Содержание
- 2. Chronic Lymphocytic Leukemia, Small Lymphocytic Lymphoma and Monoclonal B-cell Lymphocytosis: Concept • Disorders of “mature” CD5+
- 3. Monoclonal B lymphocytosis SmIg weak, CD5+, CD19+, CD23+, CD20 weak Spleen/liver Enlarged lymph nodes NO→MBL YES→SLL
- 4. CLL Most frequent leukemia in adults – 30% of all adult leukemias Incidence in western world:
- 5. Aetiology The cause of CLL is unknown There is increased incidence in farmers, rubber manufacturing workers,
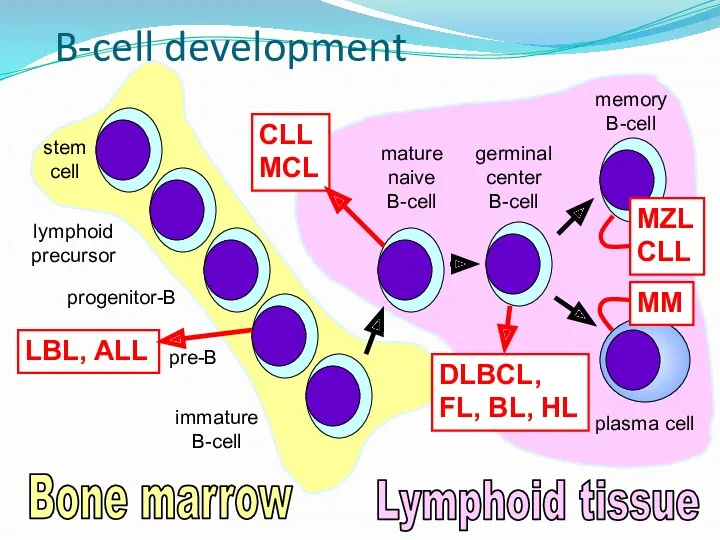
- 6. B-cell development
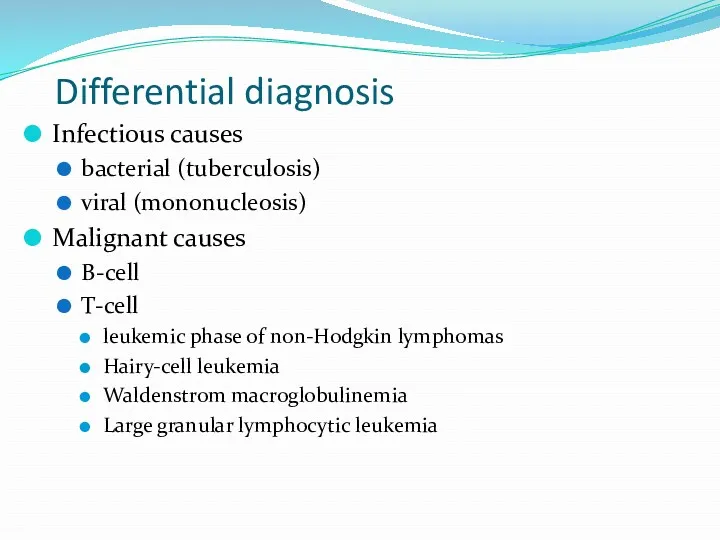
- 7. Differential diagnosis Infectious causes bacterial (tuberculosis) viral (mononucleosis) Malignant causes B-cell T-cell leukemic phase of non-Hodgkin
- 8. Clinical findings (1) Approximately 40% of CLL patients are asymptomatic at diagnosis In symptomatic cases the
- 9. Clinical findings (2) Most symptomatic patients have enlarged lymph nodes (more commonly cervical and supraclavicular) and
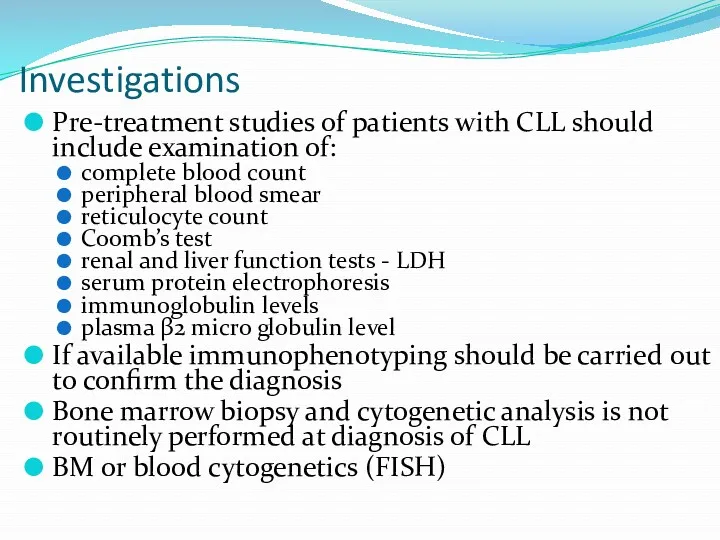
- 11. Investigations Pre-treatment studies of patients with CLL should include examination of: complete blood count peripheral blood
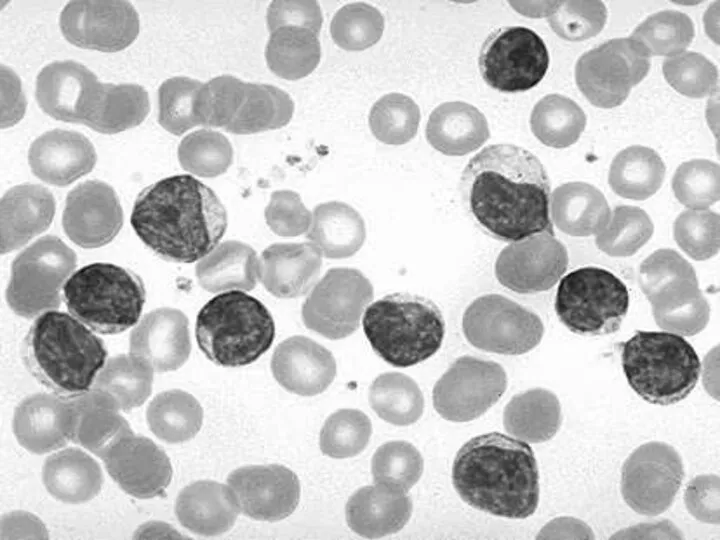
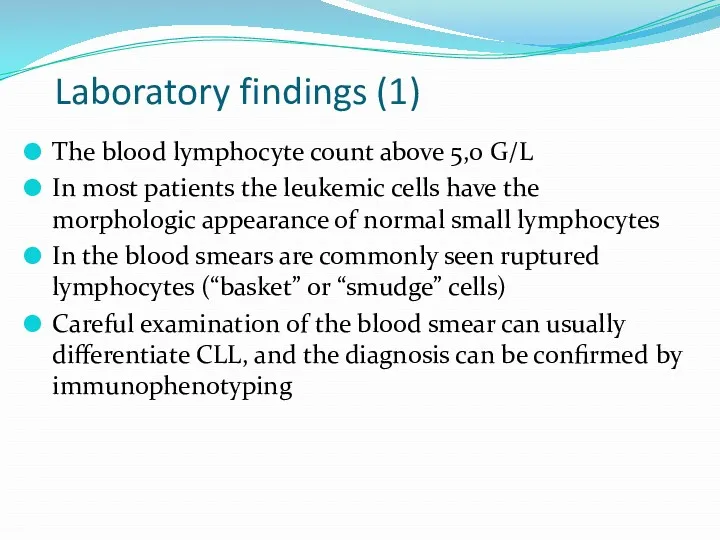
- 12. Laboratory findings (1) The blood lymphocyte count above 5,0 G/L In most patients the leukemic cells
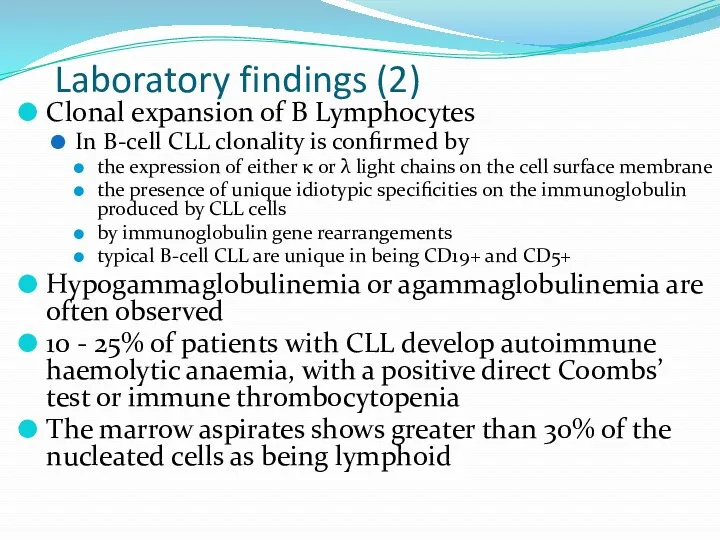
- 13. Laboratory findings (2) Clonal expansion of B Lymphocytes In B-cell CLL clonality is confirmed by the
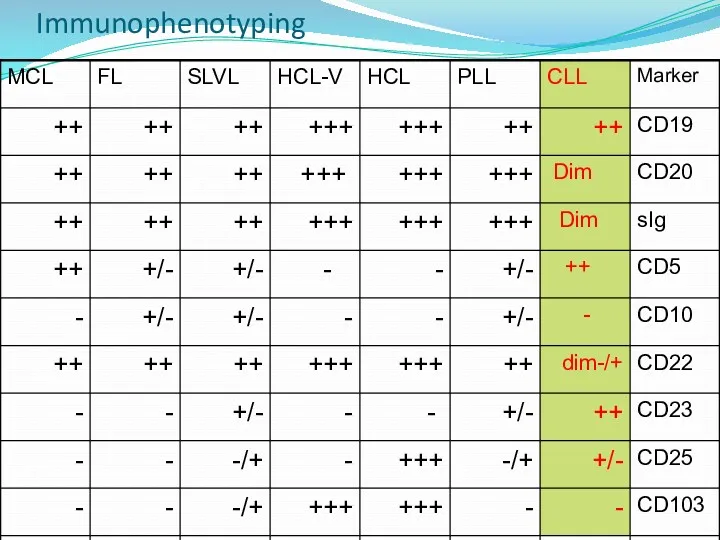
- 14. Immunophenotyping
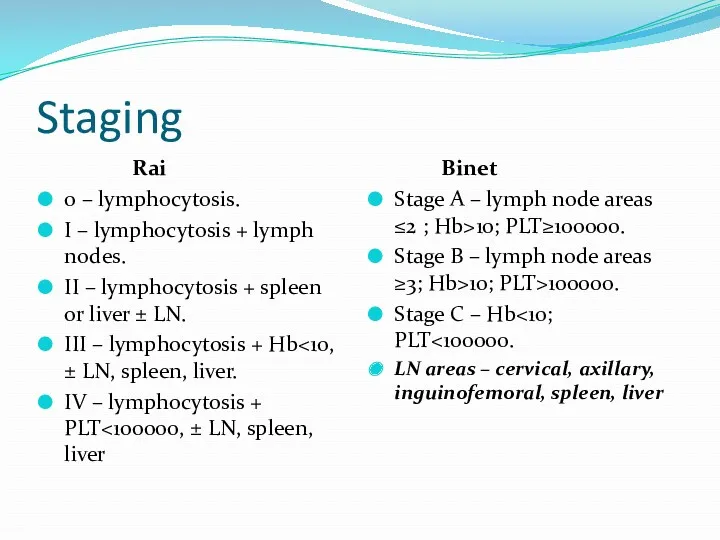
- 15. Staging Rai 0 – lymphocytosis. I – lymphocytosis + lymph nodes. II – lymphocytosis + spleen
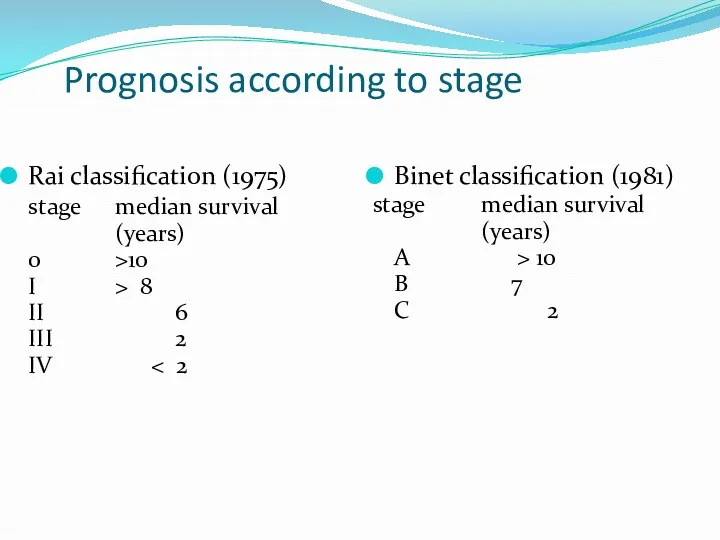
- 16. Prognosis according to stage Rai classification (1975) stage median survival (years) 0 >10 I > 8
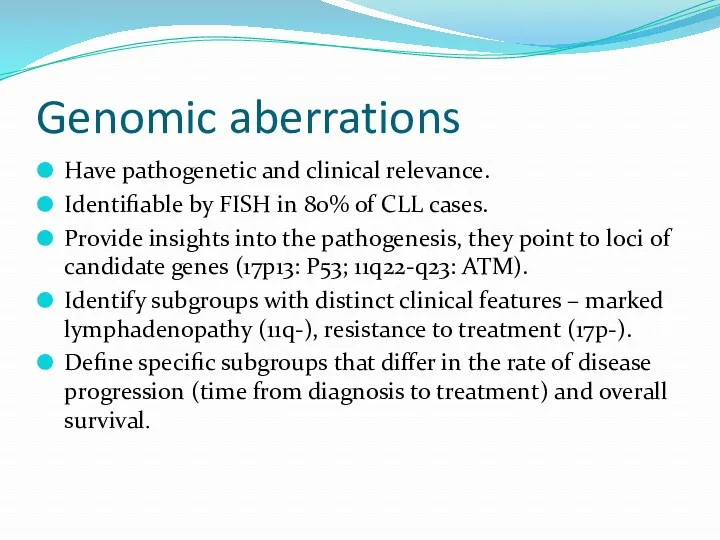
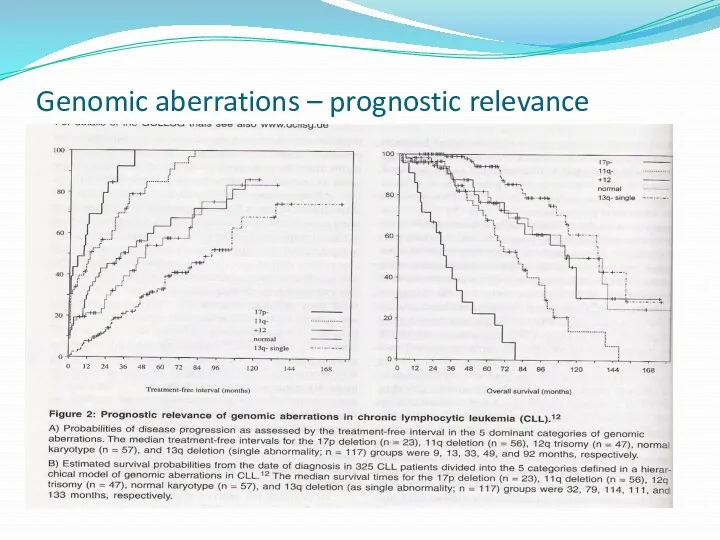
- 17. Genomic aberrations Have pathogenetic and clinical relevance. Identifiable by FISH in 80% of CLL cases. Provide
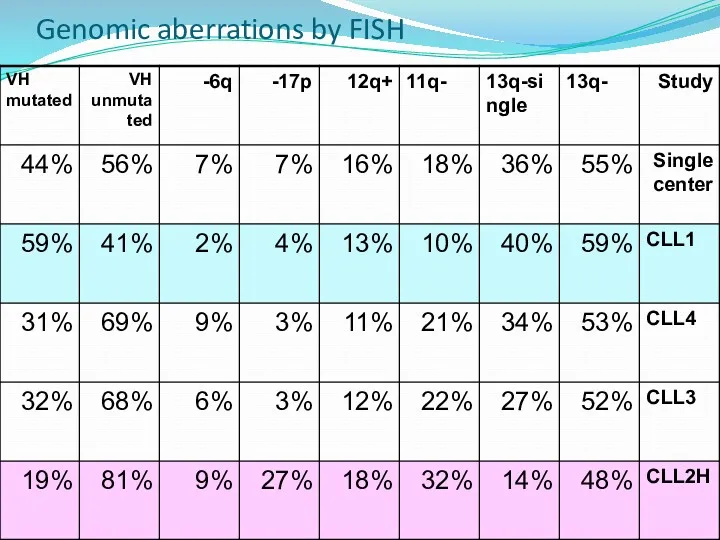
- 18. Genomic aberrations by FISH
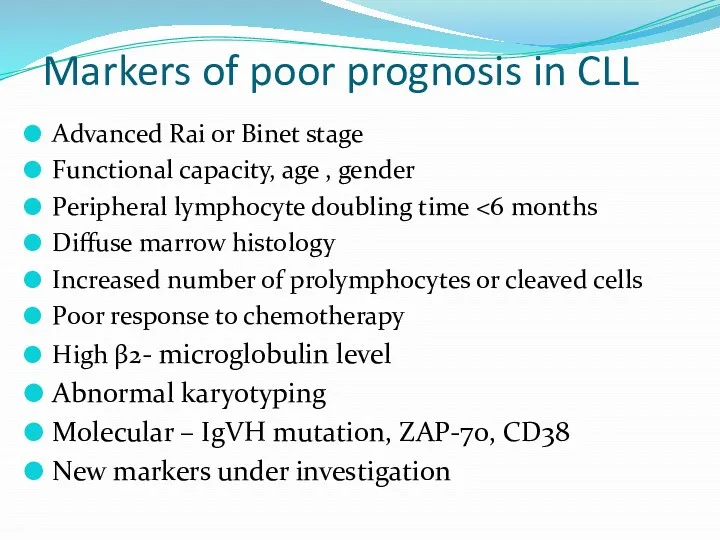
- 19. Markers of poor prognosis in CLL Advanced Rai or Binet stage Functional capacity, age , gender
- 20. Risk Stratification Diagnosis TP53 analysis Age, gender, function, stage, comorbidities TP53 intact IgVH mutation FISH Molecular
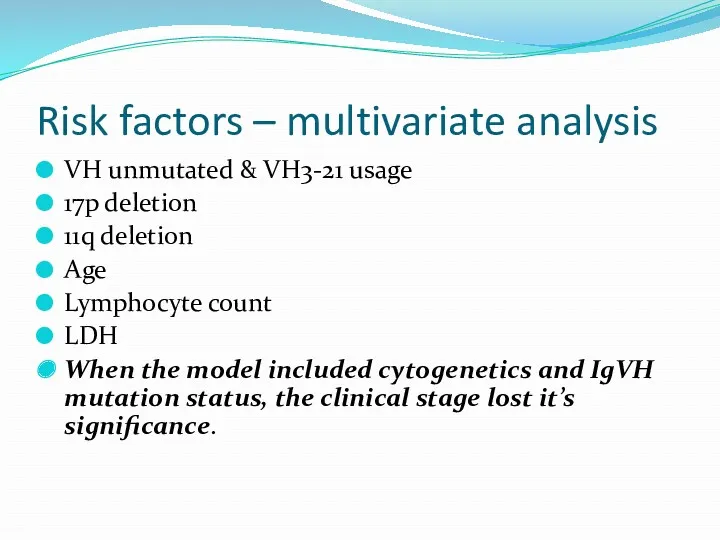
- 21. Risk factors – multivariate analysis VH unmutated & VH3-21 usage 17p deletion 11q deletion Age Lymphocyte
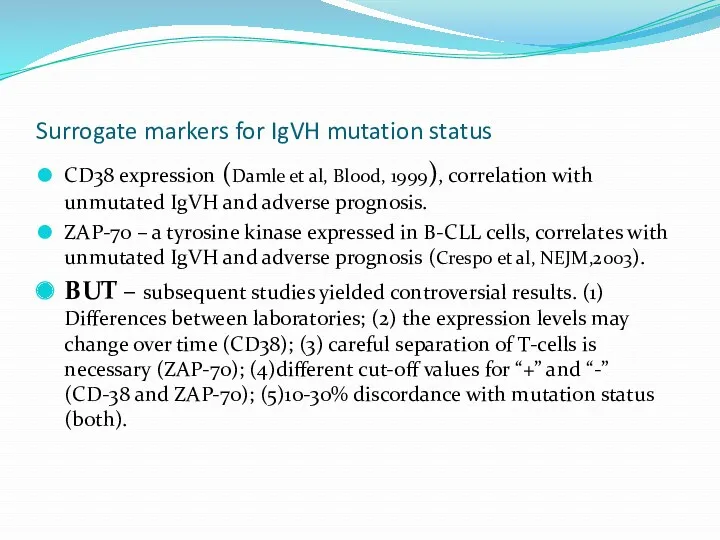
- 22. Surrogate markers for IgVH mutation status CD38 expression (Damle et al, Blood, 1999), correlation with unmutated
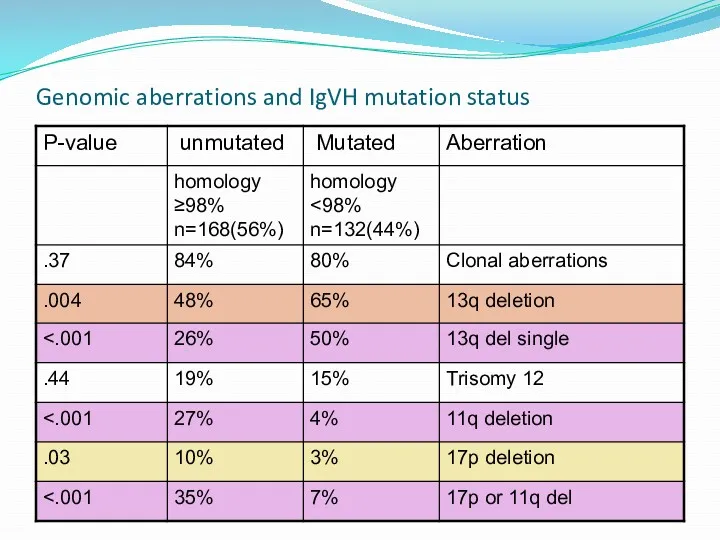
- 23. Genomic aberrations and IgVH mutation status
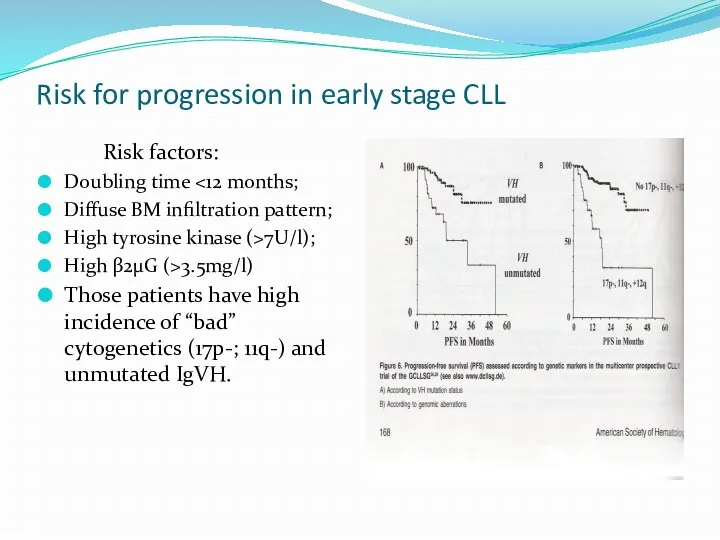
- 24. Risk for progression in early stage CLL Risk factors: Doubling time Diffuse BM infiltration pattern; High
- 25. Genomic aberrations – prognostic relevance
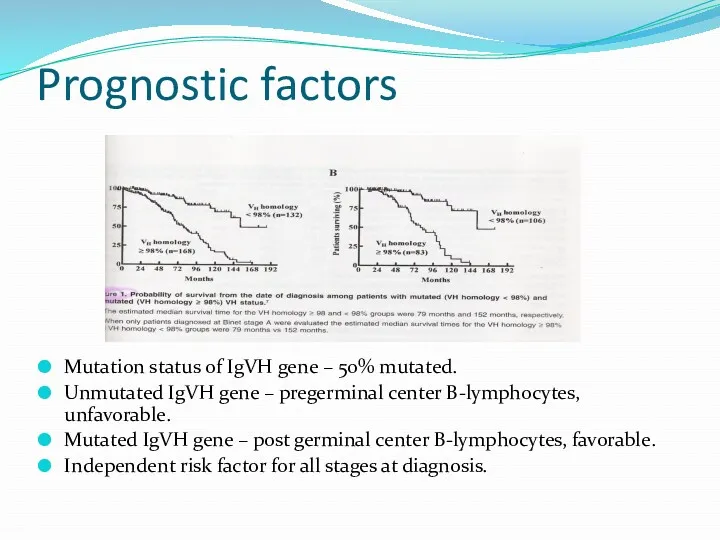
- 26. Prognostic factors Mutation status of IgVH gene – 50% mutated. Unmutated IgVH gene – pregerminal center
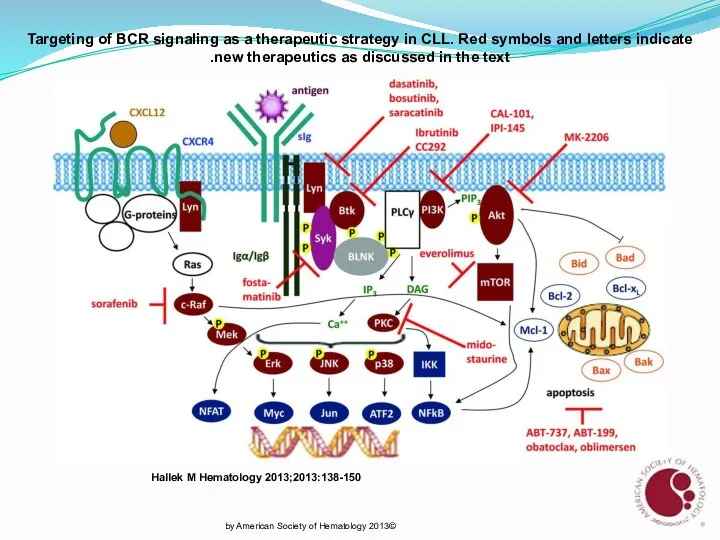
- 27. Targeting of BCR signaling as a therapeutic strategy in CLL. Red symbols and letters indicate new
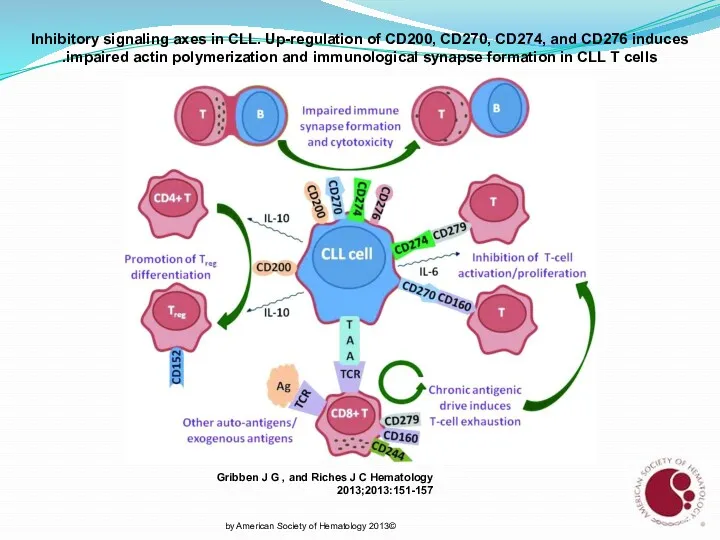
- 28. Inhibitory signaling axes in CLL. Up-regulation of CD200, CD270, CD274, and CD276 induces impaired actin polymerization
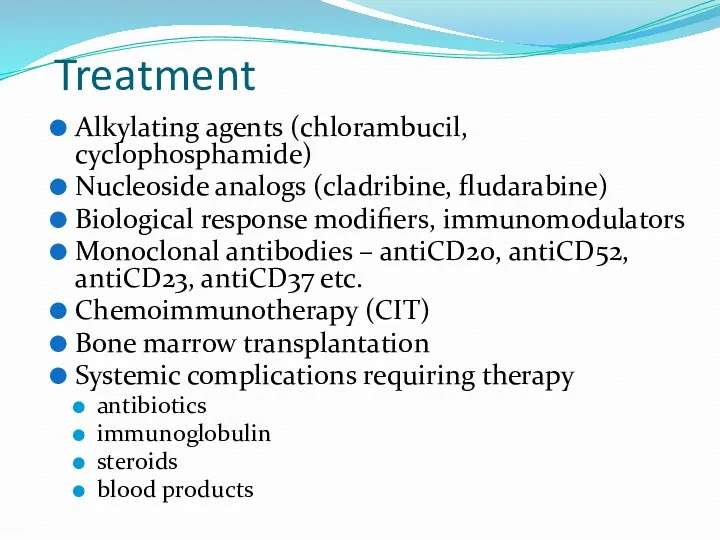
- 29. Treatment Alkylating agents (chlorambucil, cyclophosphamide) Nucleoside analogs (cladribine, fludarabine) Biological response modifiers, immunomodulators Monoclonal antibodies –
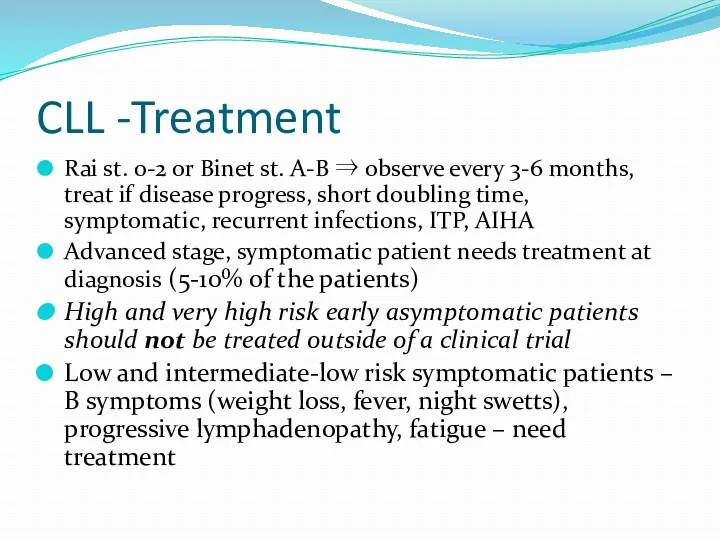
- 30. CLL -Treatment Rai st. 0-2 or Binet st. A-B ⇒ observe every 3-6 months, treat if
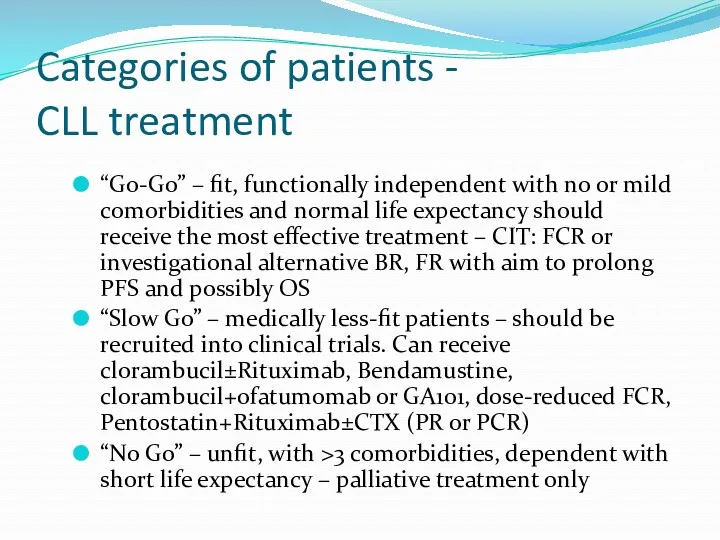
- 31. Categories of patients - CLL treatment “Go-Go” – fit, functionally independent with no or mild comorbidities
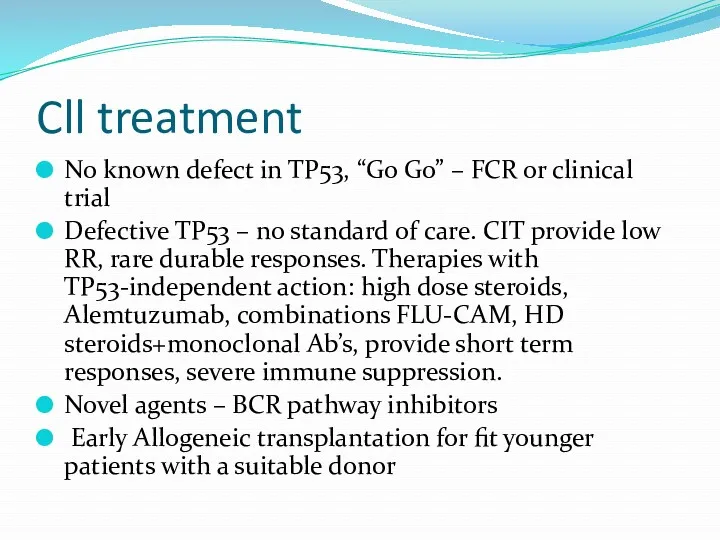
- 32. Cll treatment No known defect in TP53, “Go Go” – FCR or clinical trial Defective TP53
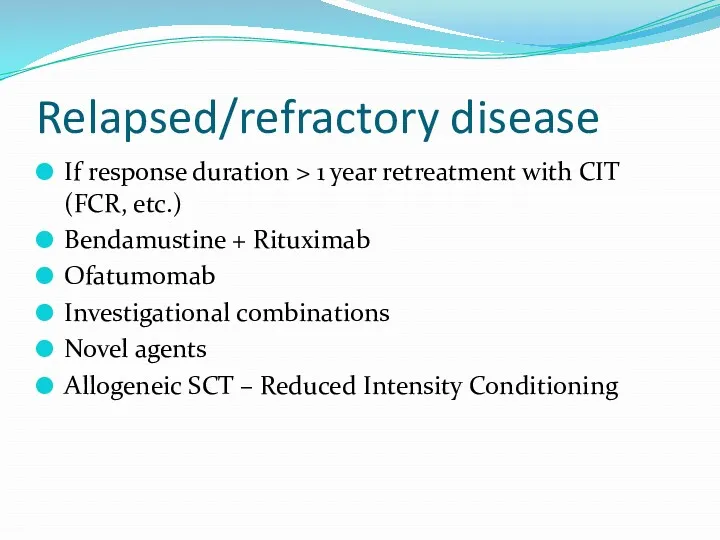
- 33. Relapsed/refractory disease If response duration > 1 year retreatment with CIT (FCR, etc.) Bendamustine + Rituximab
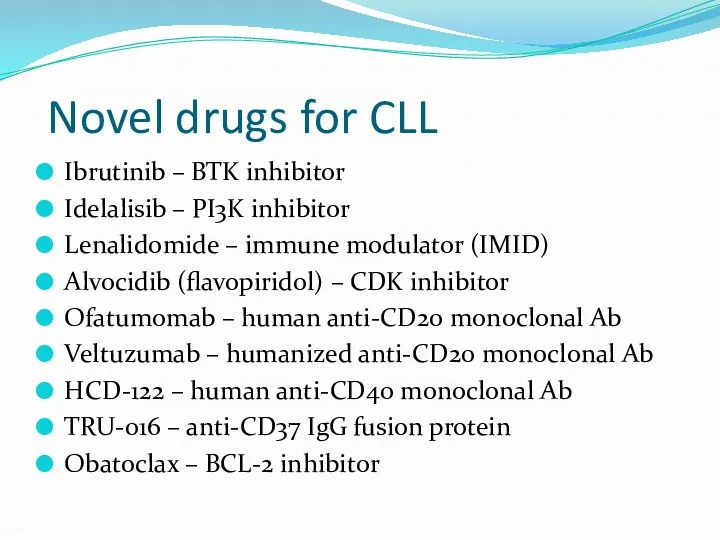
- 34. Novel drugs for CLL Ibrutinib – BTK inhibitor Idelalisib – PI3K inhibitor Lenalidomide – immune modulator
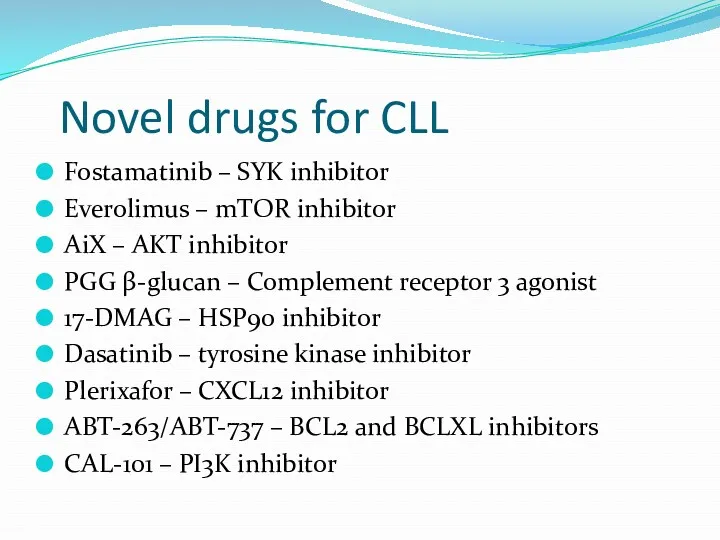
- 35. Novel drugs for CLL Fostamatinib – SYK inhibitor Everolimus – mTOR inhibitor AiX – AKT inhibitor
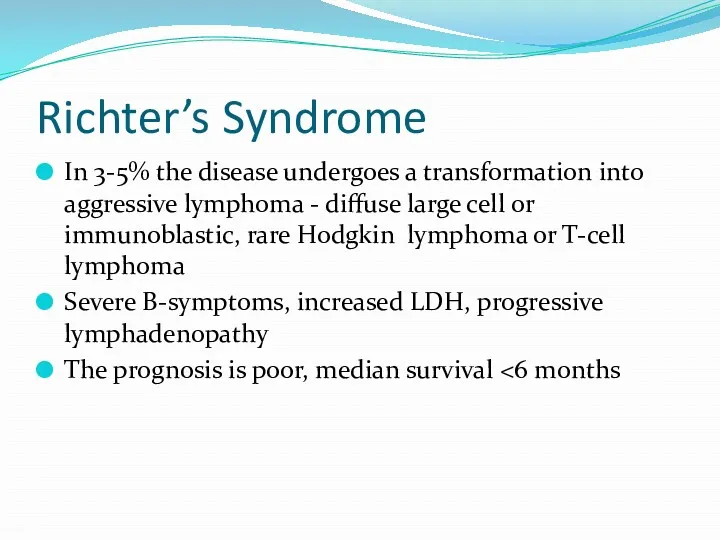
- 36. Richter’s Syndrome In 3-5% the disease undergoes a transformation into aggressive lymphoma - diffuse large cell
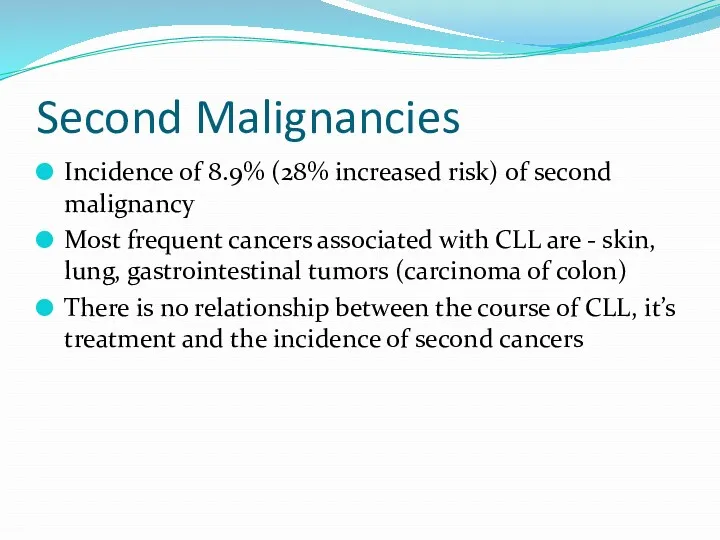
- 37. Second Malignancies Incidence of 8.9% (28% increased risk) of second malignancy Most frequent cancers associated with
- 39. Скачать презентацию

 Хронический гепатит
Хронический гепатит Хребетно-спінальна травма
Хребетно-спінальна травма Психология сложного дефекта
Психология сложного дефекта Термiнальнi та критичнi стани. Клінічна смерть
Термiнальнi та критичнi стани. Клінічна смерть Ортодонтиялық емдеудің негізгі принциптер
Ортодонтиялық емдеудің негізгі принциптер Кесарево сечение в современном акушерстве
Кесарево сечение в современном акушерстве Холецистэктомия. Травма печени
Холецистэктомия. Травма печени Анатомия и физиология, как науки
Анатомия и физиология, как науки Эпидемиологическая ситуация по ВИЧ-инфекции в мире и России. Кодировка направлений на исследование крови на ВИЧ-инфекцию
Эпидемиологическая ситуация по ВИЧ-инфекции в мире и России. Кодировка направлений на исследование крови на ВИЧ-инфекцию Вторичный туберкулез. Диссеминированный туберкулез легких
Вторичный туберкулез. Диссеминированный туберкулез легких Инфильтративный, кавернозный и фиброзно-кавернозный туберкулез. Туберкулома. Казеозная пневмония
Инфильтративный, кавернозный и фиброзно-кавернозный туберкулез. Туберкулома. Казеозная пневмония Первичная реанимация новорожденных
Первичная реанимация новорожденных Чувствительная кожа
Чувствительная кожа Медицинская реабилитация при повреждениях верхних конечностей
Медицинская реабилитация при повреждениях верхних конечностей Бинокулярное зрение. Косоглазие
Бинокулярное зрение. Косоглазие Интервенционные лучевые методы исследования и коррекции плода
Интервенционные лучевые методы исследования и коррекции плода Важная роль воды. значение воды для животного мира, для человека, в промышленности
Важная роль воды. значение воды для животного мира, для человека, в промышленности Лечение переломов верхней челюсти
Лечение переломов верхней челюсти Транквилизаторы (анксиолитики)
Транквилизаторы (анксиолитики) Методы выявления возбудителей туберкулеза и микобактериоза
Методы выявления возбудителей туберкулеза и микобактериоза Хронический пиелонефрит
Хронический пиелонефрит Еріту. Сұйықтықтарды араластыру. Қатты заттарды және сұйықтықтарды бөліп алу
Еріту. Сұйықтықтарды араластыру. Қатты заттарды және сұйықтықтарды бөліп алу Анатомо-физиологические особенности детей младшего школьного возраста
Анатомо-физиологические особенности детей младшего школьного возраста Алынбайтын протездер
Алынбайтын протездер Морфология органов периферической эндокринной системы
Морфология органов периферической эндокринной системы Сосудистая хирургия
Сосудистая хирургия Печень. Поджелудочная железа. Гистология
Печень. Поджелудочная железа. Гистология Лапаротомия надлобковым разрезом. Кесарево сечение в нижнем сегменте матки
Лапаротомия надлобковым разрезом. Кесарево сечение в нижнем сегменте матки