Содержание
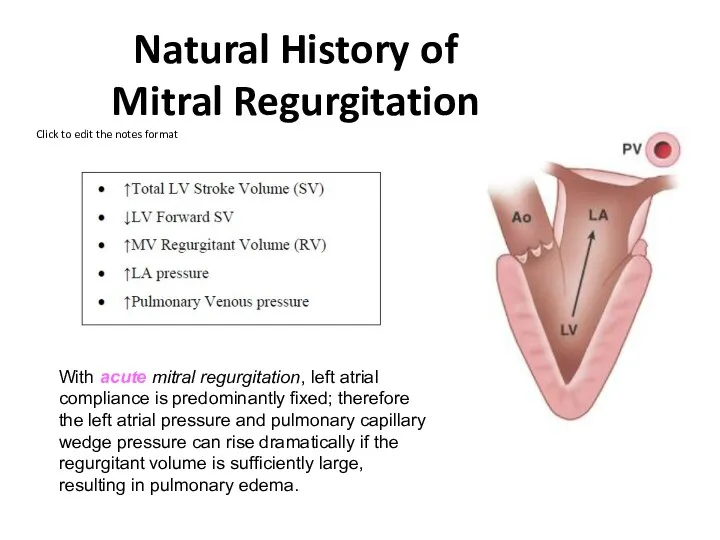
- 37. Natural History of Mitral Regurgitation With acute mitral regurgitation, left atrial compliance is predominantly fixed; therefore
- 38. Chronic Mitral Regurgitation Patients with chronic mitral regurgitation will have a long latent period before becoming
- 39. Mitral Regurgitation hemodynamics In patients with significant mitral regurgitation, prominent v-waves are seen on the left
- 40. Symptoms Fatigue & weakness – due to ? CO – predominant complaint Exertional dyspnea & cough
- 41. Sings Atrial fibrillation Cardiomegally Apical pansystolic murmur +/- thrill Soft S1, apical S3 Signs of pulmonary
- 42. escardio.org 2017
- 43. Rick A. Nishimura et al. Circulation. 2014;129:2440-2492
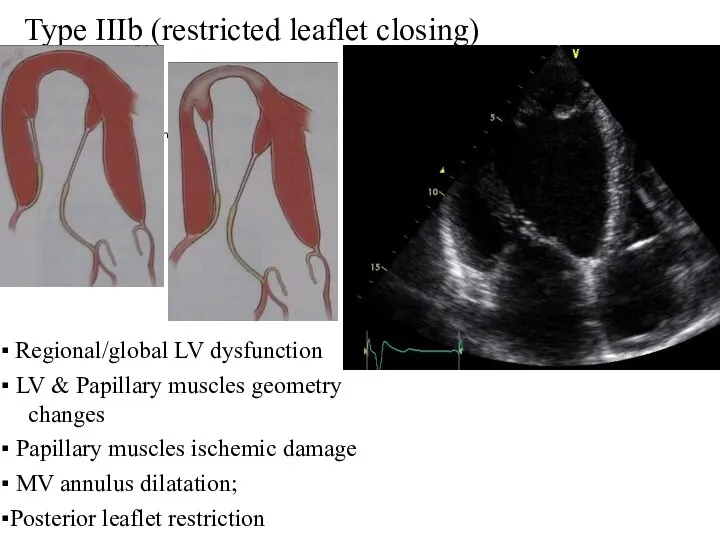
- 45. Type IIIb (restricted leaflet closing) ▪ Regional/global LV dysfunction ▪ LV & Papillary muscles geometry changes
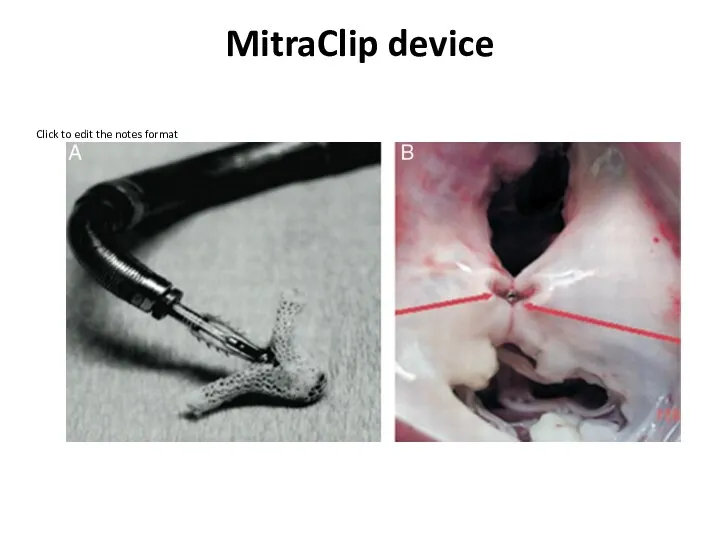
- 46. MitraClip device
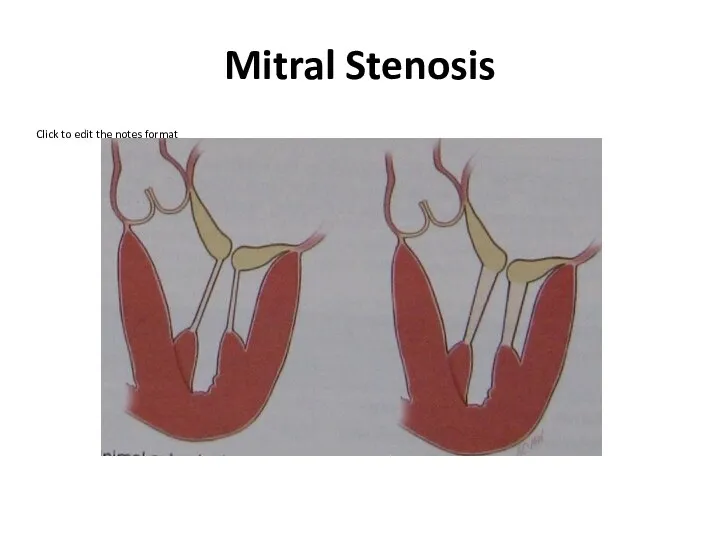
- 49. Mitral Stenosis
- 50. Mitral Stenosis Etiologies: Rheumatic valvular disease - the most common cause of mitral stenosis. Congenital deformities
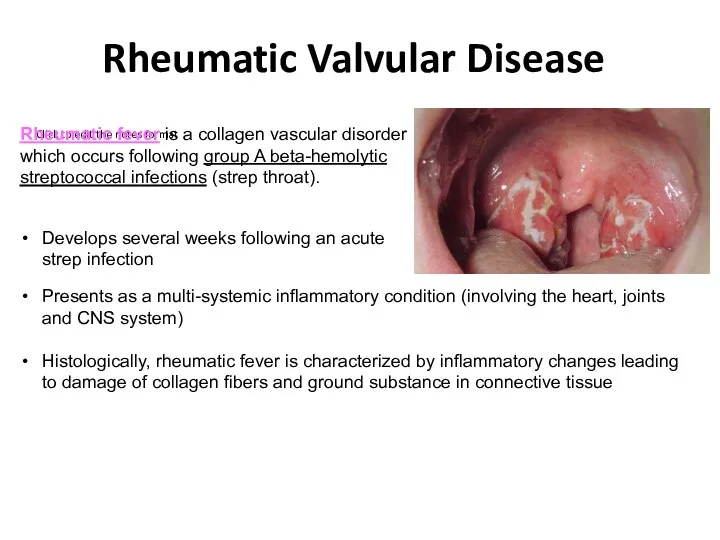
- 51. Rheumatic Valvular Disease Rheumatic fever is a collagen vascular disorder which occurs following group A beta-hemolytic
- 52. Rheumatic Mitral Stenosis
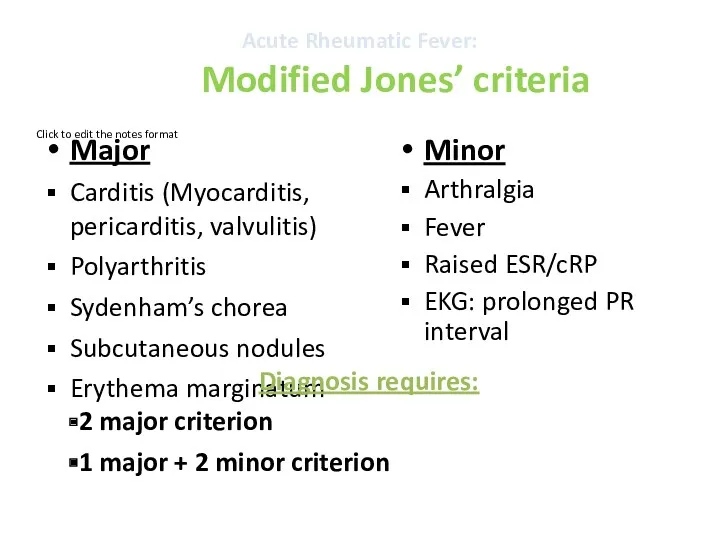
- 53. Acute Rheumatic Fever: Modified Jones’ criteria Major Carditis (Myocarditis, pericarditis, valvulitis) Polyarthritis Sydenham’s chorea Subcutaneous nodules
- 54. Acute Rheumatic Fever: Presentation
- 55. Acute Rheumatic Fever: Some clinical signs Erythema marginatum
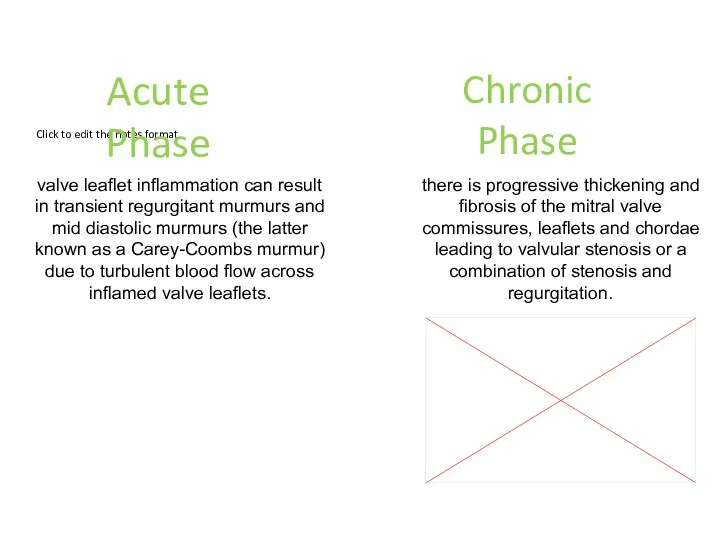
- 56. Acute Phase Chronic Phase valve leaflet inflammation can result in transient regurgitant murmurs and mid diastolic
- 57. Mitral Valve Stenosis: Sings Palpation: Small volume pulse Tapping apex-palpable S1 Palpable S2 Atrial fibrillation Signs
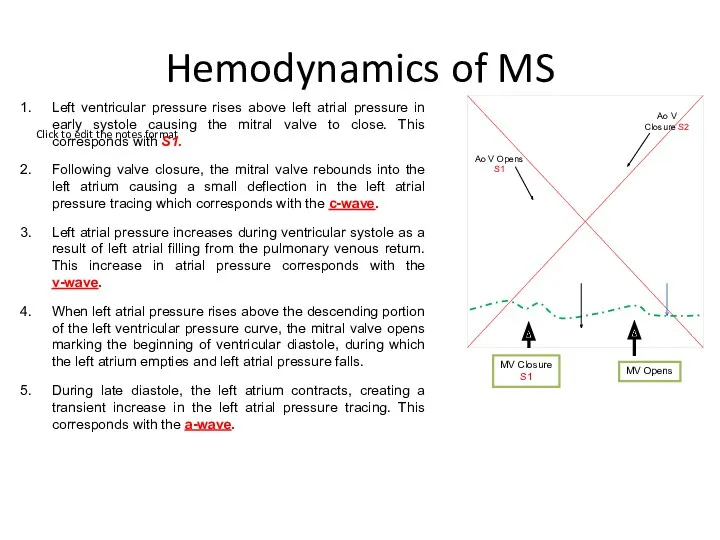
- 58. Hemodynamics of MS Left ventricular pressure rises above left atrial pressure in early systole causing the
- 59. Mitral Valve Stenosis HEMODYNAMICS
- 60. What is the impact of chronic elevation in left atrial pressures on the remainder of the
- 61. With mitral stenosis, there is impedance to left atrial emptying. Left atrial pressure rises to maintain
- 62. With ongoing passive congestion, reactive vasoconstriction occurs in the pre-capillary beds (“pre-capillary block") causing additional increases
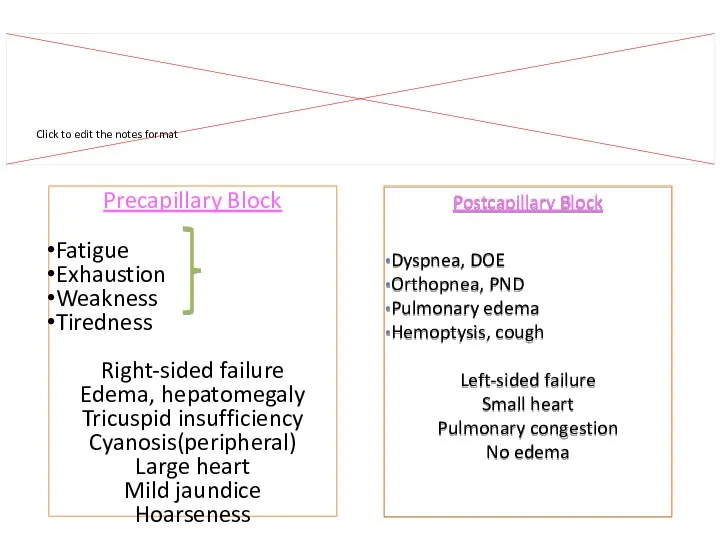
- 63. Precapillary Block Fatigue Exhaustion Weakness Tiredness Right-sided failure Edema, hepatomegaly Tricuspid insufficiency Cyanosis(peripheral) Large heart Mild
- 64. With ongoing passive congestion, reactive vasoconstriction occurs in the pre-capillary beds (“pre-capillary block") causing additional increases
- 65. Mitral Valve Stenosis: Symptoms Dyspnea and cough (pulmonary vascular congestion and pulmonary hypertension) Orthopnea (related to
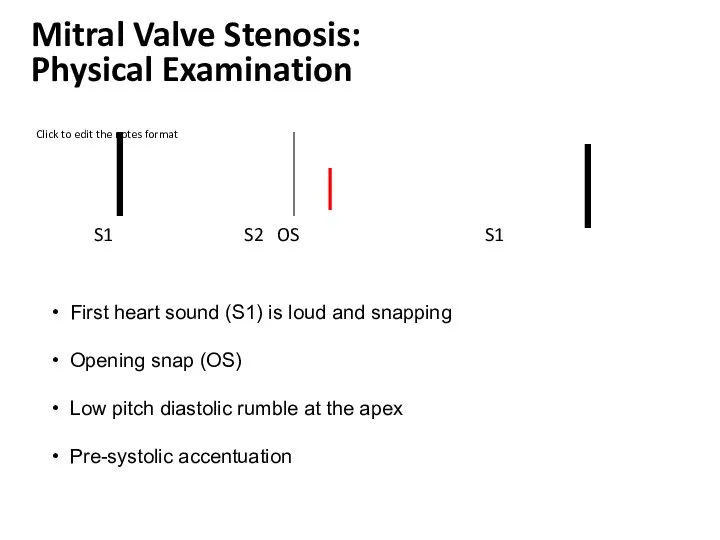
- 66. Auscultatory findings With a structurally normal mitral valve, there is no significant LA to LV diastolic
- 67. With mild mitral stenosis, left atrial pressure is elevated creating a LA to LV pressure gradient
- 68. As mitral stenosis increases in severity, left atrial pressure continues to rise to a point where
- 69. S1 S2 OS S1 First heart sound (S1) is loud and snapping Opening snap (OS) Low
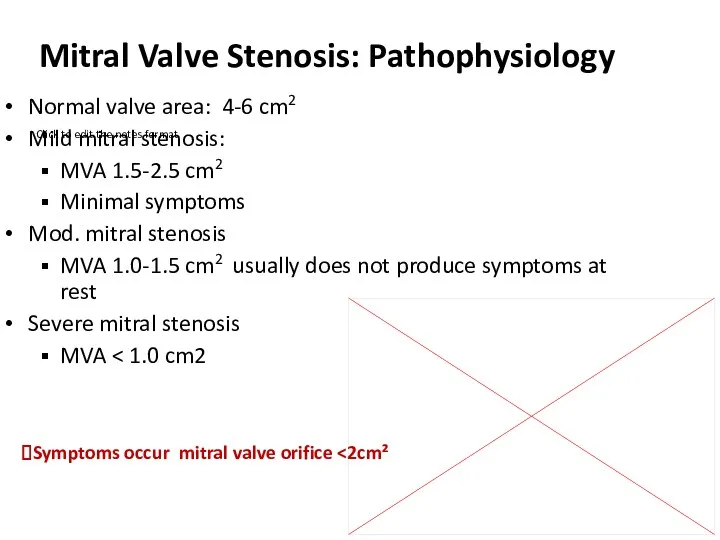
- 70. Mitral Valve Stenosis: Pathophysiology Normal valve area: 4-6 cm2 Mild mitral stenosis: MVA 1.5-2.5 cm2 Minimal
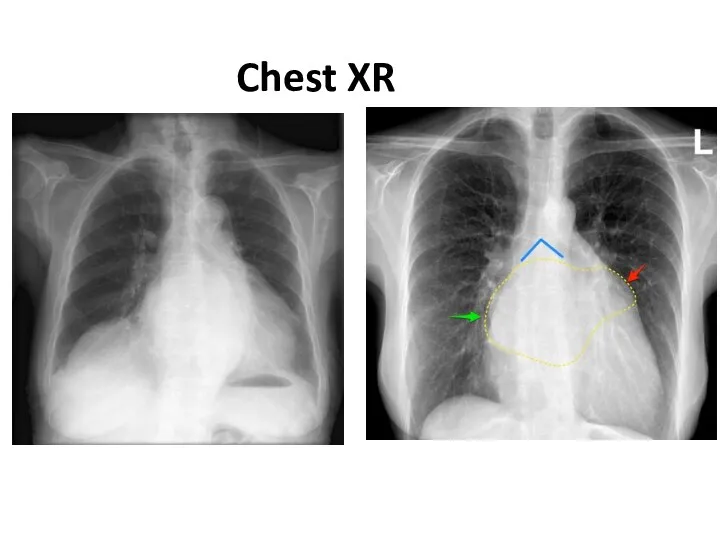
- 71. Chest XR
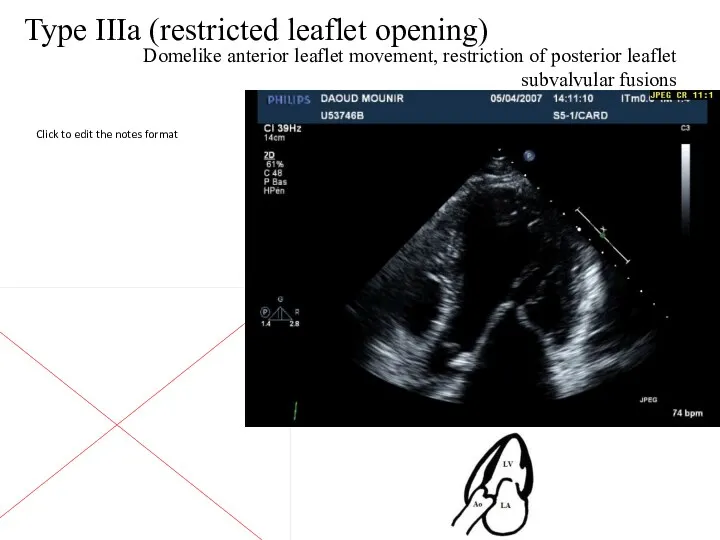
- 72. Type IIIa (restricted leaflet opening) Domelike anterior leaflet movement, restriction of posterior leaflet subvalvular fusions
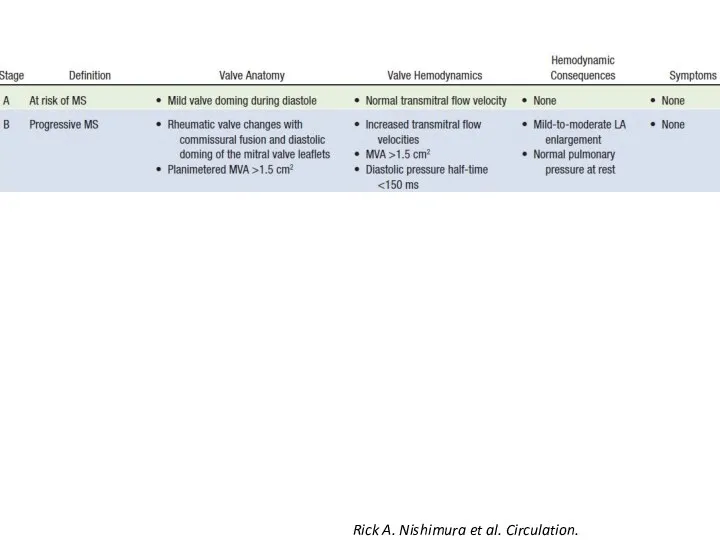
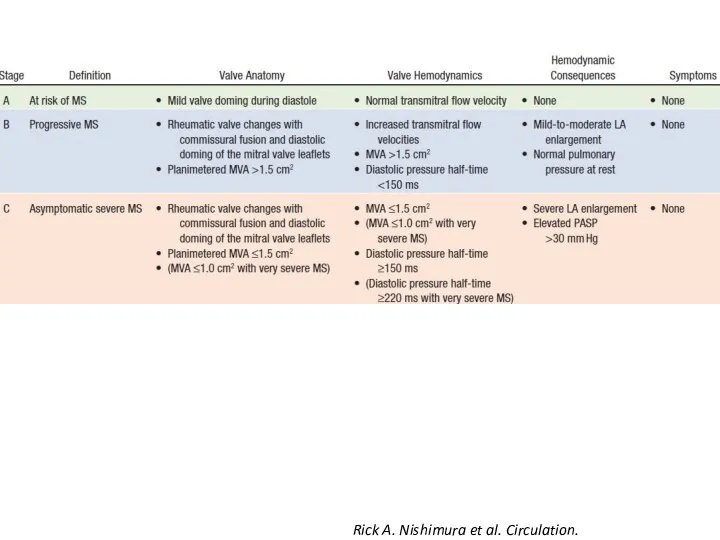
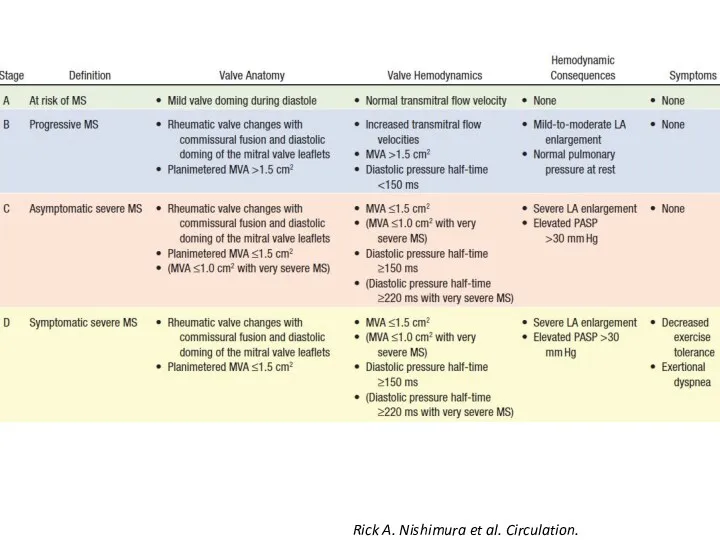
- 73. Rick A. Nishimura et al. Circulation. 2014;129:2440-2492
- 74. Rick A. Nishimura et al. Circulation. 2014;129:2440-2492
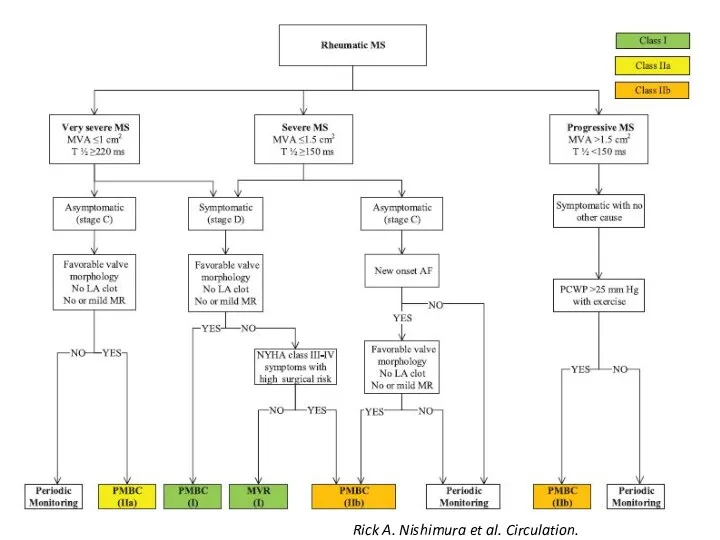
- 75. Rick A. Nishimura et al. Circulation. 2014;129:2440-2492
- 76. Rick A. Nishimura et al. Circulation. 2014;129:2440-2492
- 77. Percutaneous balloon valvuloplasty Carpentier A. “Reconstructive valve surgery” 2010
- 78. Percutaneous balloon valvuloplasty
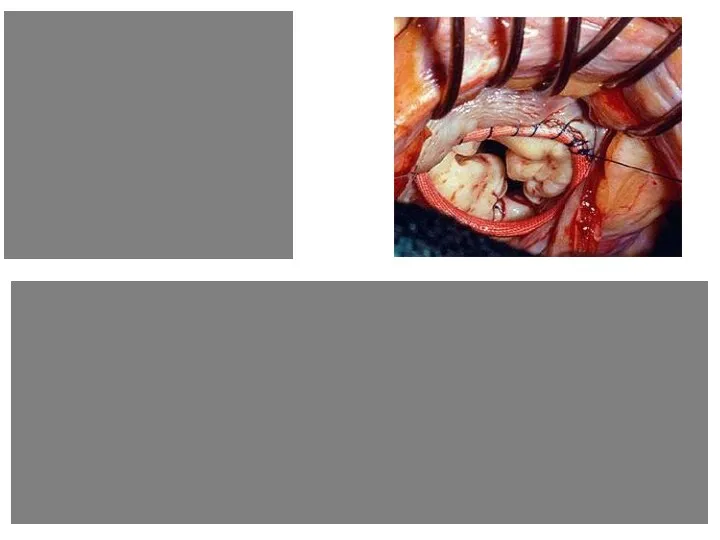
- 79. Mitral Valve Repair Carpentier A. “Reconstructive valve surgery” 2010
- 81. Скачать презентацию



 Способы восстановления дефектов кожи
Способы восстановления дефектов кожи Ревматоидный артрит
Ревматоидный артрит Причины, клинические проявления проблем пациентов детского возраста при наследственных и врожденных заболеваниях
Причины, клинические проявления проблем пациентов детского возраста при наследственных и врожденных заболеваниях Апаттар медицинасын ұйымдастыру принциптері
Апаттар медицинасын ұйымдастыру принциптері Особенности ЭКГ у детей
Особенности ЭКГ у детей Анатомо-физиологические механизмы речи
Анатомо-физиологические механизмы речи Лучевые поражения в результате общего облучения
Лучевые поражения в результате общего облучения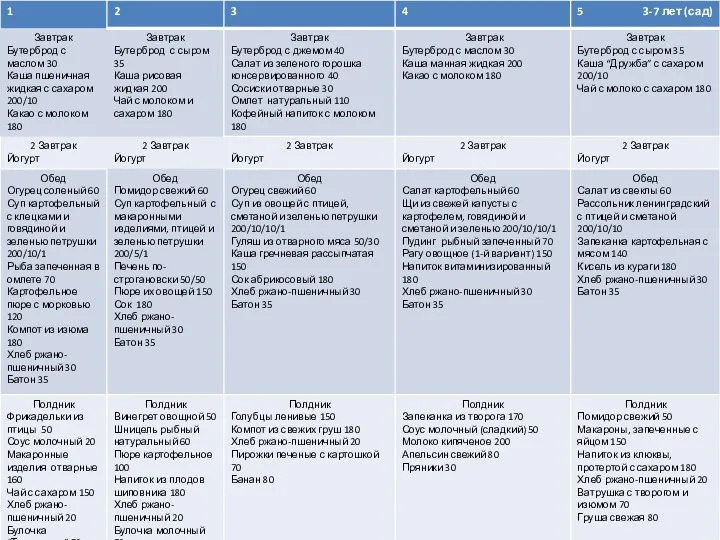 Меню 3-7 лет(сад)
Меню 3-7 лет(сад) Esophagus stomach
Esophagus stomach Клинико-фармакологические подходы к выбору лекарственных средств, применяемых для лечения сердечной недостаточности
Клинико-фармакологические подходы к выбору лекарственных средств, применяемых для лечения сердечной недостаточности Патология последа. Часть I
Патология последа. Часть I Микропрепараты. Патологическая анатомия
Микропрепараты. Патологическая анатомия Неходжкинские лимфомы у ВИЧ-инфицированных больных
Неходжкинские лимфомы у ВИЧ-инфицированных больных Этиология и патогенез туберкулеза
Этиология и патогенез туберкулеза Дифференциальная диагностика при гепато-лиенальном синдроме
Дифференциальная диагностика при гепато-лиенальном синдроме Роль общей лечебной сети в выявлении и профилактике туберкулеза
Роль общей лечебной сети в выявлении и профилактике туберкулеза Анемия и беременность
Анемия и беременность Ханс Бийлсма. Актуальные вопросы ревматологии
Ханс Бийлсма. Актуальные вопросы ревматологии Диагностика и лечение болезни Гиршпрунга у новорожденных
Диагностика и лечение болезни Гиршпрунга у новорожденных Врожденные аномалии
Врожденные аномалии Электроэнцефалография (қысқаша ЭЭГ)
Электроэнцефалография (қысқаша ЭЭГ) Сестринский процесс. Документация к сестринскому процессу. 2018 г
Сестринский процесс. Документация к сестринскому процессу. 2018 г Острые экзогенные интоксикации
Острые экзогенные интоксикации Хронические гепатиты у детей
Хронические гепатиты у детей Ісікке қарсы иммунитет. Вакцинды профилактика негіздері
Ісікке қарсы иммунитет. Вакцинды профилактика негіздері Рак шейки матки у беременных женщин
Рак шейки матки у беременных женщин Heart disease
Heart disease Аборт – экстренная контрацепция или убийство?
Аборт – экстренная контрацепция или убийство?