Содержание
- 2. DIPHTHERIA An acute, contagious disease caused by Corynebacterium diphtheriae, characterized by the formation of a fibrinous
- 3. Etiology Three biotypes of C. diphtheriae exist (mitis, intermedius, and gravis) Only toxinogenic isolates produce exotoxin
- 4. Epidemiology Humans are the only known reservoir for C. diphtheriae Spread is chiefly by the secretions
- 5. Pathogenesis the microorganisms lodge in the tonsil or nasopharynx, and multiply toxinogenic C. diphtheriae with produce
- 6. exotoxin, carried by the blood damages cells in distant organs, creating pathologic lesions in the respiratory
- 7. Symptoms and Signs The incubation period ranges between 1 and 4 days Initially, the patient with
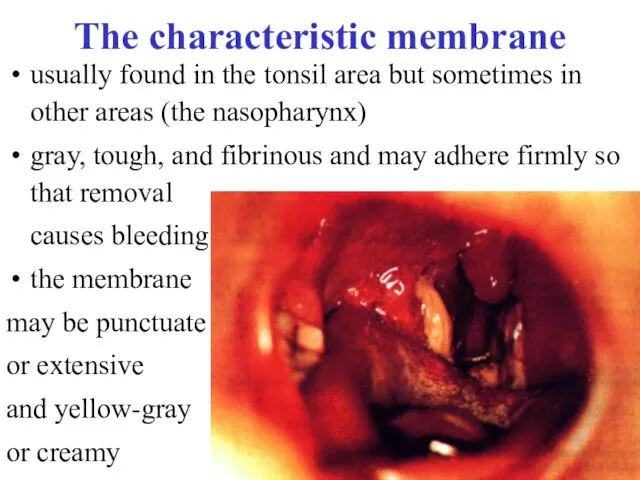
- 8. The characteristic membrane usually found in the tonsil area but sometimes in other areas (the nasopharynx)
- 9. When disease progresses, dysphagia, toxemia, and prostration are prominent The cervical lymph glands are enlarged. Pharyngeal
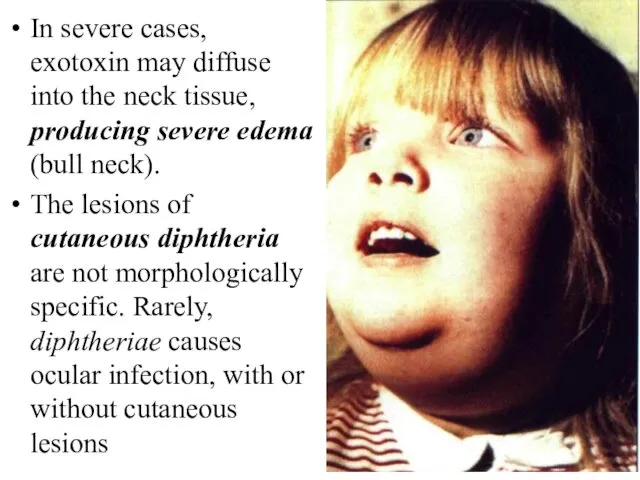
- 10. In severe cases, exotoxin may diffuse into the neck tissue, producing severe edema (bull neck). The
- 11. Complications Severe complications are likely if antitoxin is not given promptly on the basis of clinical
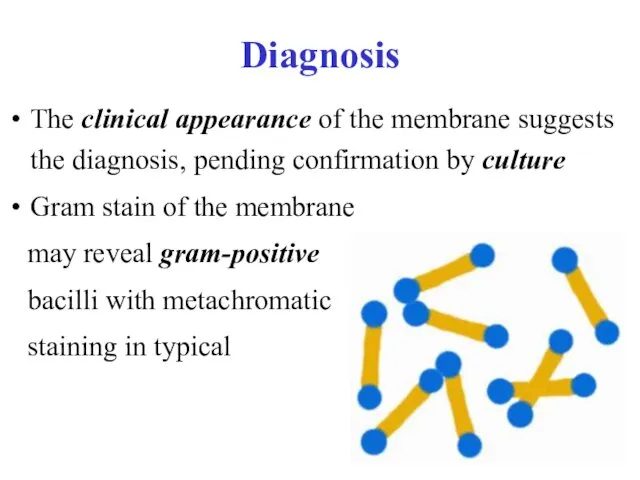
- 12. Diagnosis The clinical appearance of the membrane suggests the diagnosis, pending confirmation by culture Gram stain
- 13. Material for culture should be obtained from below the membrane, or a portion of membrane itself
- 14. Treatment Diphtheria antitoxin must be given early, since the antitoxin neutralizes only toxin not yet bound
- 15. Administered antitoxin After 20 minutes, you must meter papule too, and if it smaller then 10
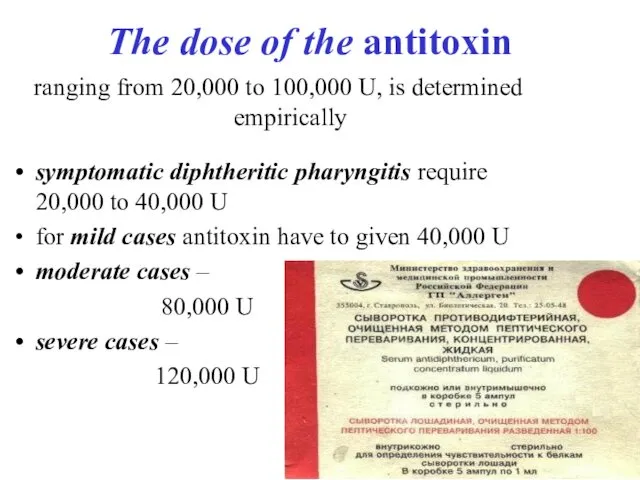
- 16. The dose of the antitoxin ranging from 20,000 to 100,000 U, is determined empirically symptomatic diphtheritic
- 17. Antimicrobial treatment is required to eradicate the organism and prevent spread; it is not a substitute
- 18. Prophylaxis Active immunization with diphtheria-tetanus-pertussis (DTP) vaccine should be routinely given to all children and all
- 19. Management of an Outbreak All symptomatic patients should be isolated Contact precautions (private room, use of
- 20. INFECTIOUS MONONUCLEOSIS is an acute disease which, characterized by fever, pharyngitis, and lymphadenopathy and cause Epstein-Barr
- 21. Etiology and Pathophysiology Epstein-Barr virus (EBV) is a herpesvirus with a host range limited primarily to
- 22. Epidemiology EBV is relatively labile and is not very contagious In most cases, the incubation period
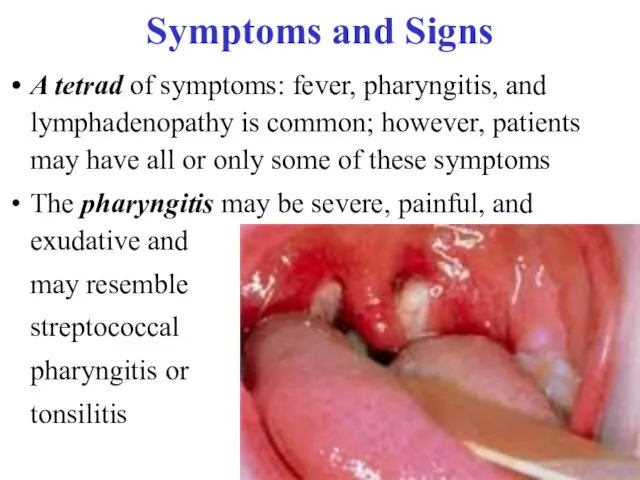
- 23. Symptoms and Signs A tetrad of symptoms: fever, pharyngitis, and lymphadenopathy is common; however, patients may
- 24. Lymphadenopathy may involve any group of nodes but is usually symmetric; anterior and posterior cervical adenopathy
- 25. Complications Neurosis complications include encephalitis, Guieain-Barre syndrome, peripheral neuropathy, aseptic meningitis, myelitis, cranial nerve palsies, and
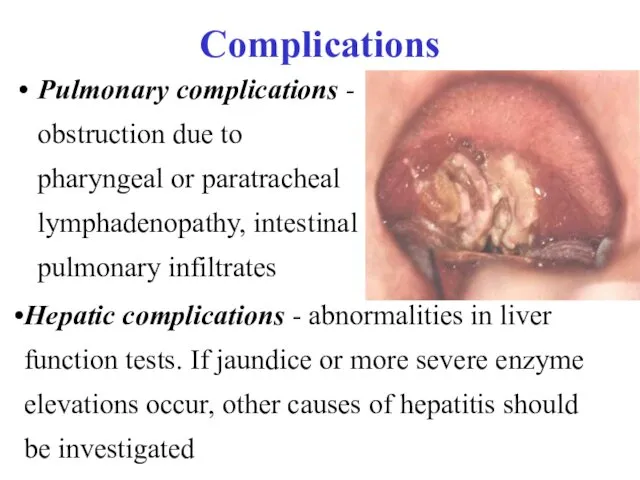
- 26. Complications Pulmonary complications - obstruction due to pharyngeal or paratracheal lymphadenopathy, intestinal pulmonary infiltrates Hepatic complications
- 27. Laboratory Findings and Diagnosis the clinical syndrome of infectious mononucleosis and its epidemiologic setting may be
- 28. resulting from reactive lymphocytes that are morphologically atypical to varying degrees (mononuclear)
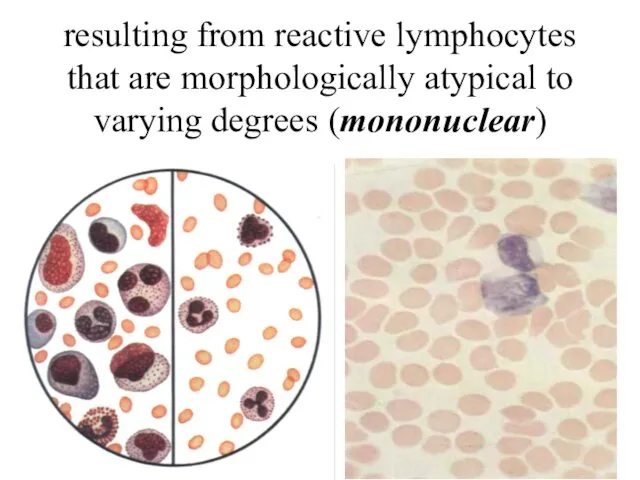
- 29. Differential Diagnosis The pharyngitis, lymphadenopathy, and fever may be clinically indistinguishable from that caused by group
- 30. Prognosis Infectious mononucleosis is usually self-limited The duration of the illness varies; the acute phase lasts
- 31. Treatment Patients should be encouraged to rest during the acute phase because of the risk of
- 32. Varicella is an acute infectious disease, characterized by vesicular eruption with transparent liquid on skin and
- 33. Etiology and Epidemiology The Varicella virus contains DNA. Varicella and herpes zoster were proved to be
- 34. Pathogenesis and pathology The portal of entry is the mucous membrane of the upper respiratory tract
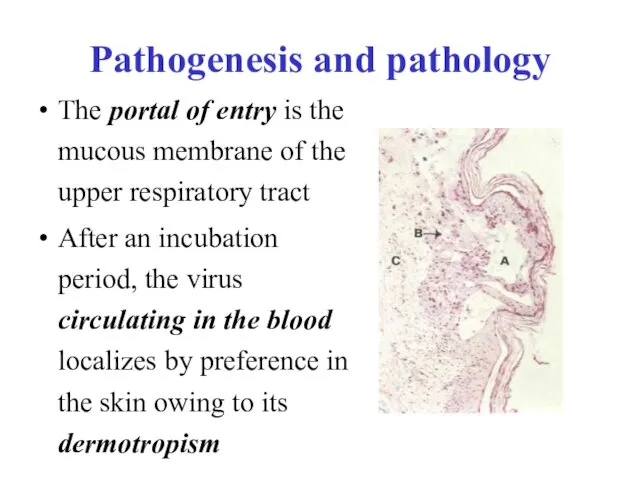
- 35. In very rare cases the lungs, liver, spleen, kidneys, pancreas, and other internal organs may be
- 36. Clinical manifestations The incubation period averages 11-21 days The outbreak of rash coincides with a rise
- 37. Vesicles are round or oval, differ in size, and are seated superficially on an uneducated base;
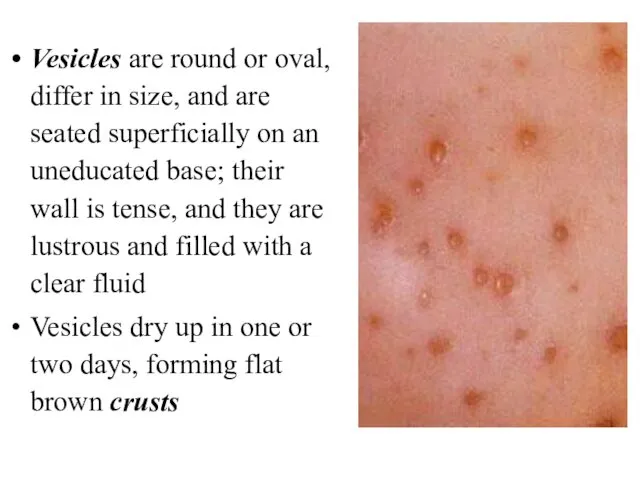
- 38. Atypical forms In the bullous form of varicella large flabby bullae develop (up to two or
- 39. Complications Complications are rare in Varicella: keratitis, laryngitis, abscesses, phlegmons, stomatitis, otitis, lymphadenitis and bronchopneumonia Individual
- 41. Скачать презентацию
 Микотоксины. Действие микотоксинов в истории
Микотоксины. Действие микотоксинов в истории Общие принципы лечения абсцессов и флегмон лица и шеи. Физиотерапия и реабилитация больных
Общие принципы лечения абсцессов и флегмон лица и шеи. Физиотерапия и реабилитация больных Диспансерное наблюдение за детьми с хроническими заболеваниями
Диспансерное наблюдение за детьми с хроническими заболеваниями Хронические расстройства питания у детей
Хронические расстройства питания у детей Наследственные заболевания человека
Наследственные заболевания человека Геморрагический шок
Геморрагический шок Гипогликемическая и гипергликемическая комы
Гипогликемическая и гипергликемическая комы Пути введения лекарственных средств
Пути введения лекарственных средств Обзор и принципы реанимации новорожденных
Обзор и принципы реанимации новорожденных Современные алгоритмы лечения сахарного диабета 2 типа
Современные алгоритмы лечения сахарного диабета 2 типа Нейропсихологическая диагностика
Нейропсихологическая диагностика Общая характеристика группы инфекционных болезней с воздушнокапельным механизмом передачи. Грипп
Общая характеристика группы инфекционных болезней с воздушнокапельным механизмом передачи. Грипп Вагинальные инфекции при беременности
Вагинальные инфекции при беременности Federal State Educational Institution of Higher Education
Federal State Educational Institution of Higher Education Синдром наличия жидкости и газа в плевральной полости. Плевриты
Синдром наличия жидкости и газа в плевральной полости. Плевриты Холера. Эпидемиология
Холера. Эпидемиология Хронический пылевой бронхит
Хронический пылевой бронхит Легочное сердце
Легочное сердце Инфекционный мононуклеоз у детей
Инфекционный мононуклеоз у детей Понятие гиподинамии, гипердинамии
Понятие гиподинамии, гипердинамии Действия ассистента, осуществляемые до прихода врача-стоматолога, после прихода врача-стоматолога и после окончания лечения
Действия ассистента, осуществляемые до прихода врача-стоматолога, после прихода врача-стоматолога и после окончания лечения Митральные пороки сердца
Митральные пороки сердца Критерии и качества стоматологических материалов. Система международных и национальных стандартов
Критерии и качества стоматологических материалов. Система международных и национальных стандартов Введение в венерологию. История развития венерологии. Инфекции, передающиеся половым путем
Введение в венерологию. История развития венерологии. Инфекции, передающиеся половым путем Доказательная профилактика. Скрининговые программы
Доказательная профилактика. Скрининговые программы Endocrine system
Endocrine system Современные подходы к лечению эндометриоидных кист яичников
Современные подходы к лечению эндометриоидных кист яичников Дисфункционалдық жатырдан қан кету
Дисфункционалдық жатырдан қан кету