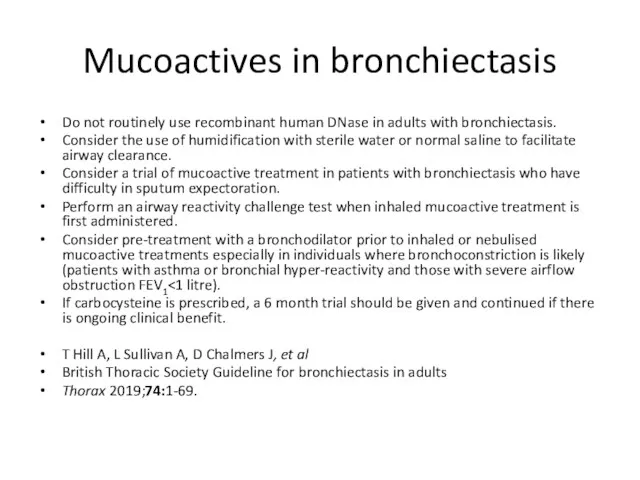
- 80. T Hill A, L Sullivan A, D Chalmers J, et al British Thoracic Society Guideline for
- 81. T Hill A, L Sullivan A, D Chalmers J, et al British Thoracic Society Guideline for
- 82. Inhaled GCS: Do not offer long-term oral corticosteroids for patients with bronchiectasis without other indications (such
- 83. PDE inhibitors, CXCR2 antagonists, statins etc Do not routinely offer phosphodiesterase type 4 (PDE4) inhibitors, methylxanthines
- 84. Antibiotics European Respiratory Society guidelines for the management of adult bronchiectasis Eva Polverino, Pieter C. Goeminne,
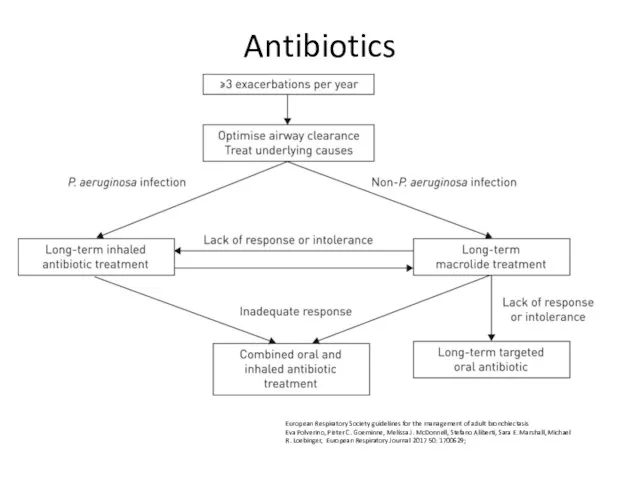
- 85. Consider long term antibiotics in patients with bronchiectasis who experience 3 or more exacerbations per year.
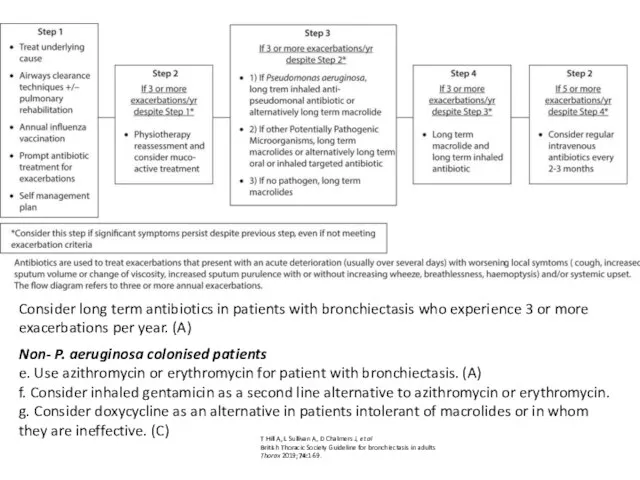
- 86. Safety Prior to starting long term macrolides, for safety reasons: (1) ensure no active NTM infection
- 87. Ps.aeruginosa European Respiratory Society guidelines for the management of adult bronchiectasis Eva Polverino, Pieter C. Goeminne,
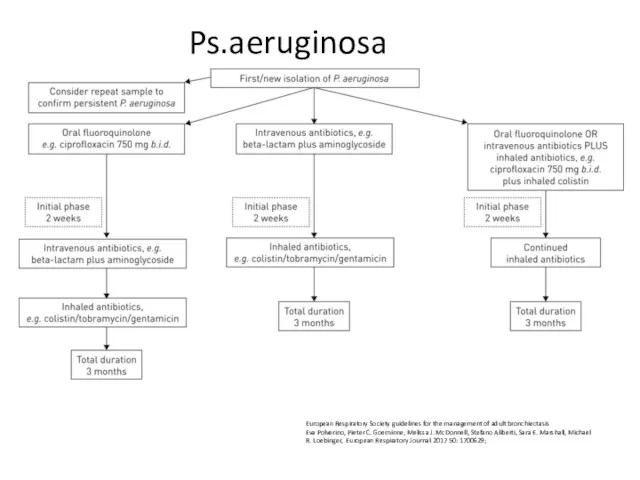
- 88. Offer patients with bronchiectasis associated with clinical deterioration and a new growth of P. aeruginosa (1st
- 89. Offer patients with bronchiectasis associated with clinical deterioration and a new growth of methicillin-resistant S. aureus
- 90. Consider long term oxygen therapy for patients with bronchiectasis and respiratory failure, using the same eligibility
- 91. Consider lung resection in patients with localised disease whose symptoms are not controlled by medical treatment
- 93. Скачать презентацию
 Несеп – жыныс жүйесінің ауытқулары
Несеп – жыныс жүйесінің ауытқулары Адаптация пациентов к зубным протезам. Механизм и динамика адаптации
Адаптация пациентов к зубным протезам. Механизм и динамика адаптации Hypocortisolism Addison's disease
Hypocortisolism Addison's disease Студенттердің тамақтану ерекшеліктері
Студенттердің тамақтану ерекшеліктері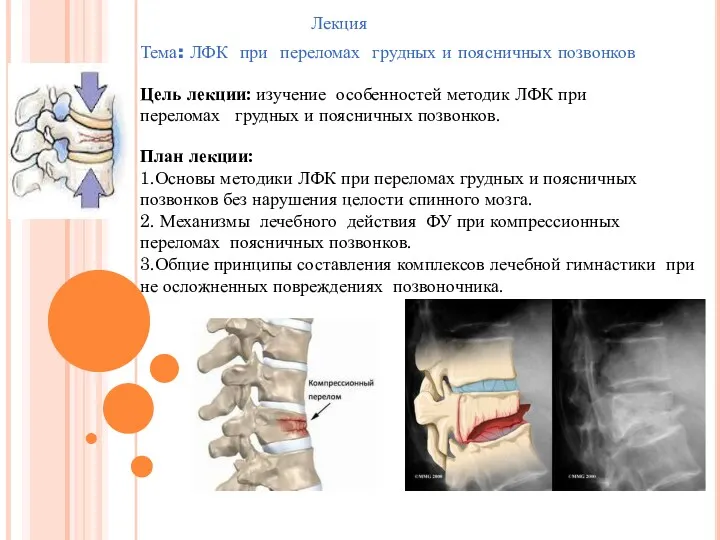 ЛФК при переломах грудных и поясничных позвонков
ЛФК при переломах грудных и поясничных позвонков Менигококковая инфекция
Менигококковая инфекция Дифференциальная диагностика инфаркта миокарда
Дифференциальная диагностика инфаркта миокарда Основные положения гигиенической оценки условий труда в процедуре аттестации рабочих мест
Основные положения гигиенической оценки условий труда в процедуре аттестации рабочих мест Нейроинфекция у детей
Нейроинфекция у детей Тірі адамға сараптама жасау
Тірі адамға сараптама жасау An Introduction To The Health Effects of Arsenic (As)
An Introduction To The Health Effects of Arsenic (As) Консультация учителя-дефектолога: Основные направления коррекционной работы по исправлению недостатков звукопроизношения
Консультация учителя-дефектолога: Основные направления коррекционной работы по исправлению недостатков звукопроизношения Мукополисахаридоз
Мукополисахаридоз Сальмонеллез, колибактериоз, диплококкоз сельскохозяйственных животных
Сальмонеллез, колибактериоз, диплококкоз сельскохозяйственных животных Технология мягких лекарственных форм
Технология мягких лекарственных форм Эхинококкоз человека
Эхинококкоз человека Ультрадыбыстың медицинада қолданылуы
Ультрадыбыстың медицинада қолданылуы Наркомании и токсикомании
Наркомании и токсикомании Воспаление. Причинные факторы воспаления (флогогены)
Воспаление. Причинные факторы воспаления (флогогены) Удаление дивертикула Меккеля. Болезнь Гиршпрунга
Удаление дивертикула Меккеля. Болезнь Гиршпрунга Методы исследования больных с заболеваниями органов дыхания. Расспрос больного
Методы исследования больных с заболеваниями органов дыхания. Расспрос больного Септический шок и септицемия
Септический шок и септицемия Гипотермия и Гипертермия
Гипотермия и Гипертермия Портфели влияют на нашу осанку
Портфели влияют на нашу осанку Системы нижней полой вены и воротной вены. Ситуационные задачи
Системы нижней полой вены и воротной вены. Ситуационные задачи Менструальный цикл
Менструальный цикл Преэклампсия. Гестоз - осложнение беременности
Преэклампсия. Гестоз - осложнение беременности Обезболивание при стоматологическом вмешательстве у детей. Виды обезболивания. Современные анестетики, их свойства
Обезболивание при стоматологическом вмешательстве у детей. Виды обезболивания. Современные анестетики, их свойства