Содержание
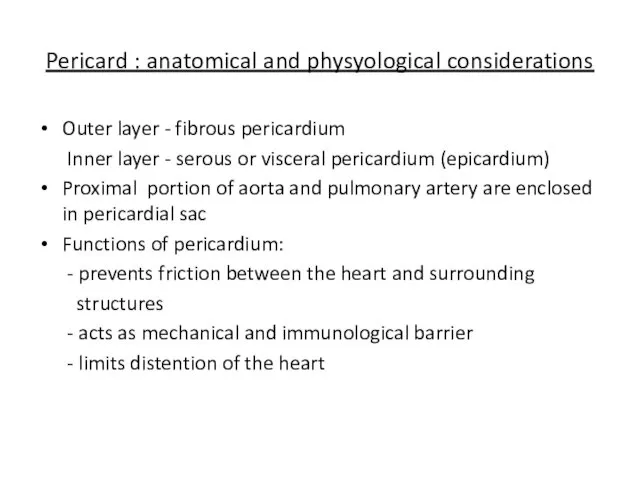
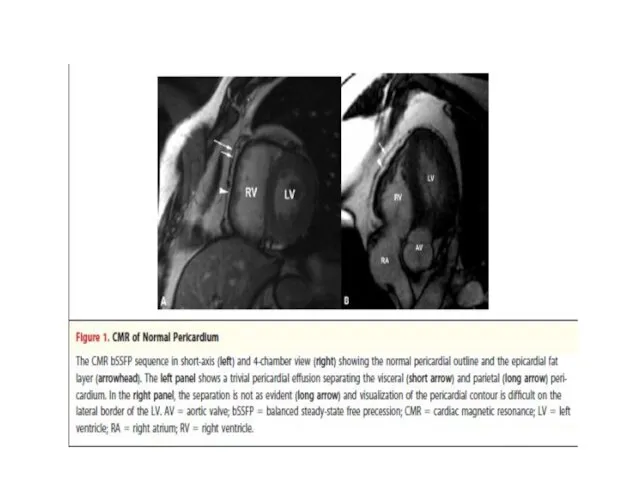
- 2. Pericard : anatomical and physyological considerations Outer layer - fibrous pericardium Inner layer - serous or
- 3. Pericardial fluid In normal hearts there is a small amount of pericardial fluid (25-50 ml) Produced
- 4. Most common forms of pericardial syndromes Acute and recurrent pericarditis Pericardial effusion Cardiac tamponade Constrictive pericarditis
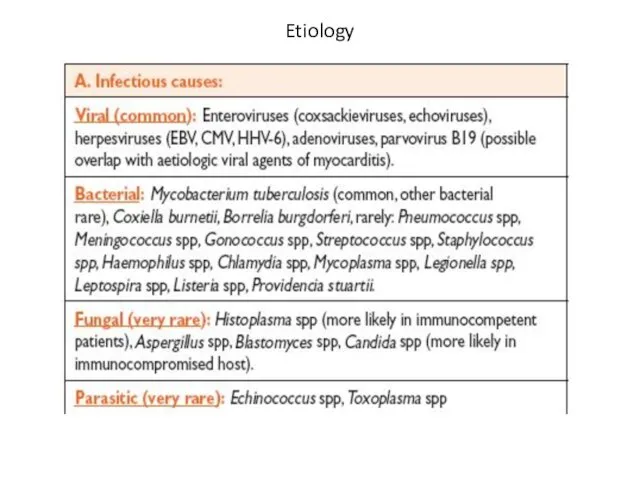
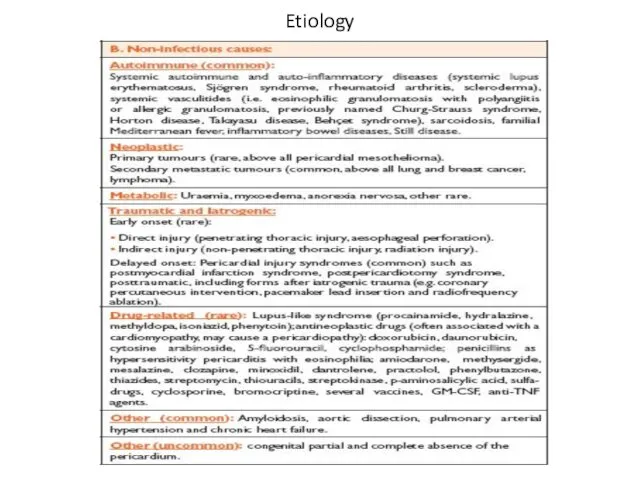
- 6. Etiology
- 7. Etiology
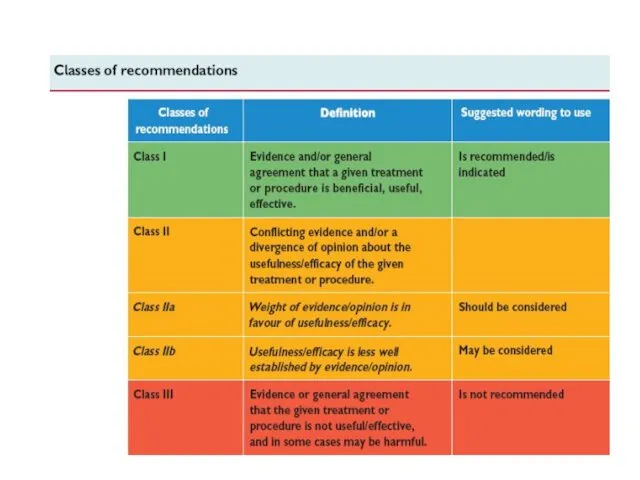
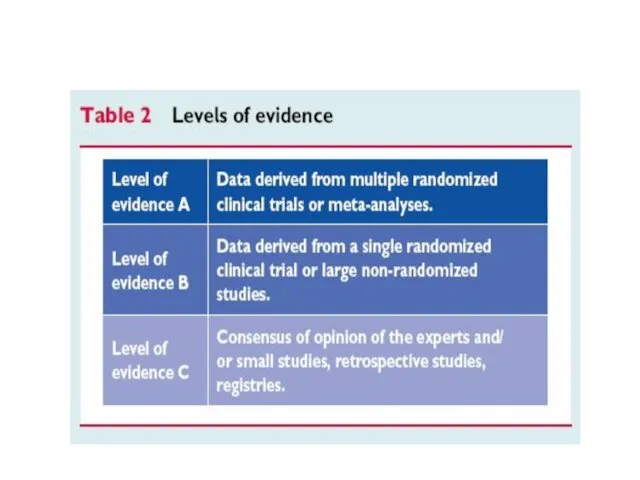
- 8. ESC guidelines 2004
- 12. Acute pericarditis
- 14. Acute pericarditis Most common form of pericardial disease ~5% of presentations to ED for non-ischemic chest
- 15. Acute pericarditis: etiology 80-95% of cases - idiopathic ( in Western Europe and in North America
- 16. Acute pericarditis: etiology (cont’d) Developed countries: emerging cases of pericarditis – iatrogenic posttraumatic, following cardiac surgery,
- 17. Acute pericarditis: etiology (cont’d) Developing countries: high prevalence of tuberculosis-related pericarditis (70-80%) in Sub-Saharian Africa, in
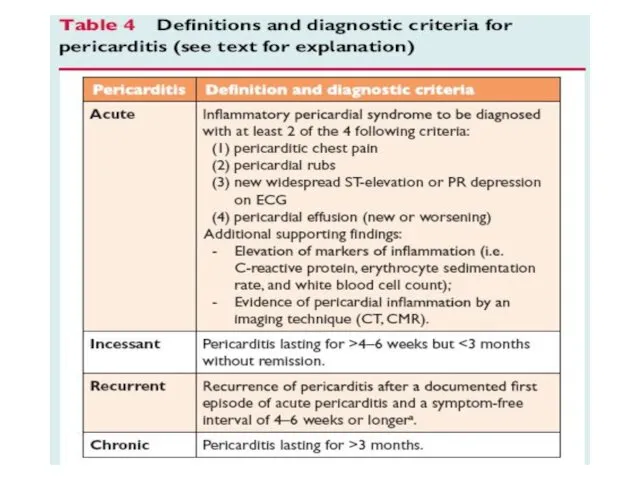
- 18. Acute pericarditis: diagnosis Typical chest pain (pleuritic CP) Pericarial friction rub Widespread ST-segment elevation and PR
- 19. Acute pericarditis: diagnosis Basic diagnostic evaluation Physical examination – auscultation ECG Trans-thoracic echocardiography (TTE) Chest x-ray
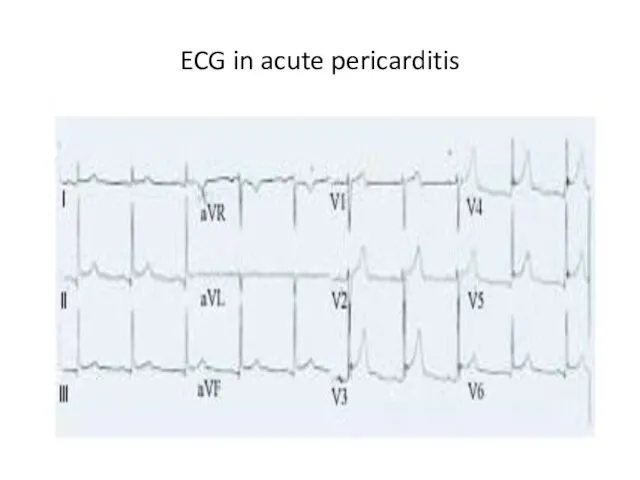
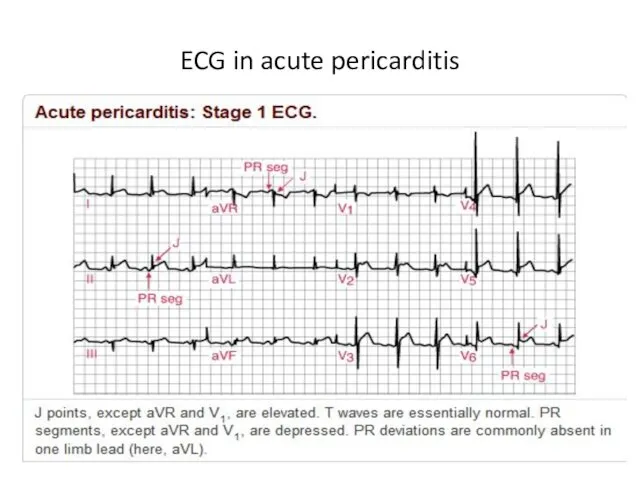
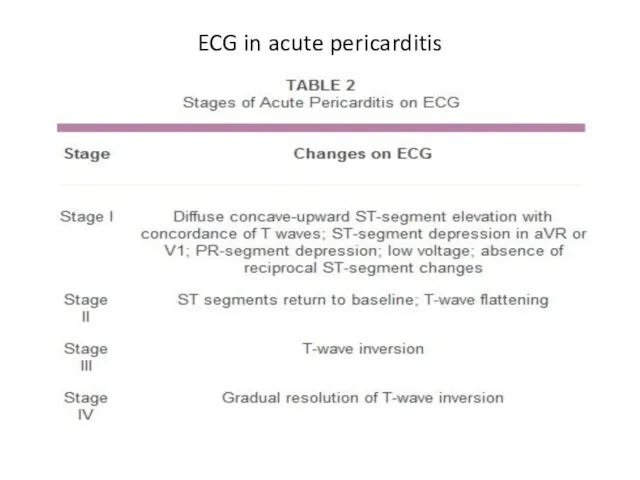
- 20. ECG in acute pericarditis
- 21. ECG in acute pericarditis
- 22. ECG in acute pericarditis
- 23. Acute pericarditis: diagnosis Basic diagnostic evaluation The need for routine etiology search in all cases of
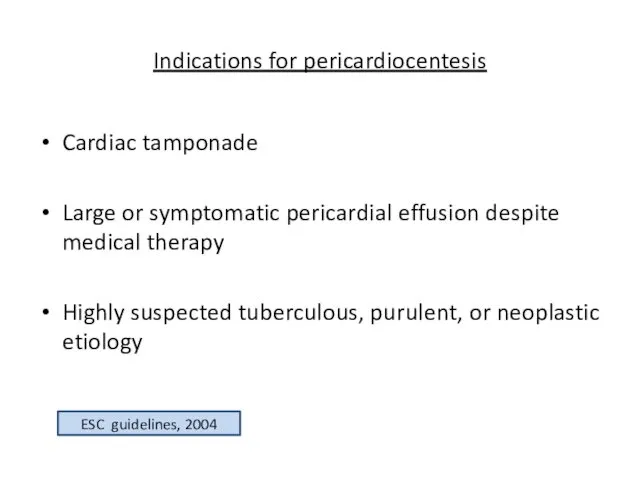
- 24. Indications for pericardiocentesis Cardiac tamponade Large or symptomatic pericardial effusion despite medical therapy Highly suspected tuberculous,
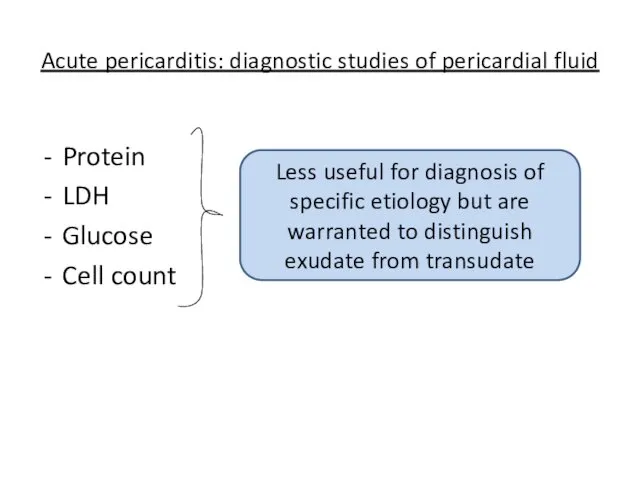
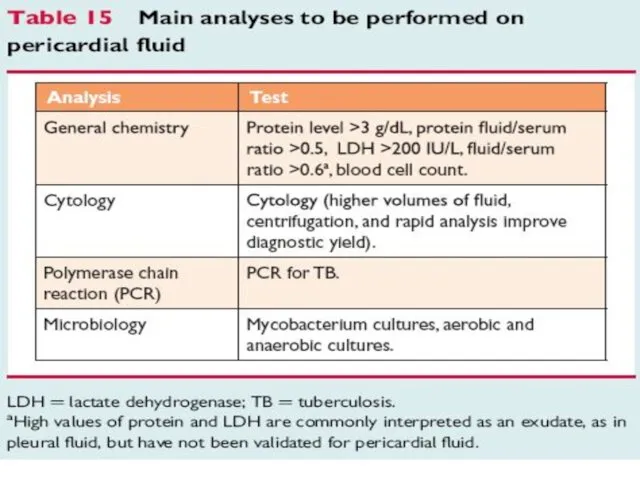
- 25. Acute pericarditis: diagnostic studies of pericardial fluid Protein LDH Glucose Cell count Less useful for diagnosis
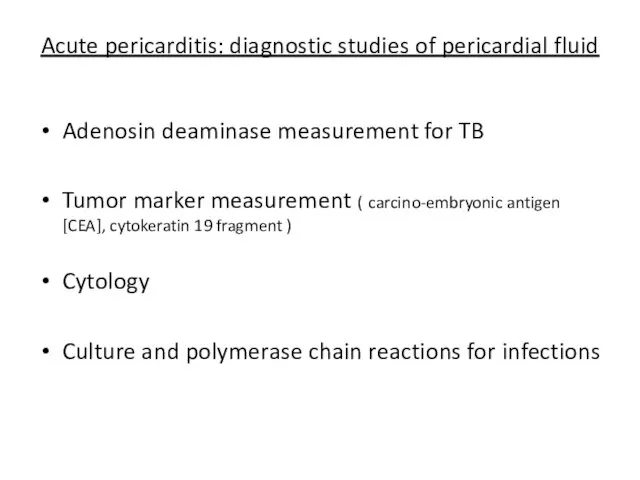
- 26. Acute pericarditis: diagnostic studies of pericardial fluid Adenosin deaminase measurement for TB Tumor marker measurement (
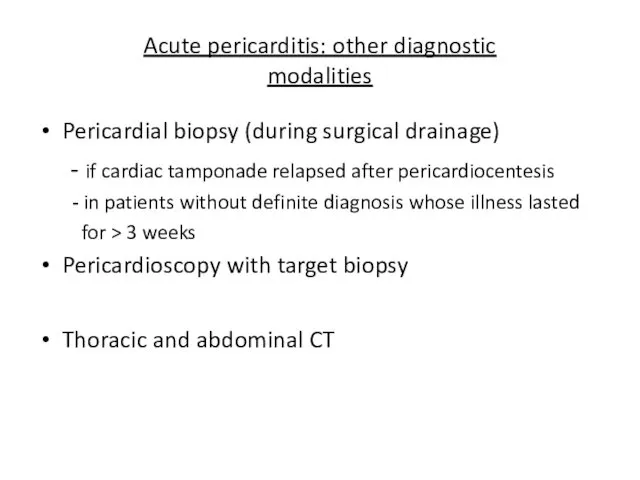
- 27. Acute pericarditis: other diagnostic modalities Pericardial biopsy (during surgical drainage) - if cardiac tamponade relapsed after
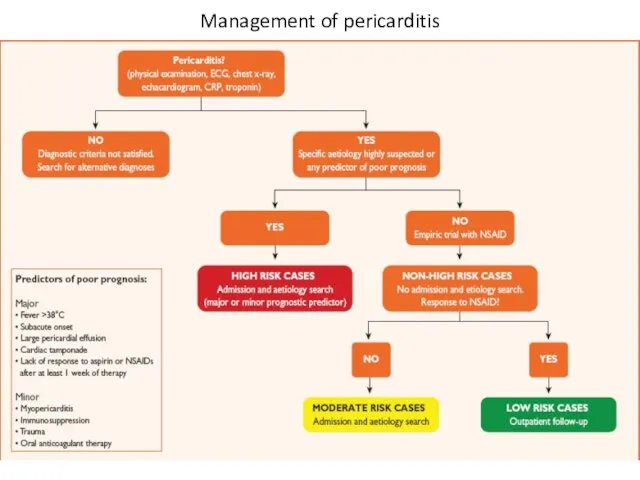
- 28. Management of pericarditis
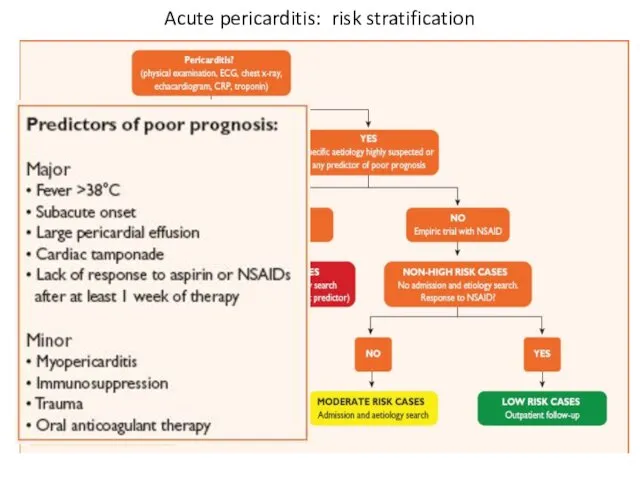
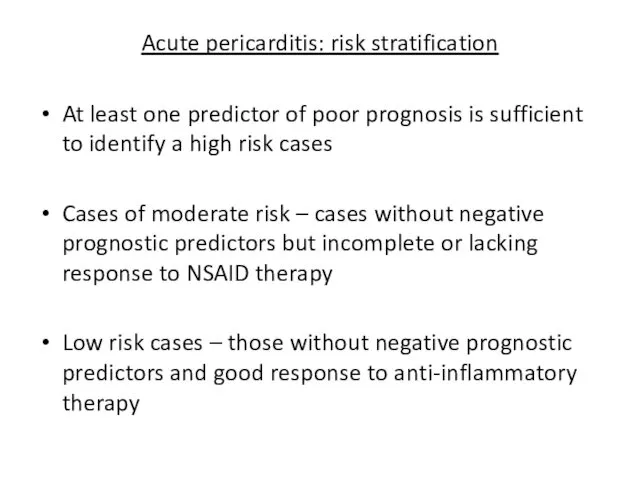
- 29. Acute pericarditis: risk stratification
- 30. Acute pericarditis: risk stratification At least one predictor of poor prognosis is sufficient to identify a
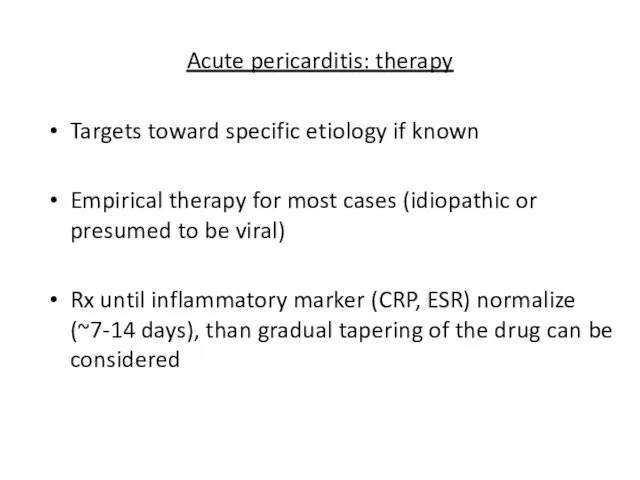
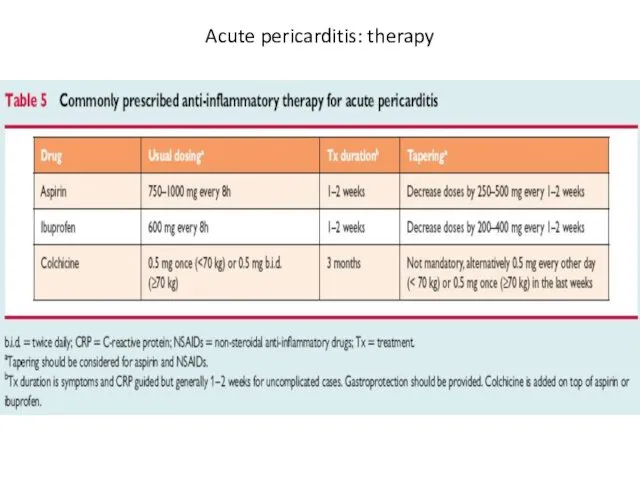
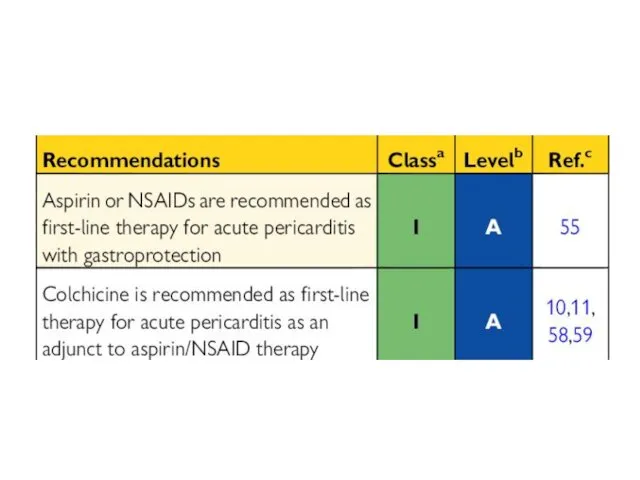
- 31. Acute pericarditis: therapy Targets toward specific etiology if known Empirical therapy for most cases (idiopathic or
- 32. Acute pericarditis: therapy
- 34. NEJM 2013, Sep 1
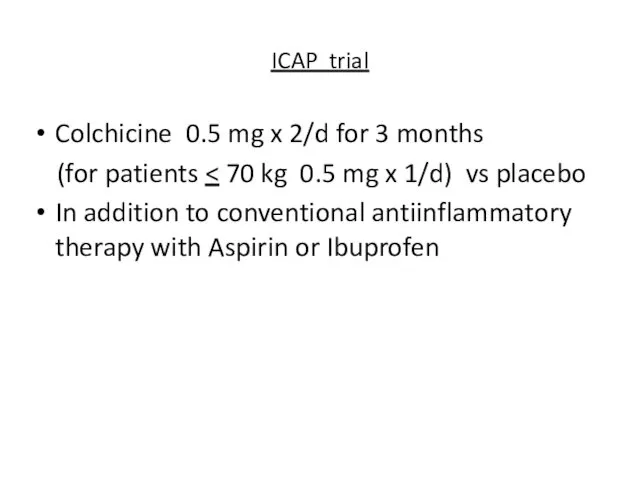
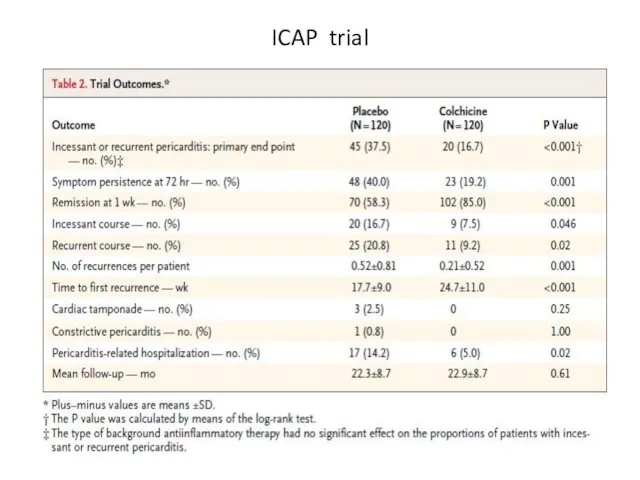
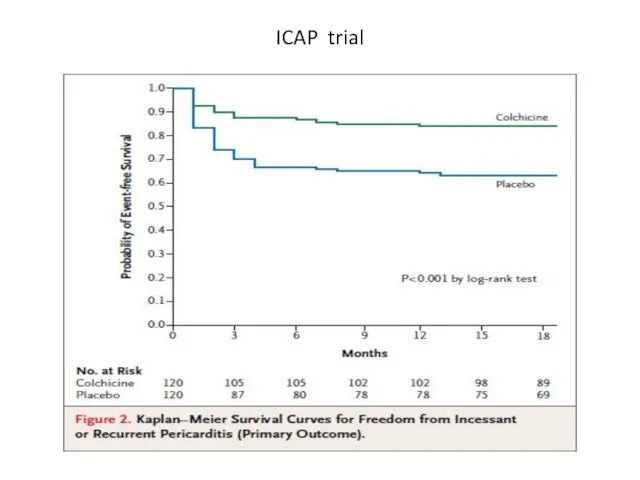
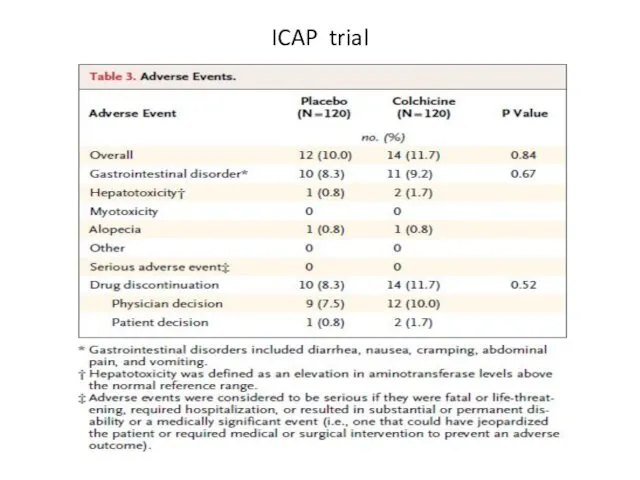
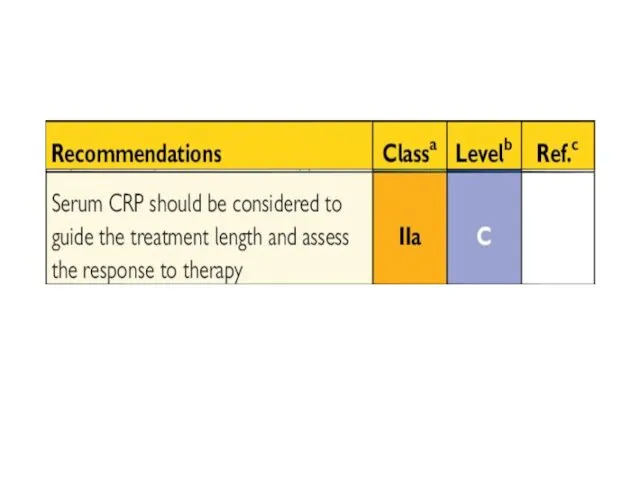
- 35. ICAP trial Colchicine 0.5 mg x 2/d for 3 months (for patients In addition to conventional
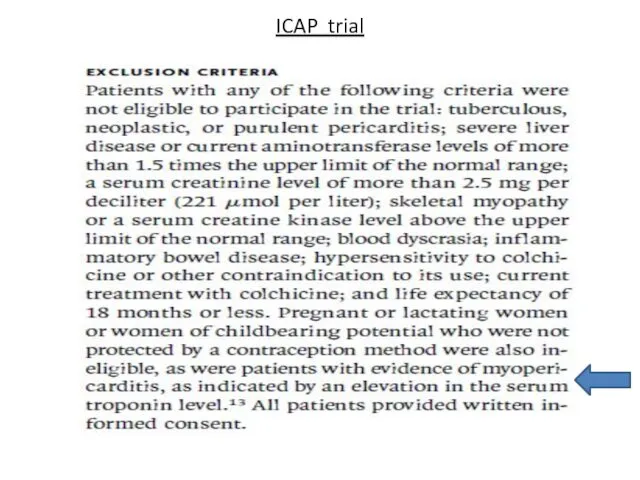
- 36. ICAP trial
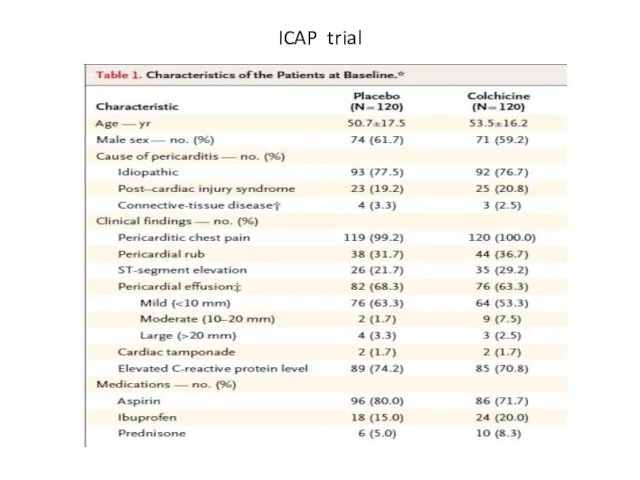
- 37. ICAP trial
- 38. ICAP trial
- 39. ICAP trial
- 40. ICAP trial
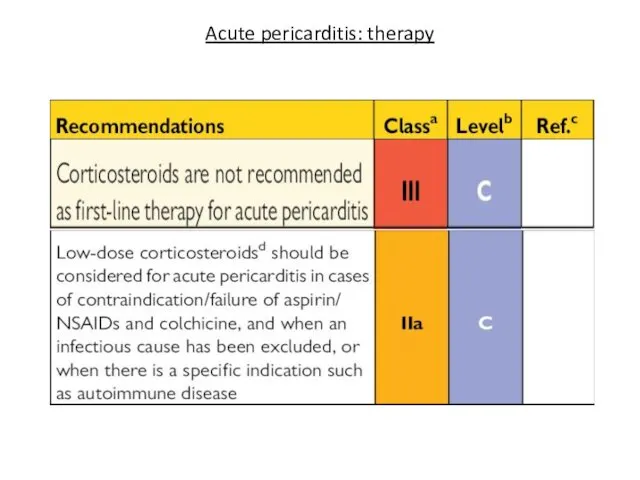
- 42. Acute pericarditis: therapy Corticosteroids increase risk of pericaditis recurrence Indications: - contraindication for aspirin and NSAID
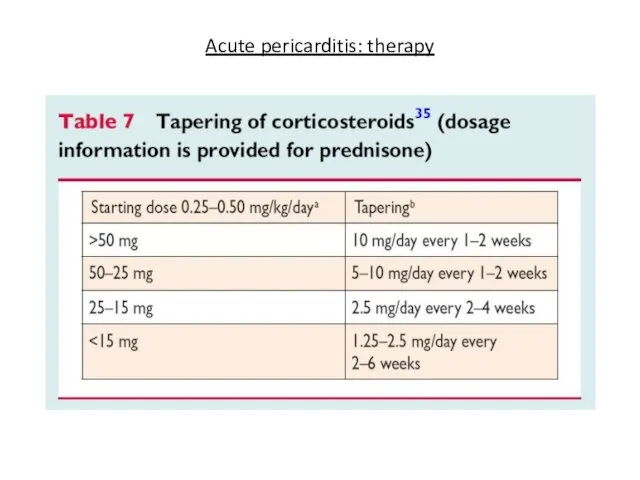
- 43. Acute pericarditis: therapy
- 44. Acute pericarditis: therapy
- 45. Acute pericarditis: therapy (cont’d) Rest and avoidance of physical activity are useful adjunctive measures until active
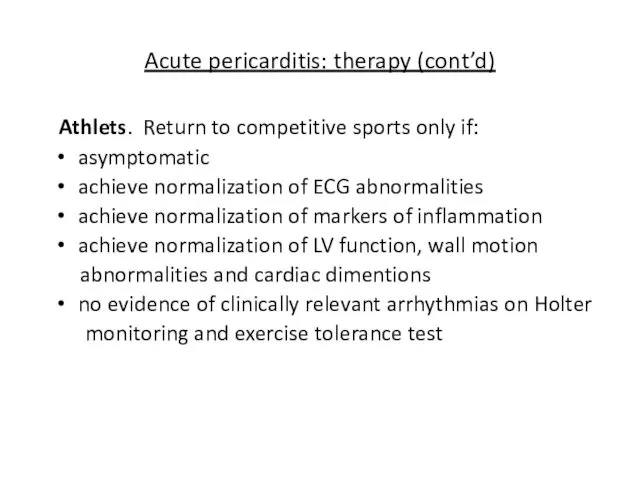
- 46. Acute pericarditis: therapy (cont’d) Athlets. Return to competitive sports only if: asymptomatic achieve normalization of ECG
- 47. Acute pericarditis: prognosis Recurrence is most common complication Incidence ~30% Autoimmune pathogenetic mechanism is most probable
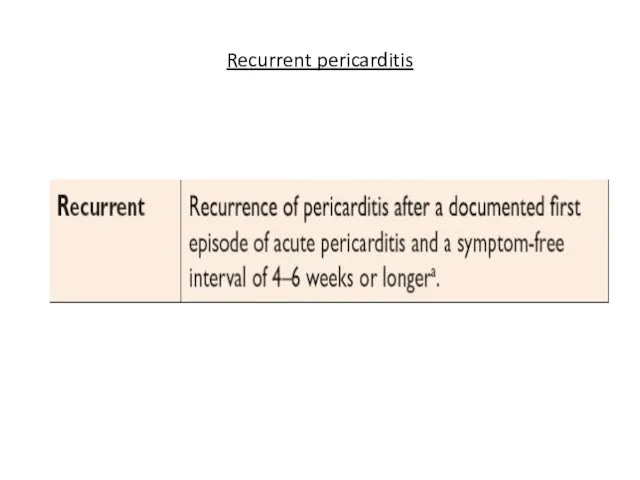
- 48. Recurrent pericarditis
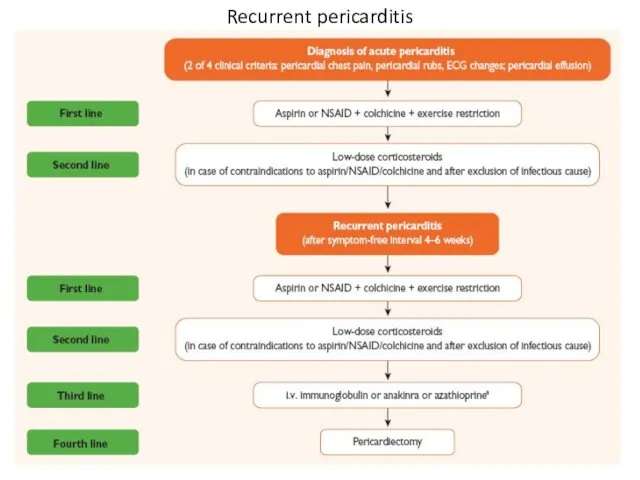
- 49. Recurrent pericarditis
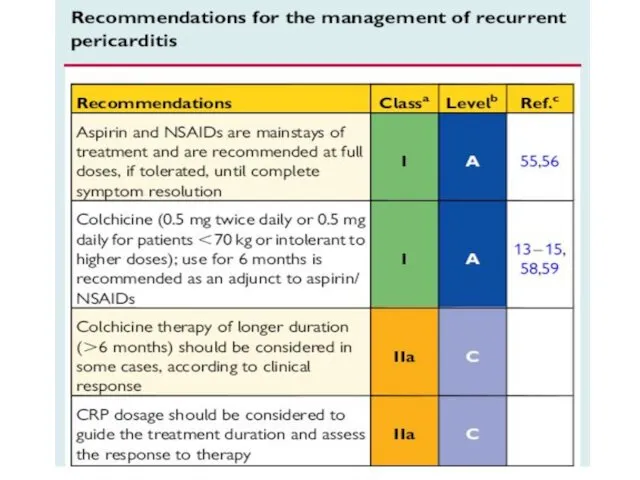
- 50. Recurrent pericarditis: therapy
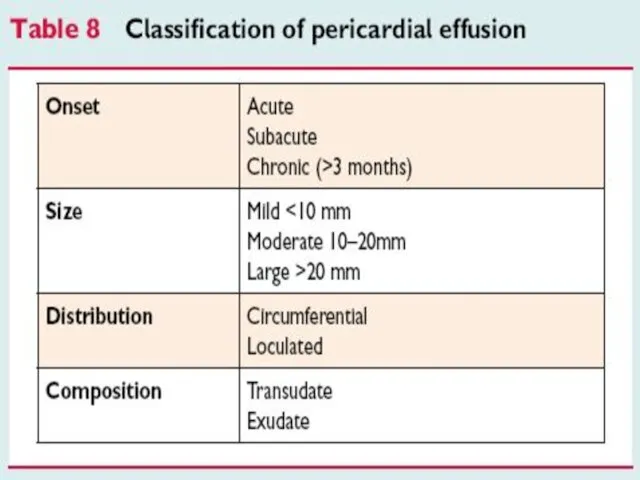
- 51. Pericardial effusion
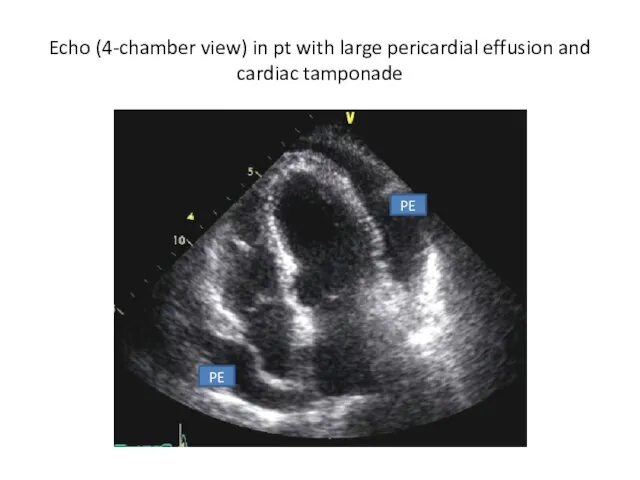
- 52. Echo (4-chamber view) in pt with large pericardial effusion and cardiac tamponade PE PE
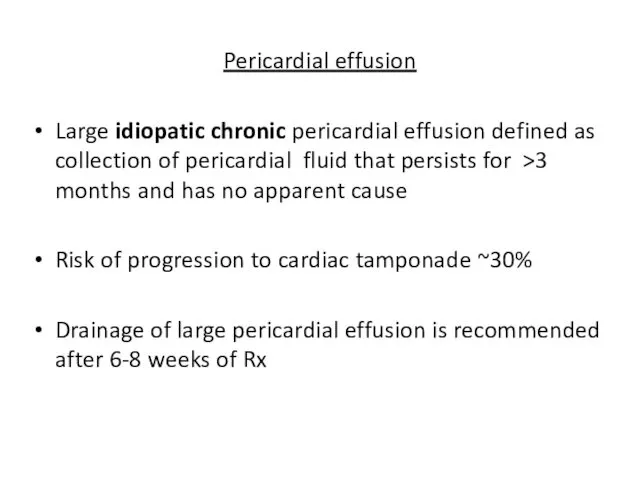
- 54. Pericardial effusion Large idiopatic chronic pericardial effusion defined as collection of pericardial fluid that persists for
- 55. Pericardial effusion Pericardiectomy is recommended in a case of large effusion after pericardiocentesis No medical therapy
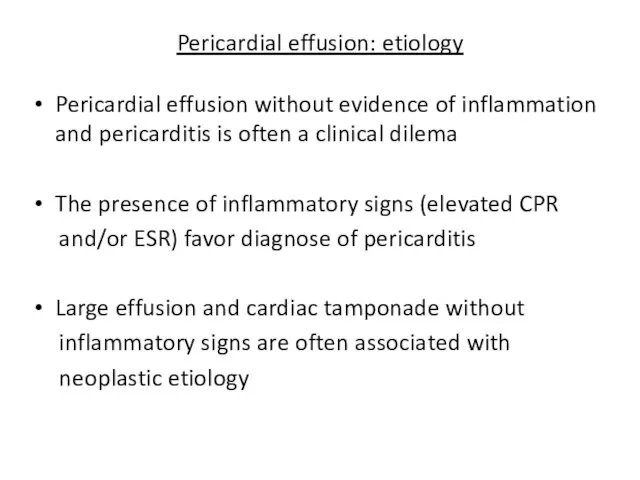
- 56. Pericardial effusion: etiology Pericardial effusion without evidence of inflammation and pericarditis is often a clinical dilema
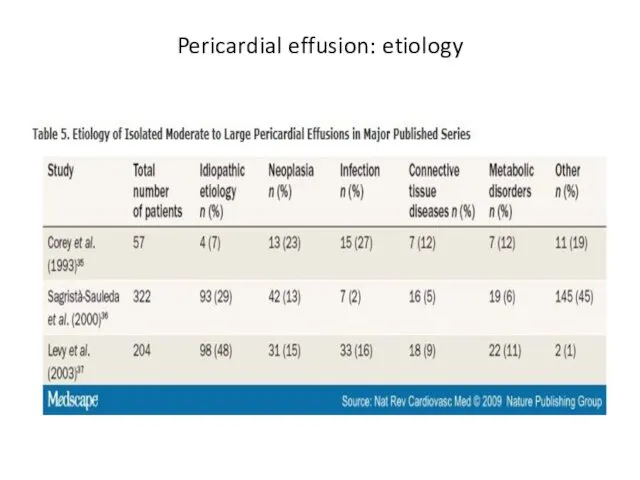
- 57. Pericardial effusion: etiology
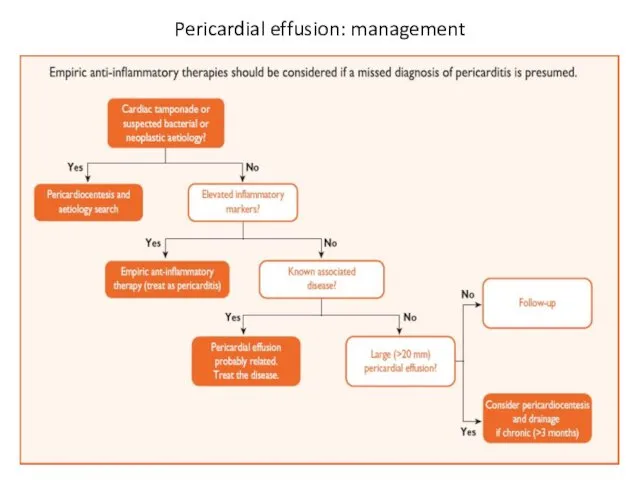
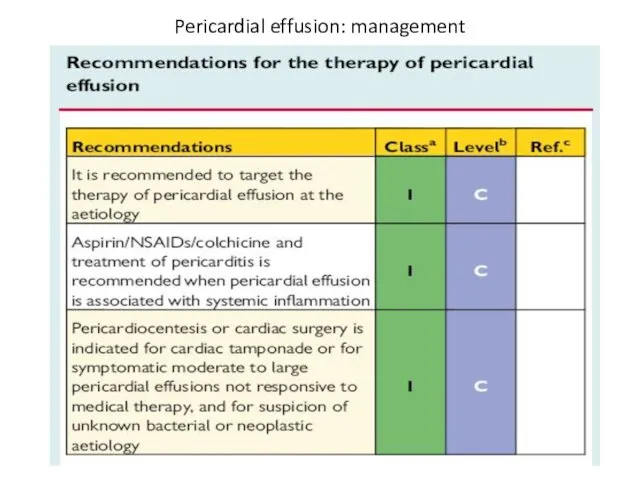
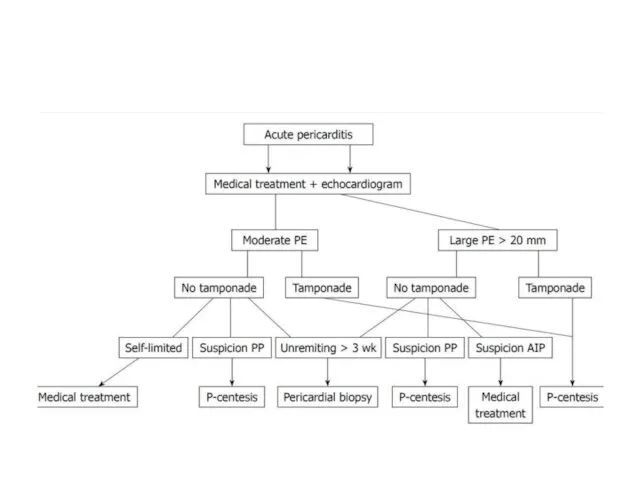
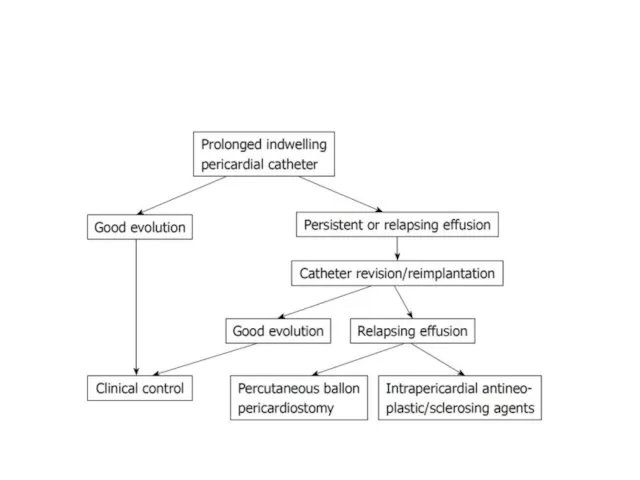
- 58. Pericardial effusion: management
- 59. Pericardial effusion: management
- 60. Pericardial effusion: management
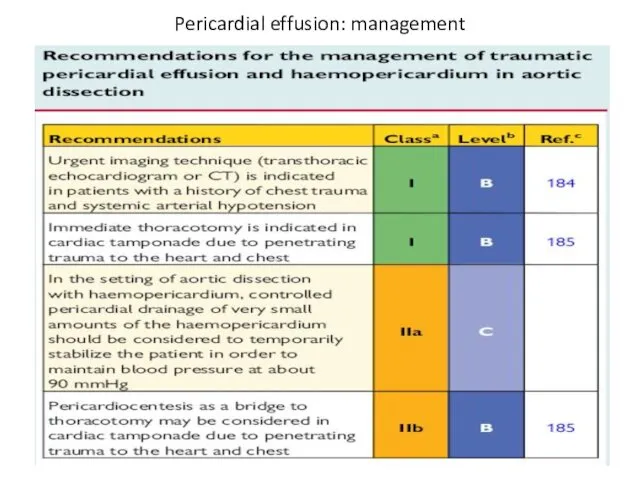
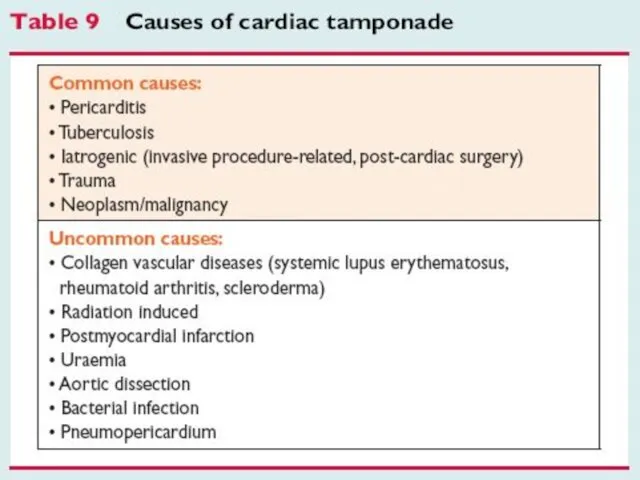
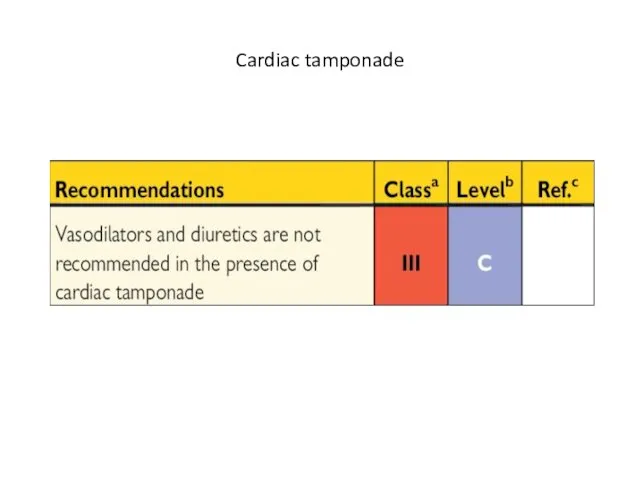
- 61. Cardiac tamponade
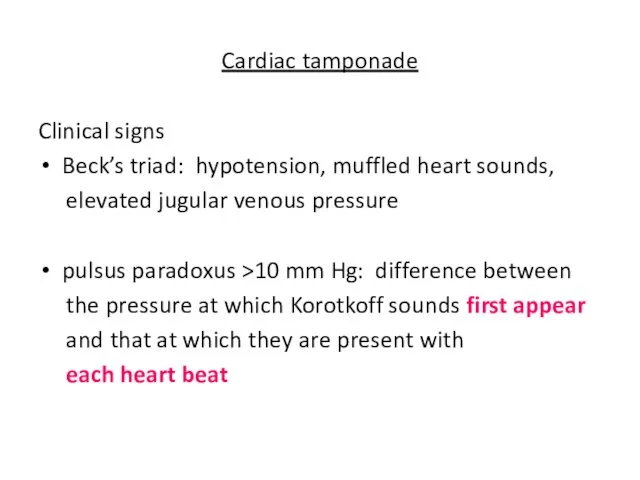
- 63. Cardiac tamponade Clinical signs Beck’s triad: hypotension, muffled heart sounds, elevated jugular venous pressure pulsus paradoxus
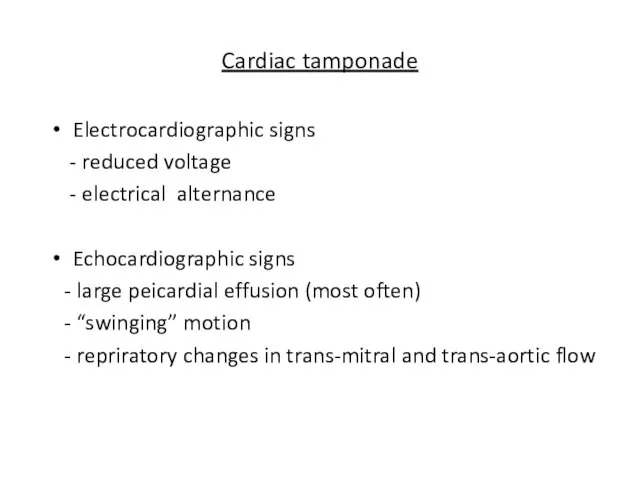
- 64. Cardiac tamponade Electrocardiographic signs - reduced voltage - electrical alternance Echocardiographic signs - large peicardial effusion
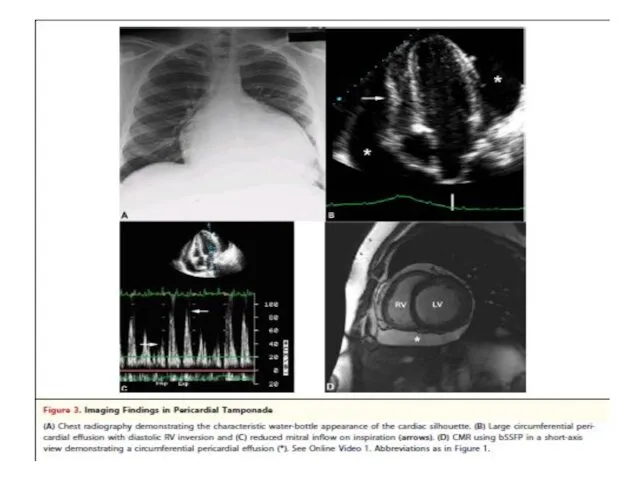
- 66. Cardiac tamponade
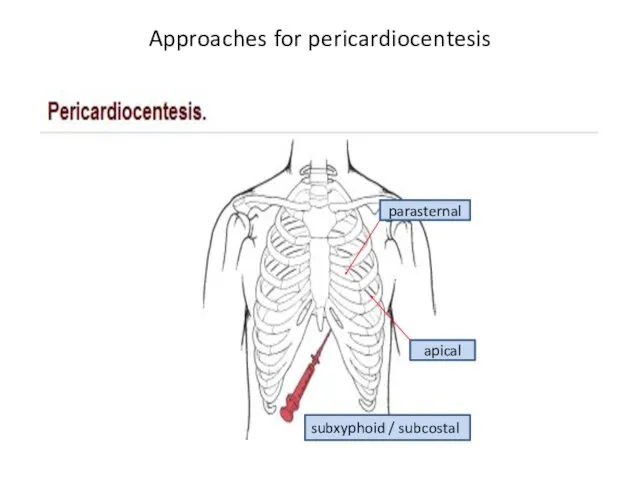
- 67. Approaches for pericardiocentesis parasternal apical subxyphoid / subcostal
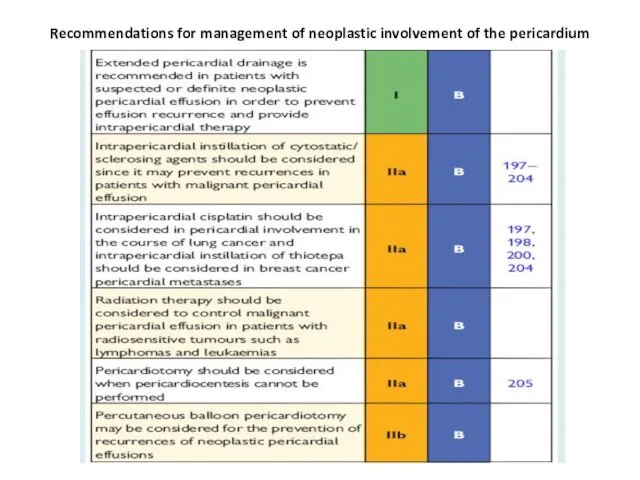
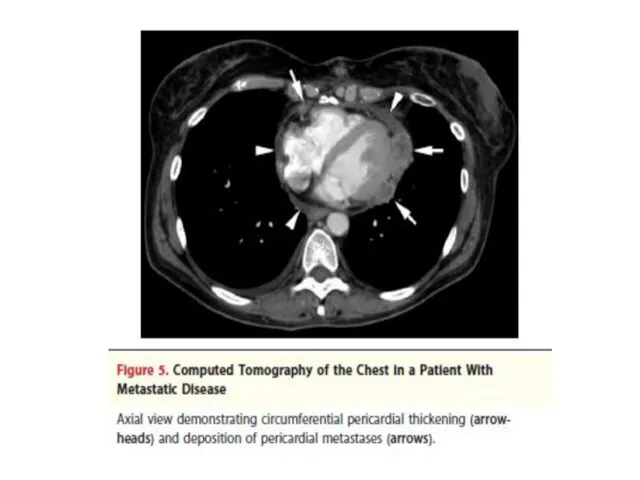
- 69. Recommendations for management of neoplastic involvement of the pericardium
- 70. Constrictive pericarditis
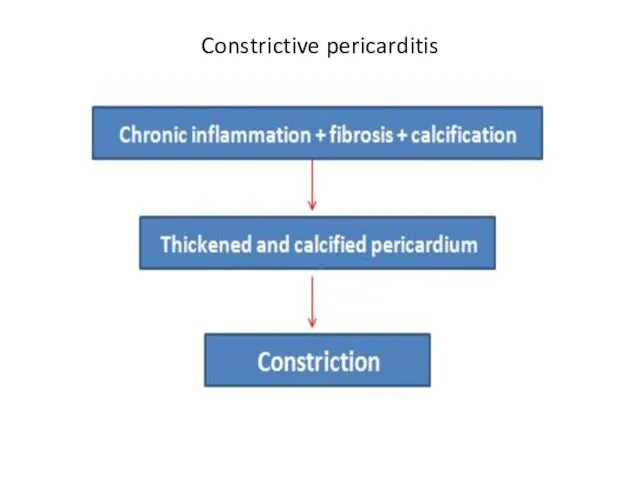
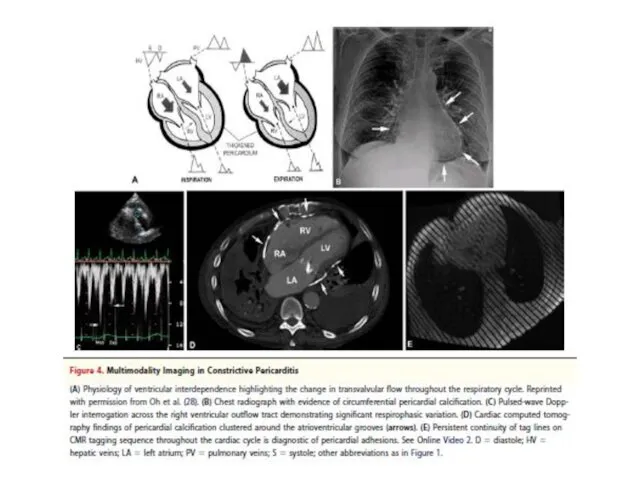
- 71. Constrictive pericarditis
- 73. Constrictive pericarditis Fibrotic pericardium impedes normal diastolic filling because of loss of elasticity Usually pericardium is
- 74. Constrictive pericarditis: etiology Idiopathic or viral - 42-49% Cardiac surgery - 11-37% Radiation Rx - 9-31%
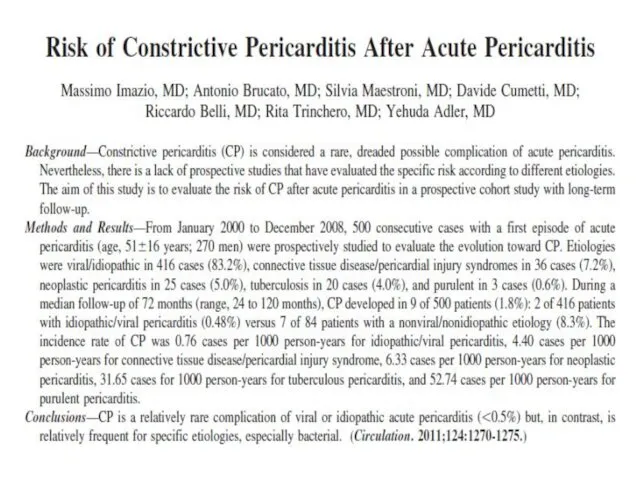
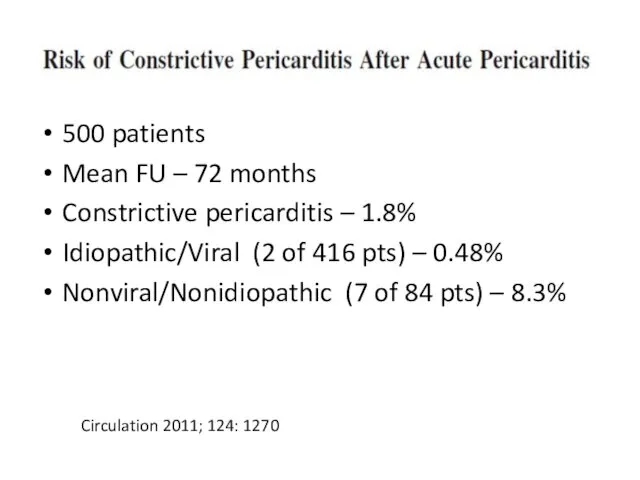
- 76. 500 patients Mean FU – 72 months Constrictive pericarditis – 1.8% Idiopathic/Viral (2 of 416 pts)
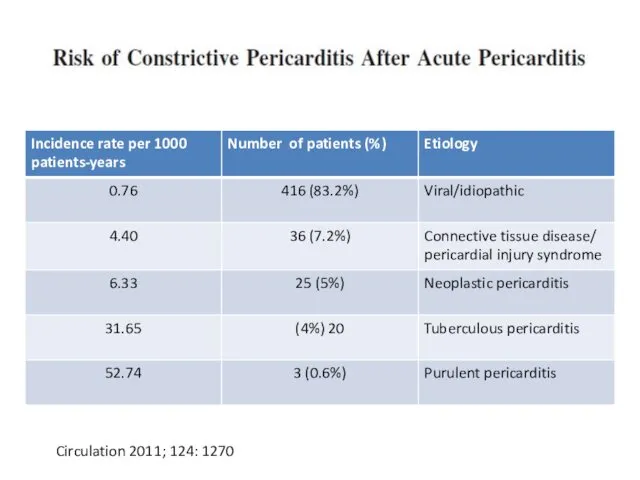
- 77. Circulation 2011; 124: 1270
- 78. Constrictive pericarditis: symptoms Right heart failure: range from periferal edema to anasarca No pulmonary congestion Usually
- 79. Constrictive pericarditis Pericardial constriction should be considered in any patient with unexplained elevation of jugular venous
- 81. Transient constrictive pericarditis 10-20% of cases during resolution of pericardial inflammation Patients with newly diagnosed constrictive
- 82. Effusive constrictive pericarditis In 8% of patients with cardiac tamponade who underwent pericardiocentesis and cardiac catheterization
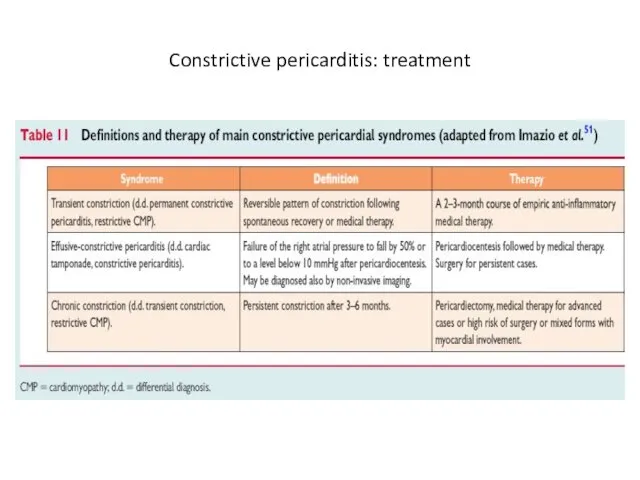
- 83. Constrictive pericarditis: treatment
- 84. Thank you for attention
- 85. Backup slides
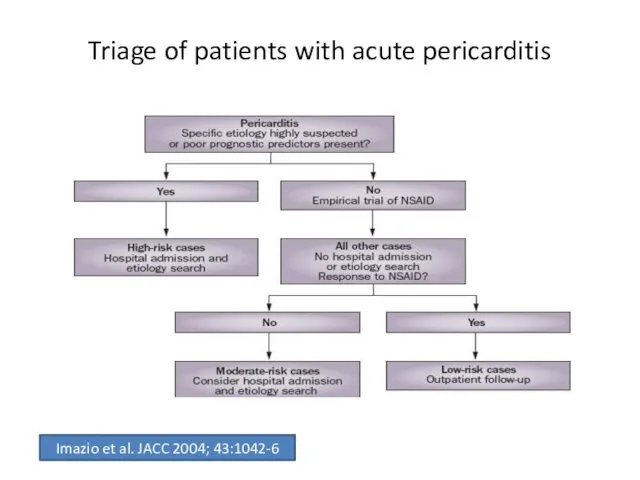
- 94. Triage of patients with acute pericarditis Imazio et al. JACC 2004; 43:1042-6
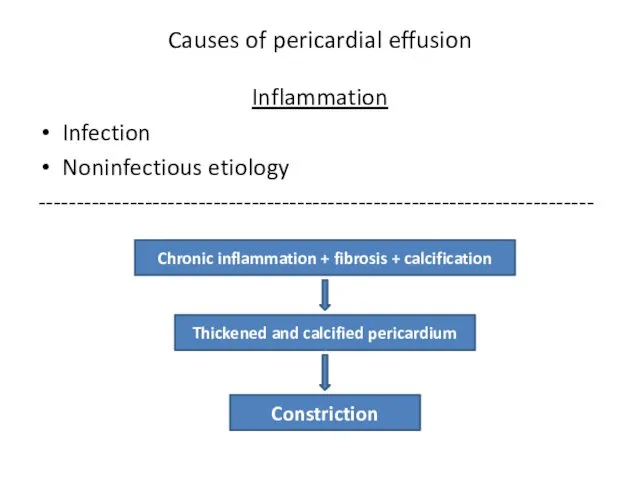
- 95. Causes of pericardial effusion Inflammation Infection Noninfectious etiology ------------------------------------------------------------------------- Chronic inflammation + fibrosis + calcification Thickened
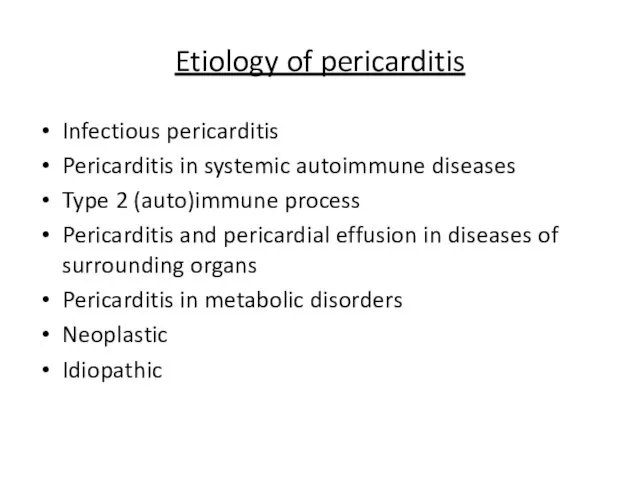
- 96. Etiology of pericarditis Infectious pericarditis Pericarditis in systemic autoimmune diseases Type 2 (auto)immune process Pericarditis and
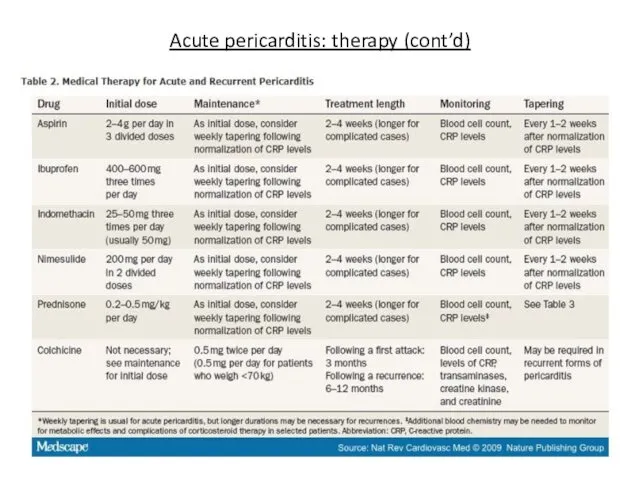
- 97. Acute pericarditis: therapy (cont’d)
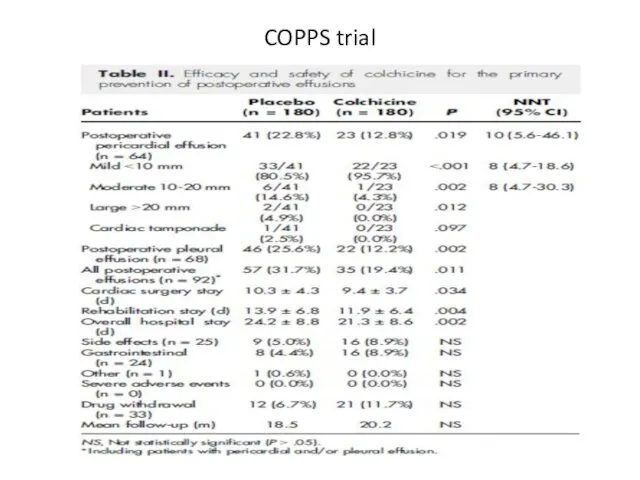
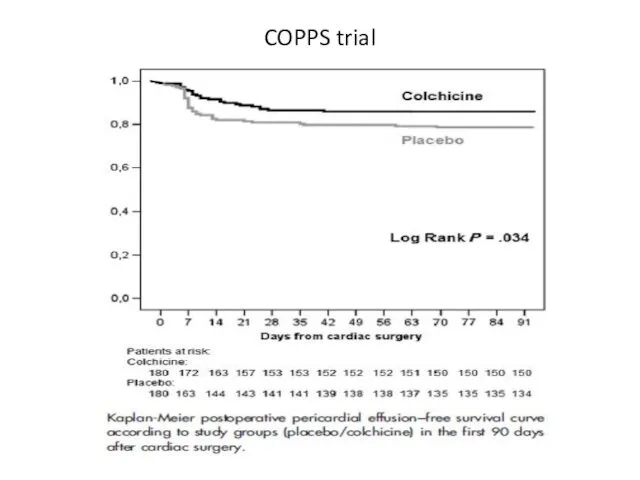
- 98. COPPS trial Am Heart J 2011; 62:527-32
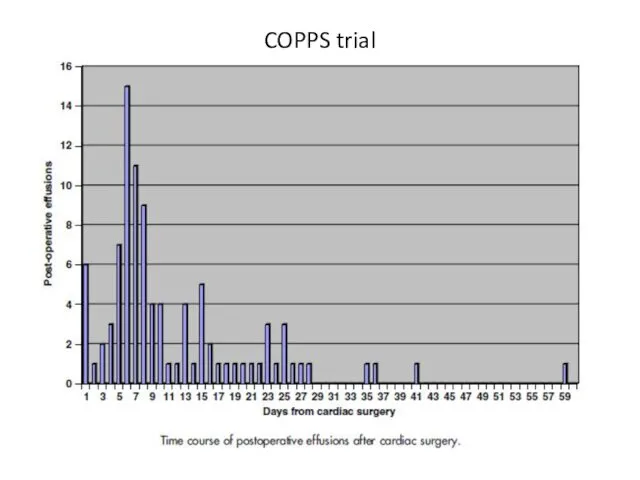
- 99. COPPS trial
- 100. COPPS trial
- 101. COPPS trial
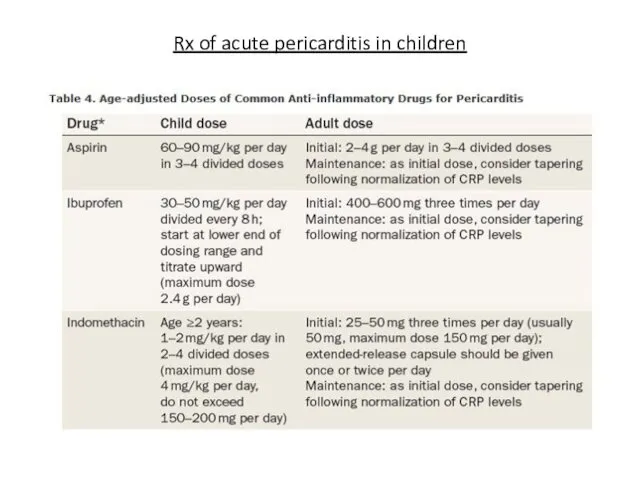
- 102. Rx of acute pericarditis in children
- 104. Скачать презентацию


 Необратимое повреждение – некроз
Необратимое повреждение – некроз Кадровая политика в здравоохранении. Критерии оценки и совершенствование
Кадровая политика в здравоохранении. Критерии оценки и совершенствование Жедел аппендицит
Жедел аппендицит узи
узи Понятие об иммунитете. Строение иммунной системы. Антигены
Понятие об иммунитете. Строение иммунной системы. Антигены Наркотики. Їх види та вплив
Наркотики. Їх види та вплив Жедел ішек инфекциялары
Жедел ішек инфекциялары Гормональные лекарственные средства
Гормональные лекарственные средства Анатомия и физиология полости рта. Анатомия зубов. Гистология твердых тканей зуба. Рентгенанатомия зубов
Анатомия и физиология полости рта. Анатомия зубов. Гистология твердых тканей зуба. Рентгенанатомия зубов Цирроз печени
Цирроз печени Морфологические группы лекарственного растительного сырья и их особенности
Морфологические группы лекарственного растительного сырья и их особенности Кеуде қуысының жарақаты. Қабырға, омыртқа сынуы
Кеуде қуысының жарақаты. Қабырға, омыртқа сынуы ОРВИ и грипп
ОРВИ и грипп Диета №9: лечебное питание при сахарном диабете
Диета №9: лечебное питание при сахарном диабете Противосудорожные препараты
Противосудорожные препараты Опухоль. Доброкачественные и злокачественные опухоли
Опухоль. Доброкачественные и злокачественные опухоли Принципы Рационального Питания
Принципы Рационального Питания Ауыл тұрғындарына алғашқы медико – санитарлық көмекті ұйымдастыру
Ауыл тұрғындарына алғашқы медико – санитарлық көмекті ұйымдастыру Bronchial asthma in children (treatment)
Bronchial asthma in children (treatment) Субмукозная миома матки
Субмукозная миома матки Болезни гипофиза: МСЭ и реабилитация
Болезни гипофиза: МСЭ и реабилитация Системная красная волчанка
Системная красная волчанка Клиническая психология
Клиническая психология Улану кезіндегі шұғыл көмек
Улану кезіндегі шұғыл көмек Миокардиты у детей
Миокардиты у детей Патогенез гнойно-воспалительных заболеваний
Патогенез гнойно-воспалительных заболеваний Создание единого цифрового контура в здравоохранении
Создание единого цифрового контура в здравоохранении Первая медицинская помощь при массовых поражениях
Первая медицинская помощь при массовых поражениях