Содержание
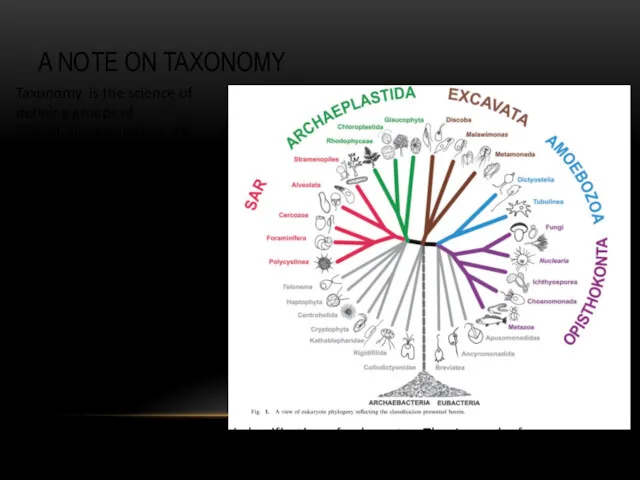
- 2. A NOTE ON TAXONOMY Adl et al. 2012 The revised classification of eukaryotes. The Journal of
- 3. PROTIST VS. PROTOZOA Kingdom Protista (single-celled eukaryotic organisms) Protozoa (heterotrophic protists) was considered as phylum within
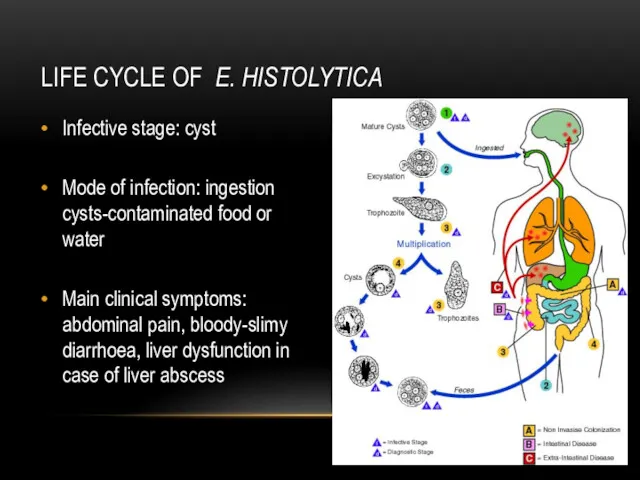
- 4. IMPORTANT TERMS Trophozoite – actively motile feeding stage. Cyst – resistant, infective stage.
- 5. MORPHOLOGY-BASED TAXONOMY Depending on the locomotion mode protozoa divided into four major groups: Phylum Flagellates (move
- 6. MORPHOLOGY-BASED TAXONOMY Depending on the locomotion mode protozoa divided into four major groups: Phylum Amoebae (by
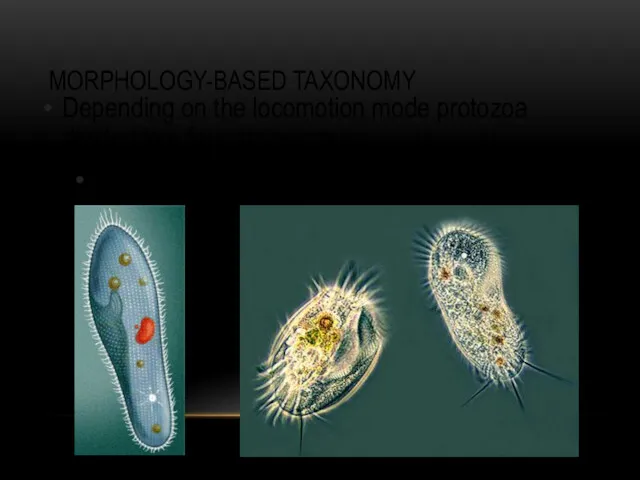
- 7. MORPHOLOGY-BASED TAXONOMY Depending on the locomotion mode protozoa divided into four major groups: Phylum Ciliates (by
- 8. MORPHOLOGY-BASED TAXONOMY Depending on the locomotion mode protozoa divided into four major groups: Phylum Sporozoa (lacking
- 9. PARASITIC AMOEBAE Six species of amoebae are common in humans in most parts of the world
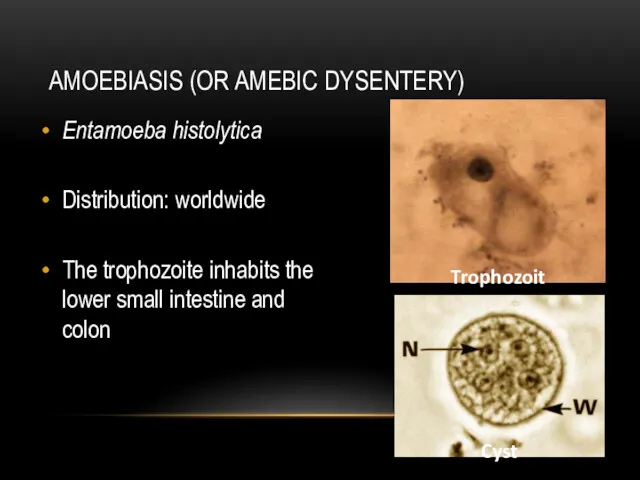
- 10. AMOEBIASIS (OR AMEBIC DYSENTERY) Entamoeba histolytica Distribution: worldwide The trophozoite inhabits the lower small intestine and
- 11. LIFE CYCLE OF E. HISTOLYTICA Infective stage: cyst Mode of infection: ingestion cysts-contaminated food or water
- 12. DIAGNOSIS AND PREVENTION OF AMOEBIASIS Diagnosis: Microscopical determination of cysts in fecal samples, serology. Prevention: Avoidance
- 13. NON-INTESTINE PARASITIC AMOEBAE … human infection is not an obligate part of their life cycle. Naegleria
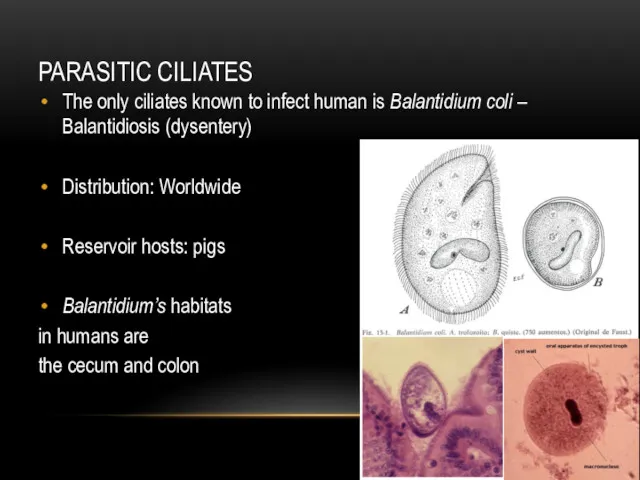
- 14. PARASITIC CILIATES The only ciliates known to infect human is Balantidium coli – Balantidiosis (dysentery) Distribution:
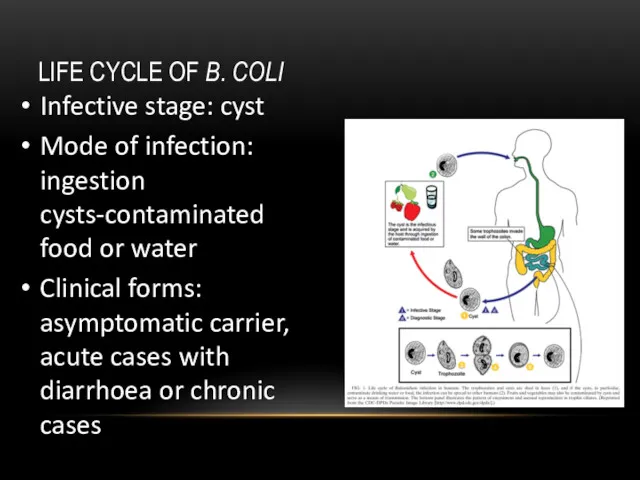
- 15. LIFE CYCLE OF B. COLI Infective stage: cyst Mode of infection: ingestion cysts-contaminated food or water
- 16. PARASITIC FLAGELLATES Depending on the infected organs, parasitic flagellates might be classified in two broad groups.
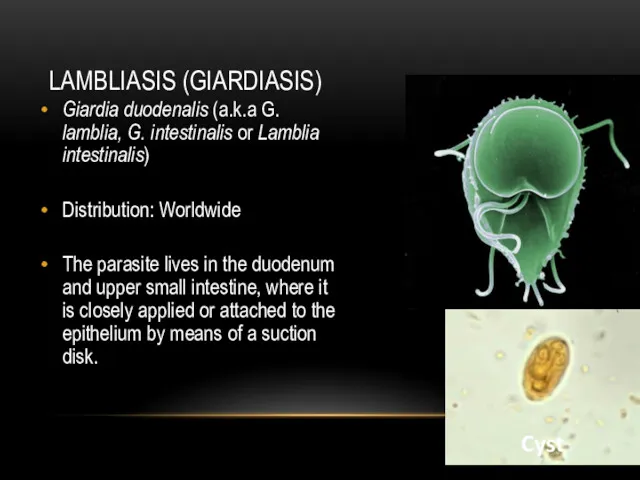
- 17. LAMBLIASIS (GIARDIASIS) Giardia duodenalis (a.k.a G. lamblia, G. intestinalis or Lamblia intestinalis) Distribution: Worldwide The parasite
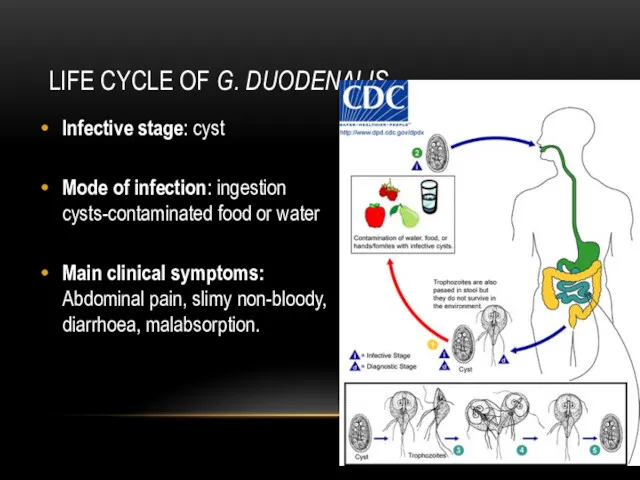
- 18. LIFE CYCLE OF G. DUODENALIS Infective stage: cyst Mode of infection: ingestion cysts-contaminated food or water
- 19. DIAGNOSIS AND PREVENTION OF LAMBLIASIS Diagnosis: Microscopic determination of trophozoites and cysts in faecal samples. Prevention:
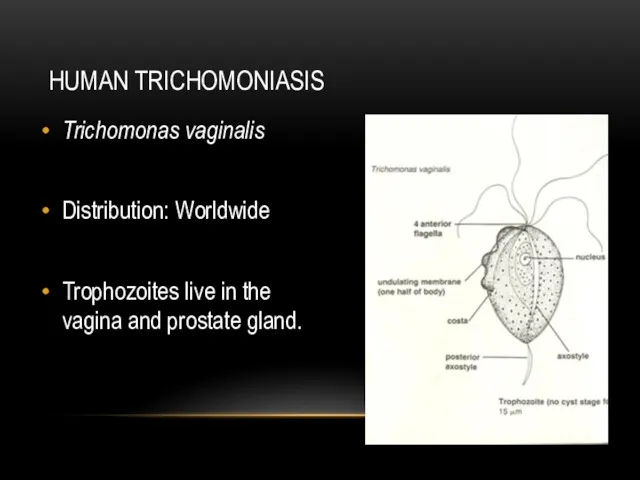
- 20. HUMAN TRICHOMONIASIS Trichomonas vaginalis Distribution: Worldwide Trophozoites live in the vagina and prostate gland.
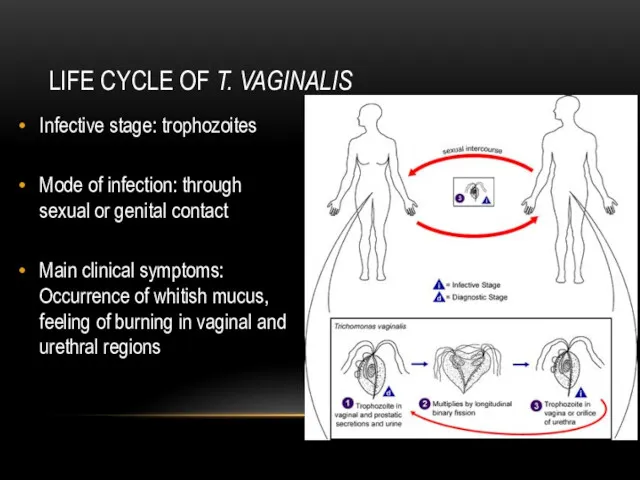
- 21. LIFE CYCLE OF T. VAGINALIS Infective stage: trophozoites Mode of infection: through sexual or genital contact
- 22. DIAGNOSIS AND PREVENTION OF TRICHOMONIASIS Diagnosis: Microscopic detection of trophozoites in mucus samples. Prophylaxis: Avoid unprotected
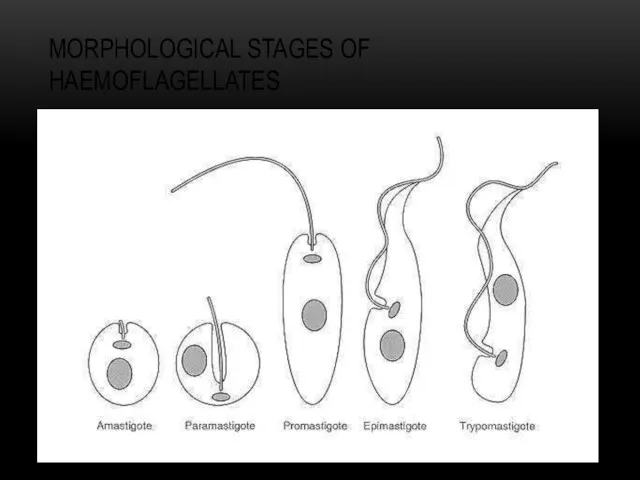
- 23. MORPHOLOGICAL STAGES OF HAEMOFLAGELLATES
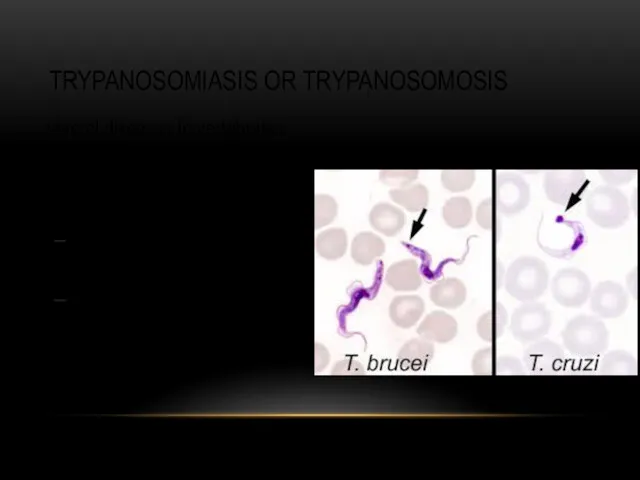
- 24. TRYPANOSOMIASIS OR TRYPANOSOMOSIS ... several diseases in vertebrates caused by parasitic trypanosomes T. cruzi (Chagas disease)
- 25. CHAGAS DISEASE (OR AMERICAN TRYPANOSOMIASIS) Distribution: Mainly in Latin America Infection mode: Invasion through bite wound
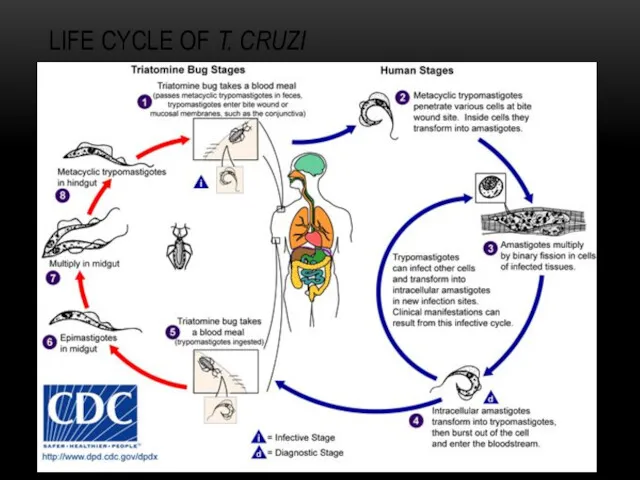
- 26. LIFE CYCLE OF T. CRUZI
- 27. CLINICAL SYMPTOMS, DIAGNOSIS AND PREVENTION Main clinical symptoms: Chagom at bite site, fever, hepatosplenomegaly, cardiomegaly, aneurisms.
- 28. SLEEPING SICKNESS OR AFRICAN TRYPANOSOMIASIS Distribution: 36 countries of sub Saharan Africa Infective stage: Metacyclic trypanosome
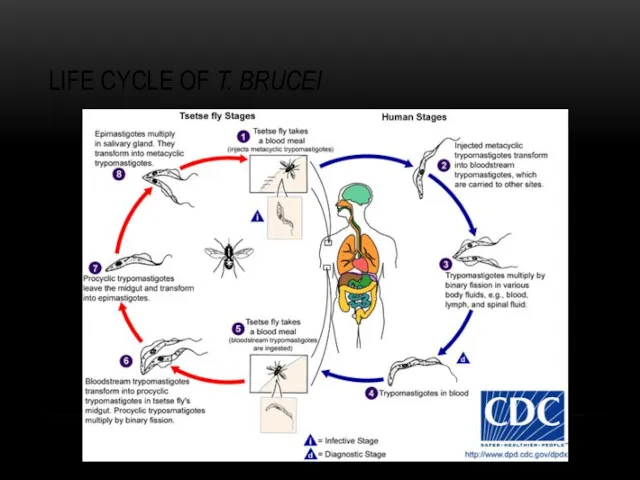
- 29. LIFE CYCLE OF T. BRUCEI
- 30. CLINICAL SYMPTOMS, DIAGNOSIS AND PREVENTION Main clinical symptoms: Fever, local edema, possibly polyadenitis, neural complications, death.
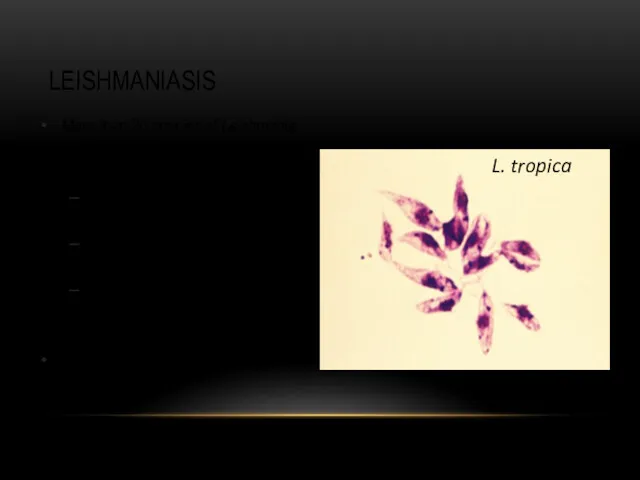
- 31. LEISHMANIASIS More than 20 species of Leishmania infect humans L. donovani (Visceral leishmaniasis or Kala-azar) L.
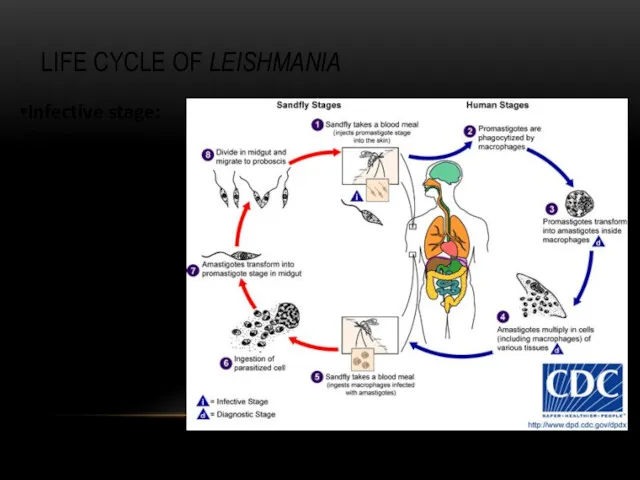
- 32. LIFE CYCLE OF LEISHMANIA Infective stage: Promastigote Mode of infection: Sand fly (Lutzomyia and Phlebotomus)
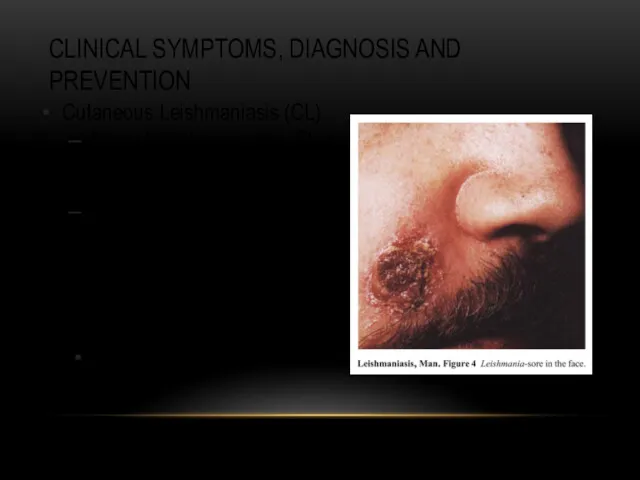
- 33. CLINICAL SYMPTOMS, DIAGNOSIS AND PREVENTION Cutaneous Leishmaniasis (CL) Main clinical symptoms: Skin nodules, ulceration, necrosis. Diagnosis:
- 34. CLINICAL SYMPTOMS, DIAGNOSIS AND PREVENTION Cutaneous Leishmaniasis (CL) Main clinical symptoms: Skin nodules, ulceration, necrosis. Diagnosis:
- 35. DIAGNOSIS AND PREVENTION OF BALANTIDIASIS Diagnosis: Microscopic determination of cysts and trophozoites in fecal smears. Prevention:
- 37. Скачать презентацию




 Бүйрек аурулары
Бүйрек аурулары Нейропсихологические синдромы нарушения памяти. Методы нейропсихологического обследования. Восстановительная работа
Нейропсихологические синдромы нарушения памяти. Методы нейропсихологического обследования. Восстановительная работа Гостра серцева недостатність
Гостра серцева недостатність Всемирный день иммунитета
Всемирный день иммунитета The final impression
The final impression Рак шейки и тела матки
Рак шейки и тела матки Симптоматология острого и хронического гломерулонефрита, пиелонефрита, почечной недостаточности
Симптоматология острого и хронического гломерулонефрита, пиелонефрита, почечной недостаточности Анатомия пәні және мақсаты. Тіндерге, ағзаларға және ағзалар жүйесіне жалпы сипаттама. Адам эмбриогенезінің алғашқы сатысы
Анатомия пәні және мақсаты. Тіндерге, ағзаларға және ағзалар жүйесіне жалпы сипаттама. Адам эмбриогенезінің алғашқы сатысы Лекарственные препараты
Лекарственные препараты Eating Disorders
Eating Disorders ОРВИ и грипп
ОРВИ и грипп Twins diagnostic methods
Twins diagnostic methods Принципы терапии острой почечной недостаточности. Патогенетические сдвиги, клиническая картина
Принципы терапии острой почечной недостаточности. Патогенетические сдвиги, клиническая картина Вывихи и переломы зубов, альвеолярного отростка. Методы лечения
Вывихи и переломы зубов, альвеолярного отростка. Методы лечения Жүктілік және Туберкулез
Жүктілік және Туберкулез Основные аспекты содержания и методики АФК. Адаптивная физическая культура
Основные аспекты содержания и методики АФК. Адаптивная физическая культура Воспаление. Этиология. Медиаторы. Виды. Острое воспаление
Воспаление. Этиология. Медиаторы. Виды. Острое воспаление Павел Захарович Кондоиди (1710-1760)
Павел Захарович Кондоиди (1710-1760) Лабораторная диагностика стафилококковой инфекции
Лабораторная диагностика стафилококковой инфекции Анафилактикалық және гиповолемиялық шок
Анафилактикалық және гиповолемиялық шок Клиническая фармакология лекарственных средств, влияющих на гемостаз
Клиническая фармакология лекарственных средств, влияющих на гемостаз First aid
First aid Жүктілік кезіндегі жатыр мойнының рагі
Жүктілік кезіндегі жатыр мойнының рагі Патофизиология опухолевого роста
Патофизиология опухолевого роста СП при раке желудка
СП при раке желудка Краснуха
Краснуха Возрождение, медицина
Возрождение, медицина Лечение огнестрельных ранений живота
Лечение огнестрельных ранений живота