Содержание
- 2. Chemical control of breathing alveolar pO2 and pCO2 need to be kept constant rises in pCO2
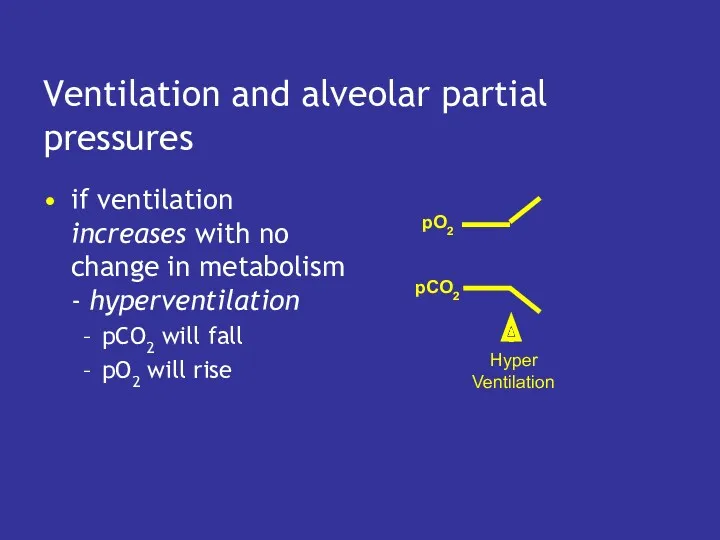
- 3. Ventilation and alveolar partial pressures if ventilation increases with no change in metabolism - hyperventilation pCO2
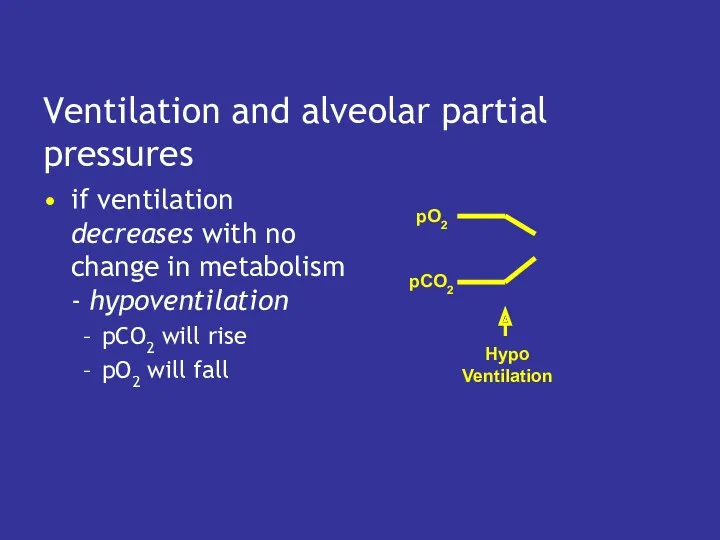
- 4. Ventilation and alveolar partial pressures if ventilation decreases with no change in metabolism - hypoventilation pCO2
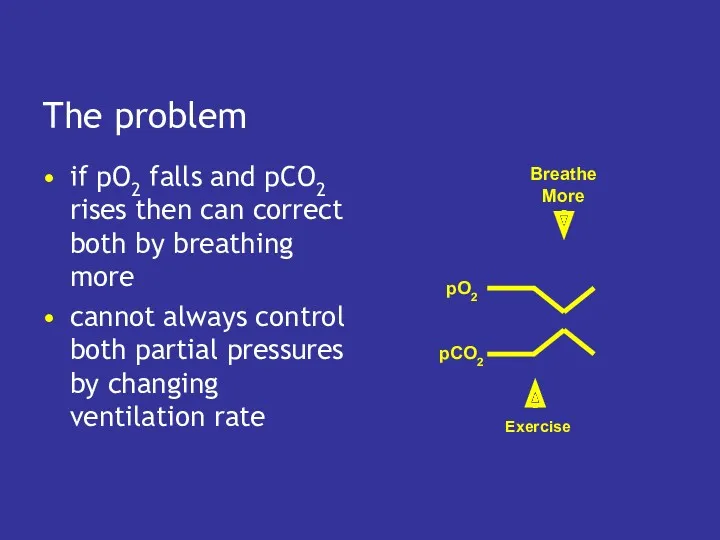
- 5. The problem if pO2 falls and pCO2 rises then can correct both by breathing more cannot
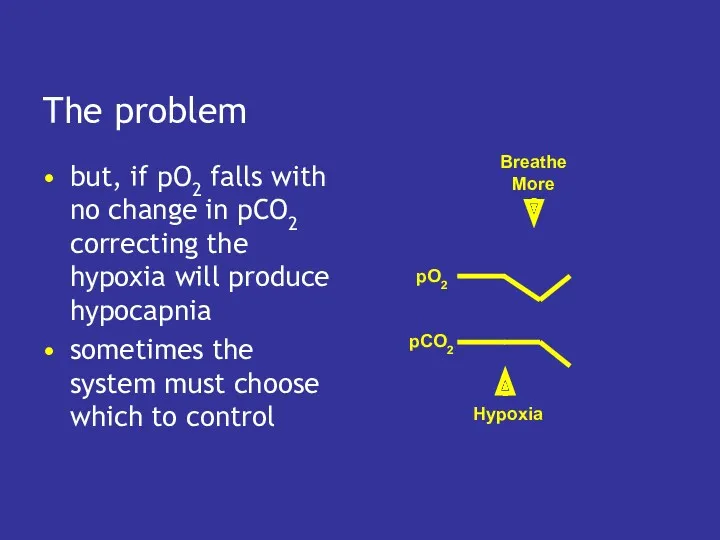
- 6. The problem but, if pO2 falls with no change in pCO2 correcting the hypoxia will produce
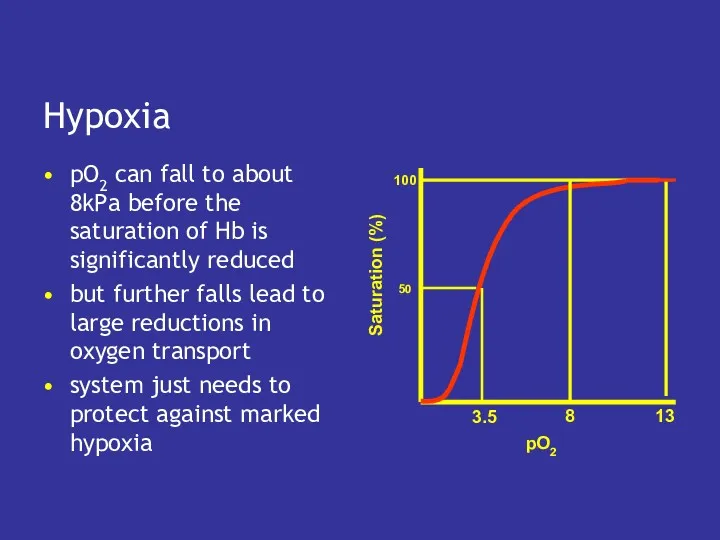
- 7. Hypoxia pO2 can fall to about 8kPa before the saturation of Hb is significantly reduced but
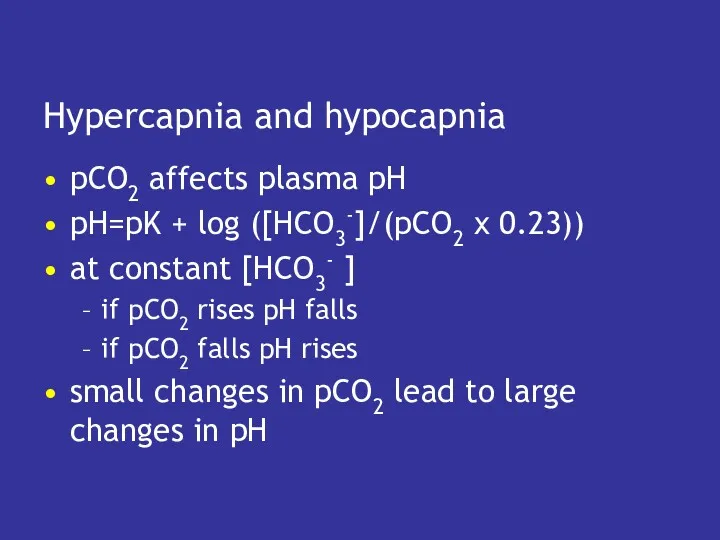
- 8. Hypercapnia and hypocapnia pCO2 affects plasma pH pH=pK + log ([HCO3-]/(pCO2 x 0.23)) at constant [HCO3-
- 9. Effects of acid and alkaline blood if plasma pH falls below 7.0 enzymes lethally denatured if
- 10. Ventilation and acid base balance hypoventilation leads to hypercapnia hypercapnia causes plasma pH to fall this
- 11. Hyperventilation causes pCO2 to fall so pH rises - respiratory alkalosis can cause lethal tetany
- 12. Role of the kidneys plasma pH depends on the ratio of [HCO3-] to pCO2, not on
- 13. Metabolic acid if the tissues produce acid, this reacts with HCO3- the fall in [HCO3-] leads
- 14. Metabolic alkali if plasma [HCO3-] rises (e.g. after vomiting) plasma pH rises metabolic alkalosis can be
- 15. Therefore Plasma pH depends on the ratio of [HCO3-] to pCO2 Respiratory driven changes in pH
- 16. Control of ventilation do not need to control pO2 precisely, but must keep it above 8kPa
- 17. Responses to hypoxia alveolar pO2 must fall a lot to stimulate breathing arterial pO2 monitored by
- 18. Responses to pCO2 peripheral chemoreceptors will detect changes but are rather insensitive central chemoreceptors in the
- 19. Central chemoreceptors detect changes in arterial pCO2 small rises in pCO2 increase ventilation small falls in
- 20. Negative feedback control if pCO2 rises, central chemoreceptors stimulate breathing which blows off CO2, and returns
- 21. Central chemoreceptors actually respond to changes in the pH of cerebro-spinal fluid (CSF) CSF separated from
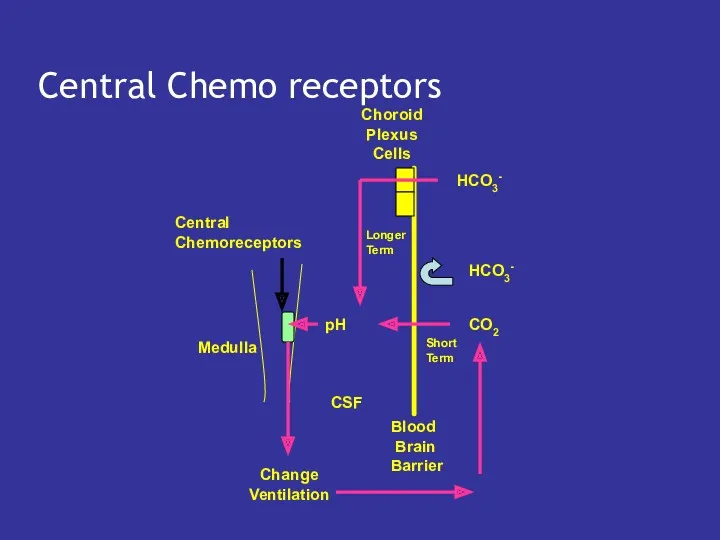
- 22. Central Chemo receptors
- 23. Cerebro-spinal fluid pH determined by ratio of [HCO3-] to pCO2 [HCO3-] fixed in short term so
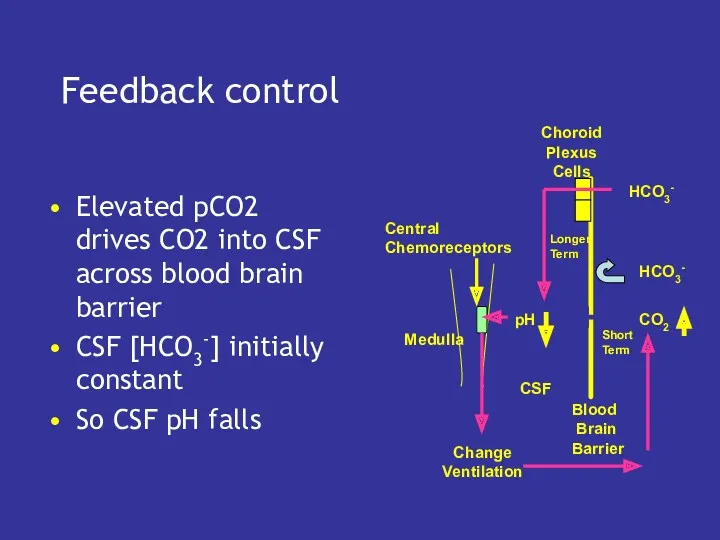
- 24. Feedback control Elevated pCO2 drives CO2 into CSF across blood brain barrier CSF [HCO3-] initially constant
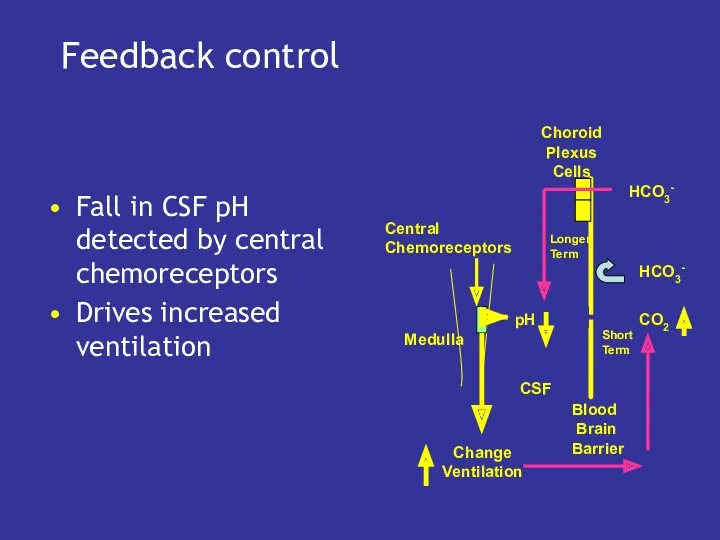
- 25. Feedback control Fall in CSF pH detected by central chemoreceptors Drives increased ventilation pH CO2 HCO3-
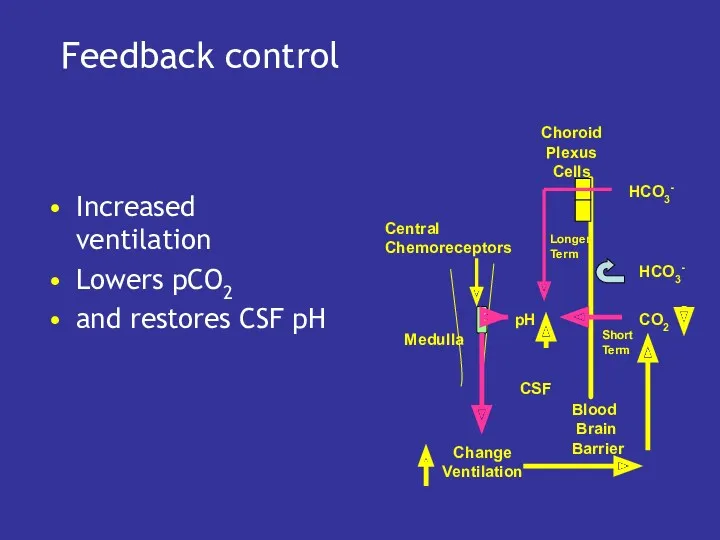
- 26. Feedback control Increased ventilation Lowers pCO2 and restores CSF pH pH CO2 HCO3- HCO3- Blood Brain
- 27. Role of Choroid Plexus CSF [HCO3-] determines which pCO2 is associated with ‘normal’ CSF pH CSF
- 29. Скачать презентацию
![Metabolic alkali if plasma [HCO3-] rises (e.g. after vomiting) plasma](/_ipx/f_webp&q_80&fit_contain&s_1440x1080/imagesDir/jpg/233046/slide-13.jpg)
![Therefore Plasma pH depends on the ratio of [HCO3-] to](/_ipx/f_webp&q_80&fit_contain&s_1440x1080/imagesDir/jpg/233046/slide-14.jpg)
![Cerebro-spinal fluid pH determined by ratio of [HCO3-] to pCO2](/_ipx/f_webp&q_80&fit_contain&s_1440x1080/imagesDir/jpg/233046/slide-22.jpg)
![Role of Choroid Plexus CSF [HCO3-] determines which pCO2 is](/_ipx/f_webp&q_80&fit_contain&s_1440x1080/imagesDir/jpg/233046/slide-26.jpg)
 Классификация, строение и номенклатура органически. Предмет органической химии
Классификация, строение и номенклатура органически. Предмет органической химии Процессы в растворах: электролитическая диссоциация (ЭД)
Процессы в растворах: электролитическая диссоциация (ЭД) Природные источники углеводородов
Природные источники углеводородов Закон сохранения массы веществ. Химические уравнения
Закон сохранения массы веществ. Химические уравнения Александр Евгеньевич Ферсман
Александр Евгеньевич Ферсман Амины
Амины Характеристика химического элемента по его положению в периодической системе элементов Д.И.Менделеева
Характеристика химического элемента по его положению в периодической системе элементов Д.И.Менделеева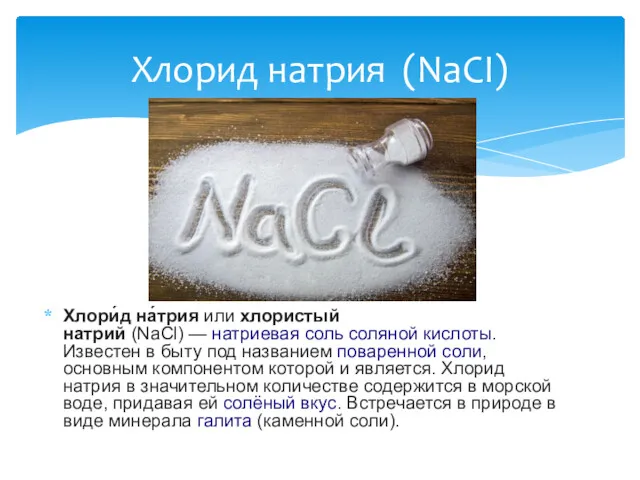 Хлорид натрия (NaCI)
Хлорид натрия (NaCI) Производства аммиака. Лекция 7
Производства аммиака. Лекция 7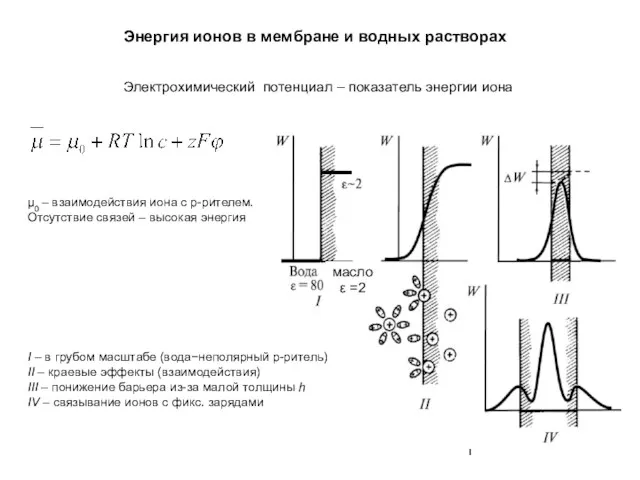 Энергия ионов в мембране и водных растворах
Энергия ионов в мембране и водных растворах Рідкі кристали
Рідкі кристали Железо и его сплавы
Железо и его сплавы Анри Ле Шателье. 1850-1963. Принцип Ле Шателье в химии
Анри Ле Шателье. 1850-1963. Принцип Ле Шателье в химии The Sulphur cycle. The Sulphur dioxide problems
The Sulphur cycle. The Sulphur dioxide problems Спирти. Історична довідка
Спирти. Історична довідка Химия в решении сырьевой проблемы
Химия в решении сырьевой проблемы Аминокислоты. Белки
Аминокислоты. Белки Органическая химия в ряду других наук
Органическая химия в ряду других наук Способы раскисления и модифицирования стали
Способы раскисления и модифицирования стали Топливный элемент
Топливный элемент Химия и косметика
Химия и косметика Гетероциклдік қосылыстар
Гетероциклдік қосылыстар Углепластики
Углепластики Electronică aplicată. (Curs 2)
Electronică aplicată. (Curs 2) Будова електронних оболонок атомів
Будова електронних оболонок атомів Кристаллическое состояние вещества в природе
Кристаллическое состояние вещества в природе Вода на Земле. Строение молекулы воды
Вода на Земле. Строение молекулы воды Метод МО
Метод МО