Содержание
- 2. Isoimmunization - one of the clinical forms imunopatology of pregnancy, provided that there is incompatibility of
- 3. The most frequent: Isoimmunization of Rh-factor; Isoimmunization AB0- system.
- 4. Alloimmune Hemolytic Disease Of The Fetus / Newborn: Definition: Rh-izoimunization - humoral immune response to erythrocytic
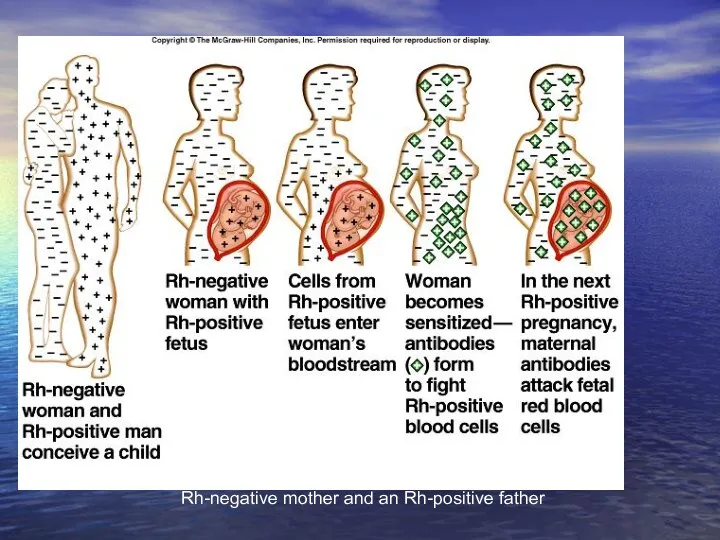
- 5. About 1 in 10 pregnancies involve an Rh-negative mother and an Rh-positive father
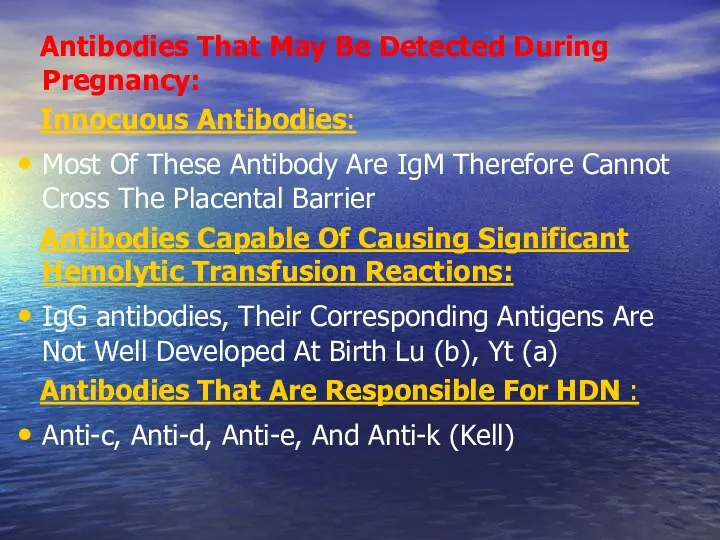
- 6. Antibodies That May Be Detected During Pregnancy: Innocuous Antibodies: Most Of These Antibody Are IgM Therefore
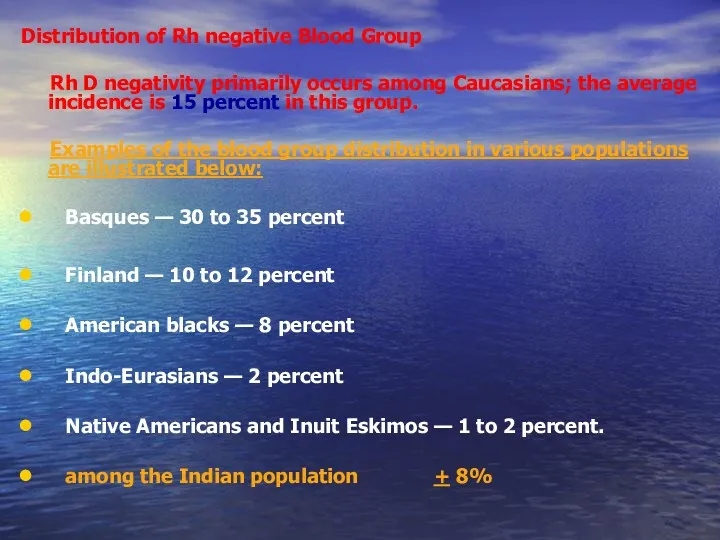
- 7. Distribution of Rh negative Blood Group Rh D negativity primarily occurs among Caucasians; the average incidence
- 8. The main sections of our lectures The RH Antigen – Biochemical and Genetic Aspects Mechanism of
- 9. The RH Antigen – Biochemical and Genetic Aspects
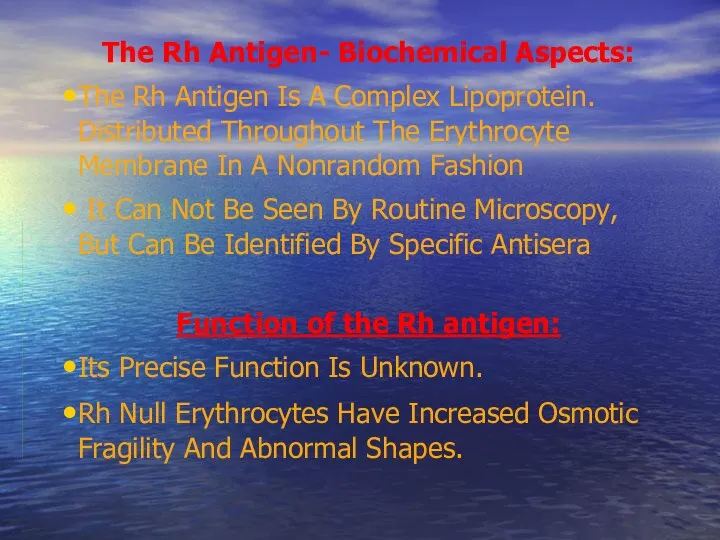
- 10. The Rh Antigen- Biochemical Aspects: The Rh Antigen Is A Complex Lipoprotein. Distributed Throughout The Erythrocyte
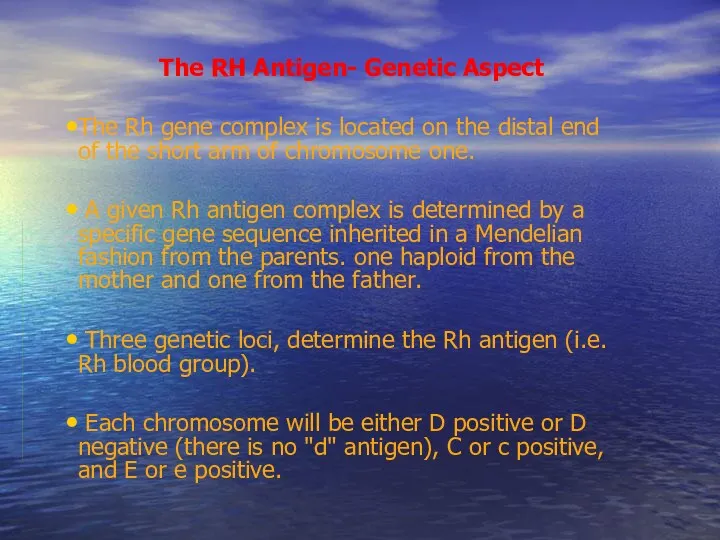
- 11. The RH Antigen- Genetic Aspect The Rh gene complex is located on the distal end of
- 12. Genetic Expression (Rh Surface Protein Antigenicity): Grades Of “Positively” Due To Variation In The Degree Genetic
- 13. Factors Affect The Expression Of The Rh Antigen The Number Of Specific Rh-antigen Sites: - The
- 14. D c E e C d eCd/EcD Phenotype Genotype D positive Antigenicity of the Rh surface
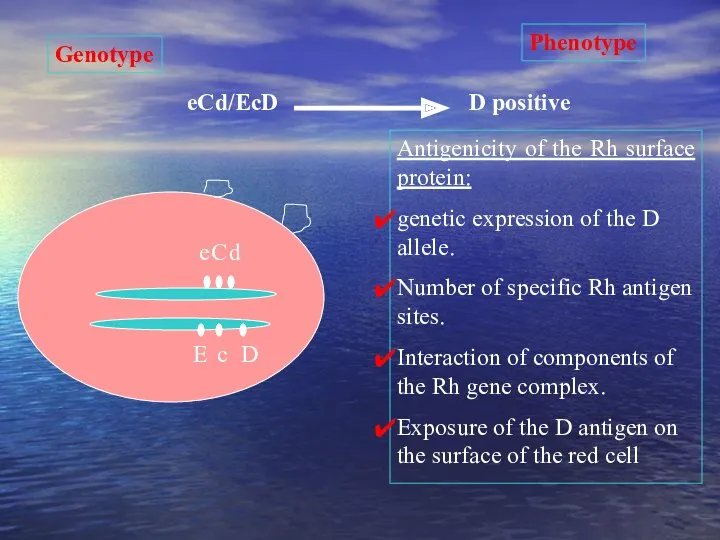
- 15. Mechanism of Development of Maternal Rh Isoimmunization
- 16. FetoMaternal Hemorrhage Sensitization occurs as a result of seepage of fetal cells into maternal circulation as
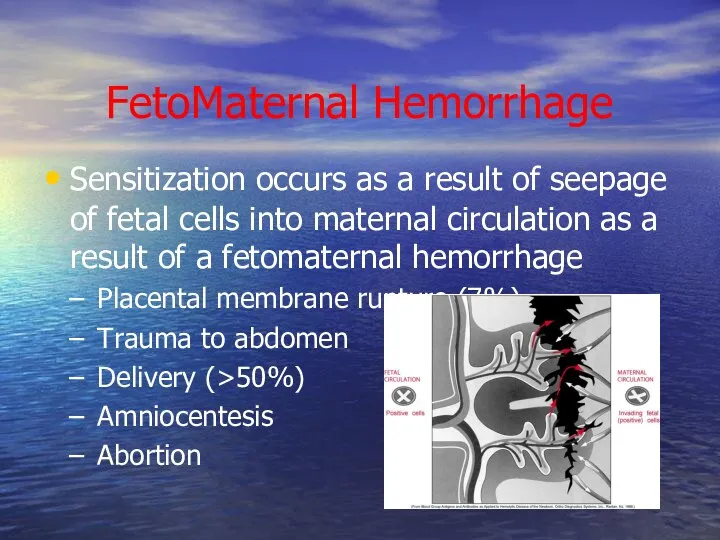
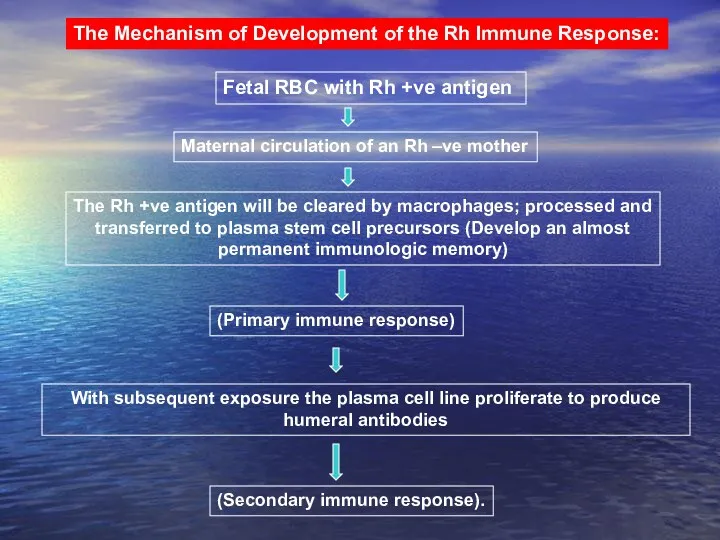
- 17. The Mechanism of Development of the Rh Immune Response: Fetal RBC with Rh +ve antigen Maternal
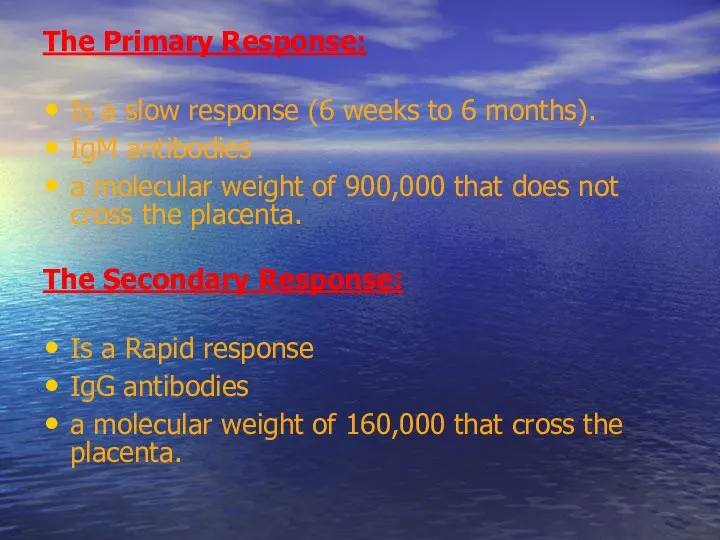
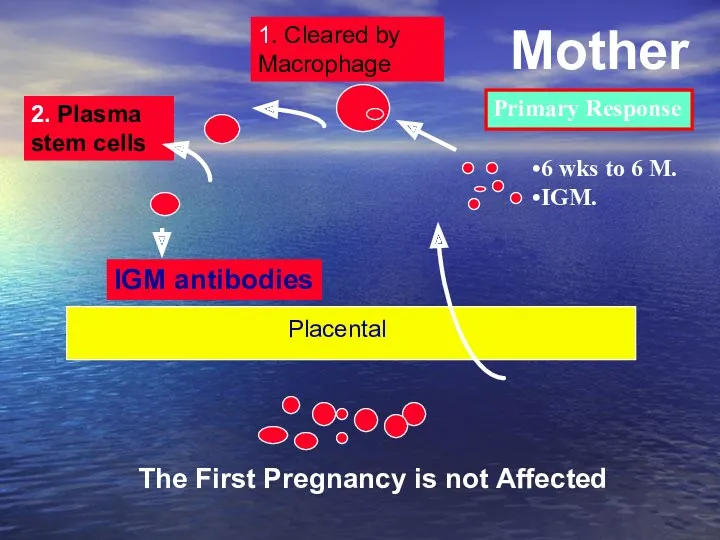
- 18. The Primary Response: Is a slow response (6 weeks to 6 months). IgM antibodies a molecular
- 19. Exposure to maternal antigen in utero “the grandmother theory”: Explains the development of fetal isoimmunization in
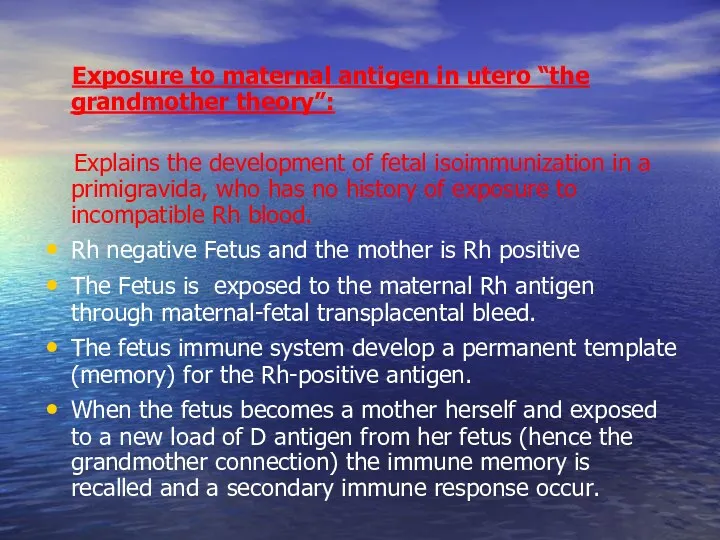
- 20. IGM antibodies 1. Cleared by Macrophage 2. Plasma stem cells The First Pregnancy is not Affected
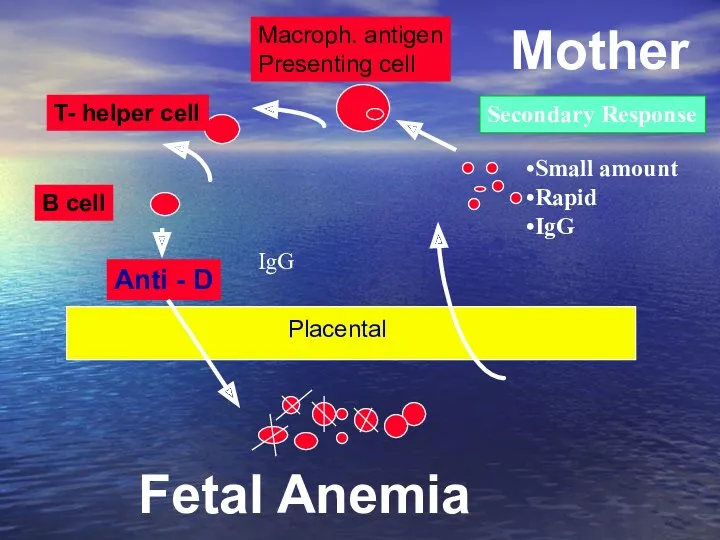
- 21. Anti - D Macroph. antigen Presenting cell T- helper cell B cell Fetal Anemia Mother Placental
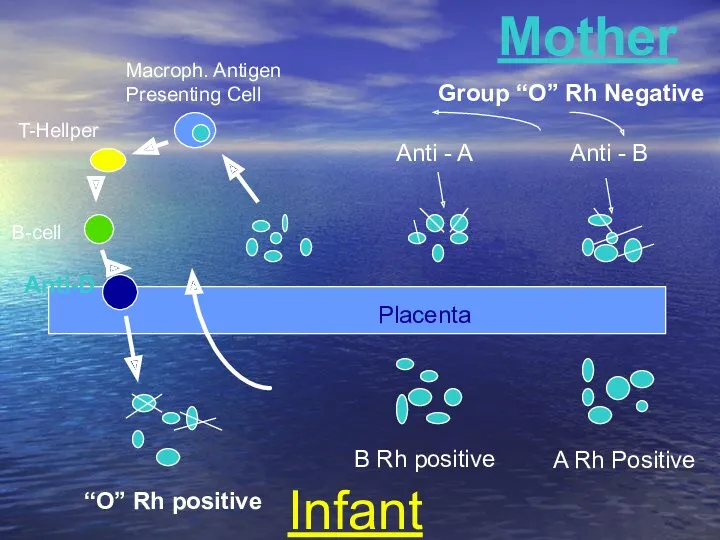
- 22. Macroph. Antigen Presenting Cell T-Hellper B-cell Anti-D Anti - A Anti - B Mother Infant B
- 23. Natural History of Maternal isoimmunization /HD of the Newborn
- 24. Natural History of Rh Isoimmunization And HD Fetus and Newborn Without treatment: less than 20% of
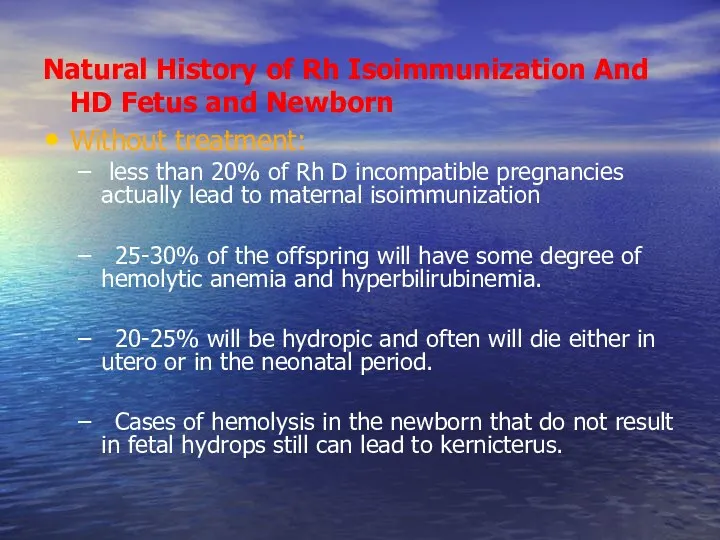
- 25. Kernicterus Kernicterus (bilirubin encephalopathy) results from high levels of indirect bilirubin (>20 mg/dL in a term
- 26. Kernicturus Affected structures have a bright yellow color. Unbound unconjugated bilirubin crosses the blood-brain barrier and,
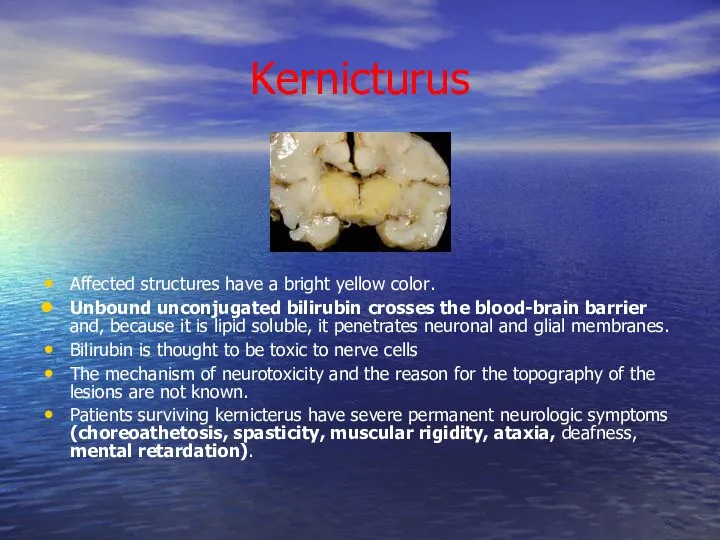
- 27. The Risk of development of Fetal Rh-disease is affected by: Less than 20% of Rh D
- 28. Why Not All the Fetuses of Isoimmunized Women Develop the Same Degree of Disease? Expression Of
- 29. Risk factors: - a history of artificial abortion; - a history of spontaneous abortions; - transfusion
- 30. Pathogenesis of Fetal Erythroblastosis Fetalis
- 31. Pathogenesis When erythroblasts are used up in the bone marrow, erythropoiesis in the spleen and liver
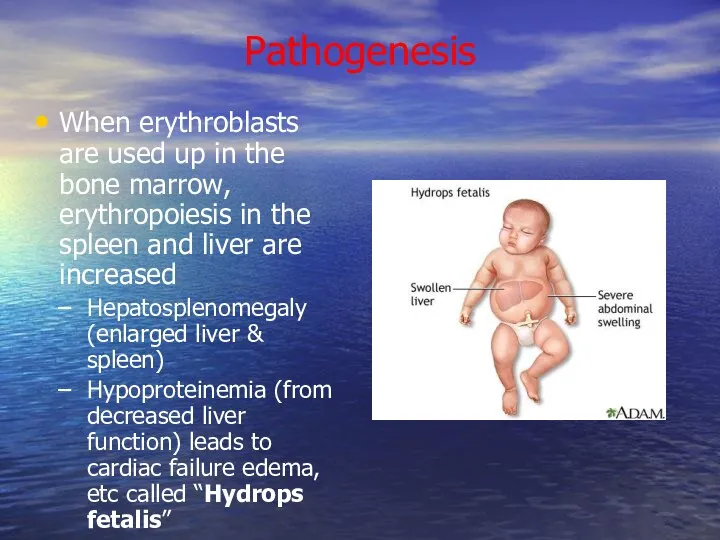
- 32. Bilirubin Hemoglobin is metabolized to bilirubin Before birth, “indirect” bilirubin is transported across placenta and conjugated
- 33. Laboratory Findings Vary with severity of HDN and include: Anemia Hyperbilirubinemia Reticulocytosis (6 to 40%) ↑
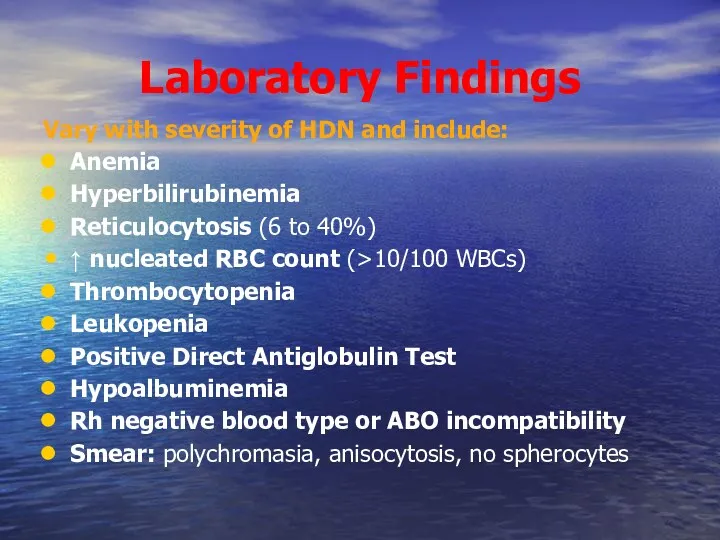
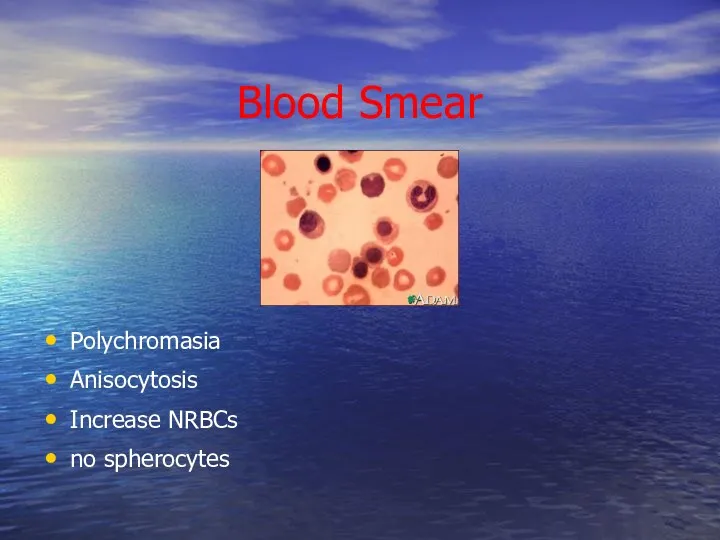
- 34. Blood Smear Polychromasia Anisocytosis Increase NRBCs no spherocytes
- 35. Rh Antibodies Antibodies Coated Red Cells Destruction of Fetal Cells by Fetal RES Fetal Anemia Fetal
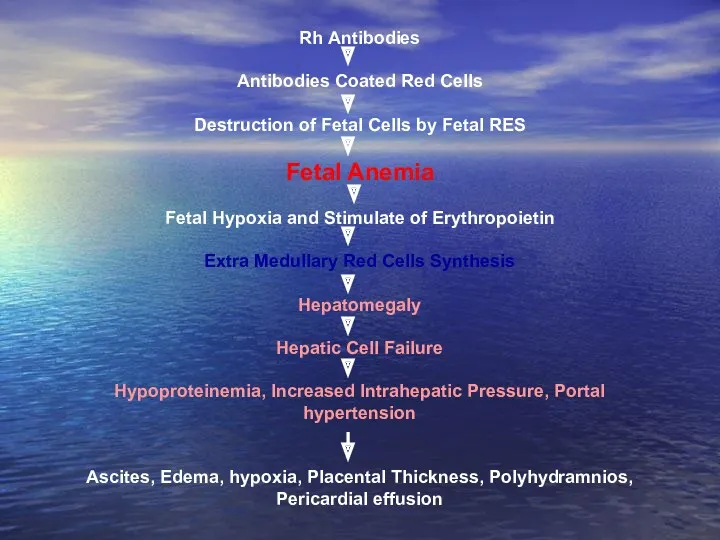
- 36. Complications of Fetal-Neonatal Anemia: Fetal Hydrops And IUFD Hepatosplenomegaly Neonatal Jaundice Compilations Of Neonatal Kernicterus (Lethargy,
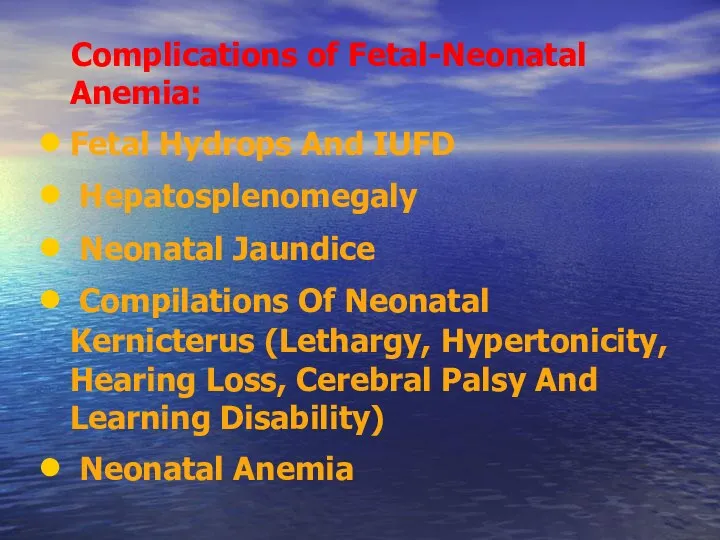
- 37. Hydrops Fetalis
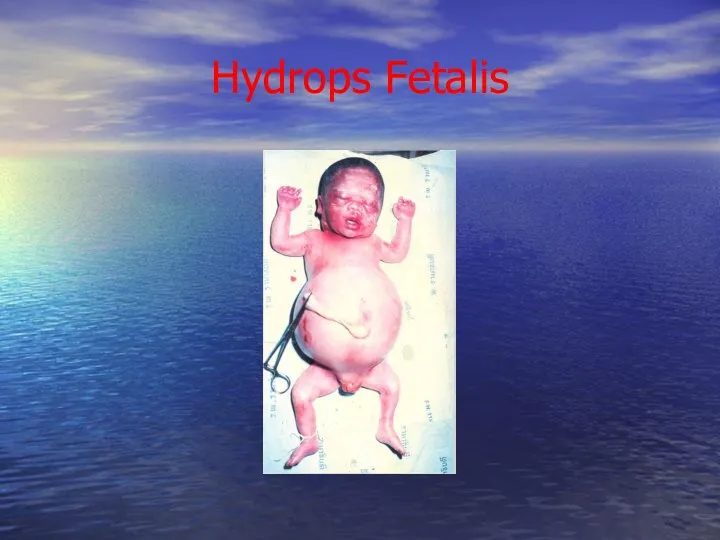
- 38. Management Prevention Treatment:
- 39. Prevention of Rh Isoimmunization
- 40. Prevention of Rh Isoimmunization Prophylaxis during pregnancy in the absence of immunization of pregnant. A by
- 41. Dose of prophylactic Anti-D Ig: In term pregnancy before 13 weeks dose of anti-Rho (D) antibody
- 42. Prevention of postpartum birth Rh-positive child: during the first 72 hours by intramuscular put 1 dose
- 43. Prevention of hypertension in the system AB0 during pregnancy is not performed. Pseudoreaction drug prevention and
- 44. Management of cases of Rh isoimmunization Diagnosis Of RH Isoimmunization Evaluation of Fetal Condition
- 45. Diagnosis of Rh isoimmunization Family history: a blood transfusion without regard to Rh-ownership, abortion, stillbirth or
- 46. Antibody Titre in Saline: RhD-positive cells suspended in saline solution are agglutinated by IgM anti-RhD antibody,
- 47. The Direct Coombs Test Is Done After Birth To Detect The Presence Of Maternal Antibody On
- 48. Fetal Rhesus Determination RHD Type And Zygosity (If RHD-positive) Of The Father Amniocentesis To Determine The
- 49. Management of cases of Rh isoimmunization Diagnosis Of RH Isoimmunization Evaluation of Fetal Condition
- 50. Goals of managing Fetal Alloimmunization: Initially detecting fetal anemia prior to the occurrence of fetal compromise.
- 51. Evaluation of Fetal Condition Measurements Of Antibodies in Maternal Serum Determination of Fetal Rh Blood Group
- 52. Although not reliably accurate in predicting severity of fetal disease, past obstetrical history can be somewhat
- 53. Maternal Anti-D Titer Antibody Titer Is A Screening Test. A Positive Anti-d Titer Means That The
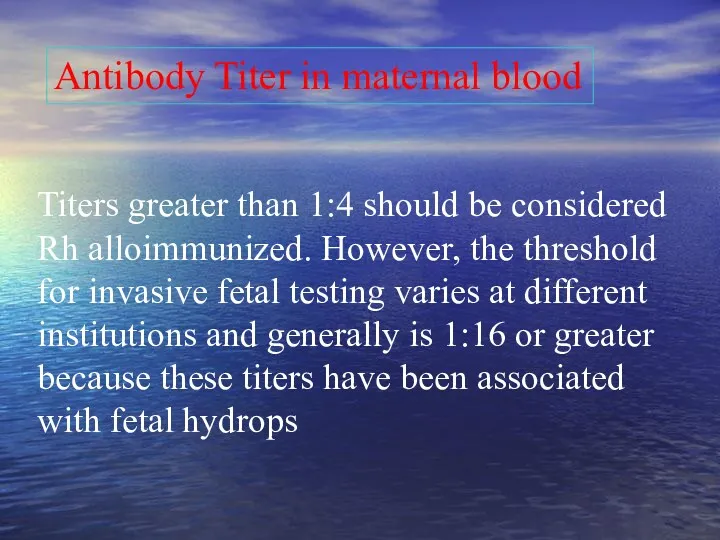
- 54. Ultrasound Image of Transabdominal Chorion Villus Sampling
- 55. To Establish The Correct Gestational Age. In Guiding Invasive Procedures And Monitoring Fetal Growth And Well-being.
- 56. Ultrasound scanning enables to establish the early signs of dropsy fetal dropsy fetal and that developed
- 57. Doppler Velocimetry Of The Fetal Middle Cerebral Artery (MCA) For Predicting Fetal Anemia
- 58. Cardiotocography is showing signs of chronic hypoxia and reduced compensatory ability of the fetoplacental complex.
- 59. Invasive Techniques Amniocentesis Fetal Blood Sampling
- 60. Transabdominal amniocentesis performed in the period after 26 weeks of pregnancy. Questions about the need to
- 61. Studies of amniotic fluid to assess the severity of fetal anemia. In cases of fetal hypertension
- 62. Ultrasound image of amniocentesis at 16 weeks of gestation
- 63. Cordocentesis - taking blood from the umbilical cord through the anterior abdominal wall women. In determining
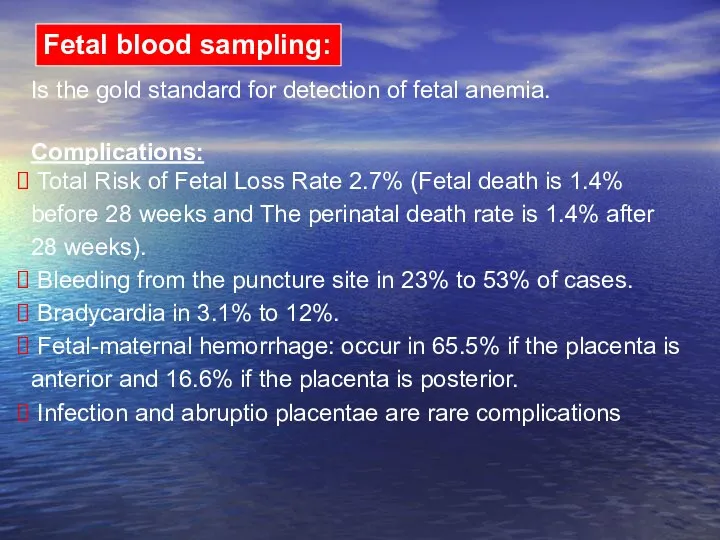
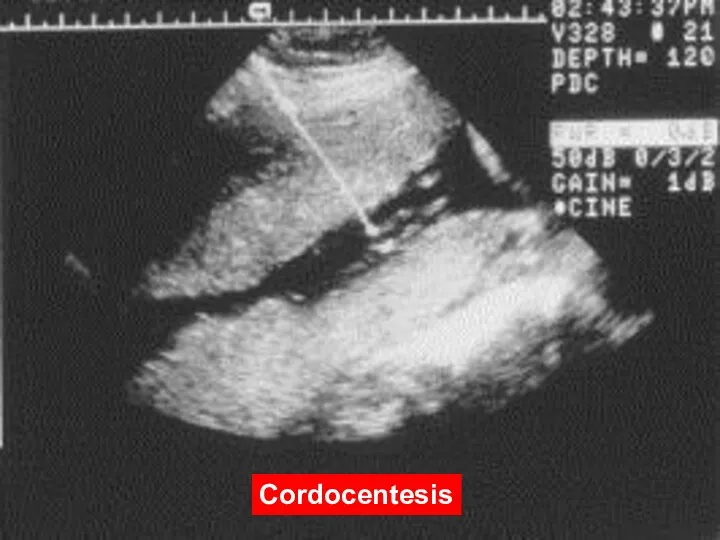
- 64. Is the gold standard for detection of fetal anemia. Complications: Total Risk of Fetal Loss Rate
- 65. Diagram of cordocentesis procedure Cordocentesis
- 66. Cordocentesis
- 67. Suggested management of the RhD-sensitized pregnancy Monthly Maternal Indirect Coombs Titre Below Critical Titre Complicated History
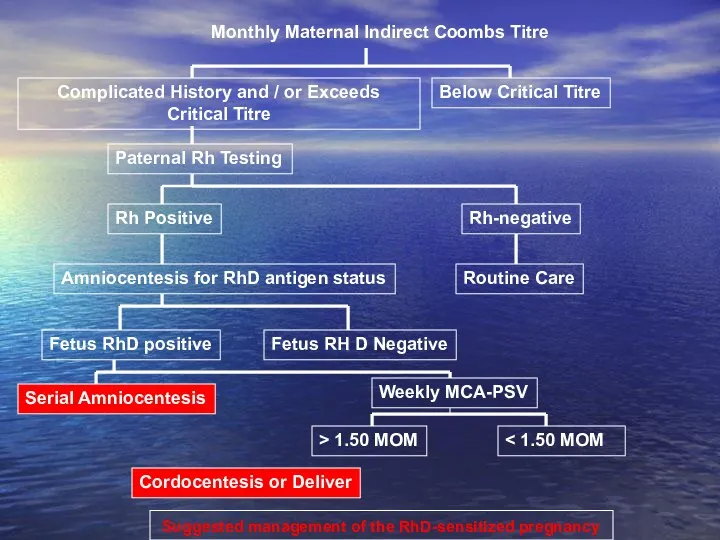
- 68. Titers greater than 1:4 should be considered Rh alloimmunized. However, the threshold for invasive fetal testing
- 69. Indications for early obstetrical complications in Rh-conflict: 1. AB titre equal to or more than 1:64
- 70. Because the wavelength at which bilirubin absorbs light is 420-460 nm, the amount of shift in
- 71. Transcutaneous Monitoring Transcutaneous bilirubinometry can be adopted as the first-line screening tool for jaundice in well,
- 72. TREATMENT Exchange transfusion Phototherapy
- 73. Intrauterine Transfusion (IUT) Given to the fetus to prevent hydrops fetalis and fetal death. Can be
- 74. Intrauterine Transfusion An intrauterine fetal blood transfusion is done in the hospital. The mother may have
- 75. Intrauterine Transfusion Increasingly common and relatively safe procedure since the development of high resolution ultrasound particularly
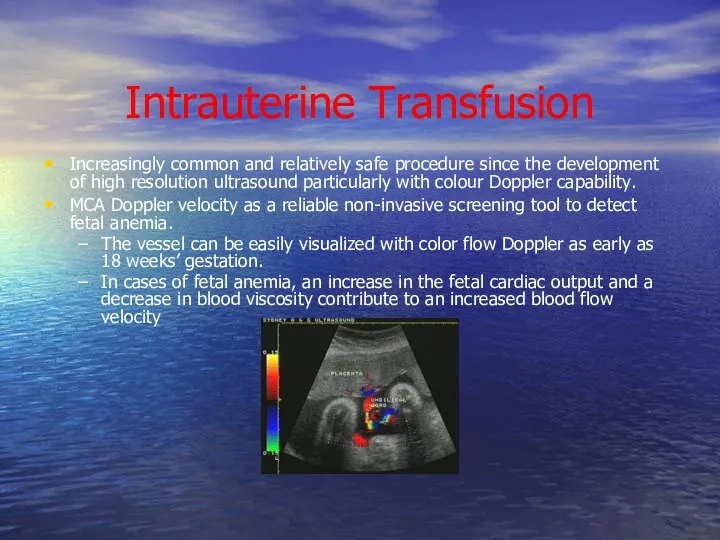
- 76. Intrauterine Transfusion The risk of these procedures is now largely dependent on the prior condition of
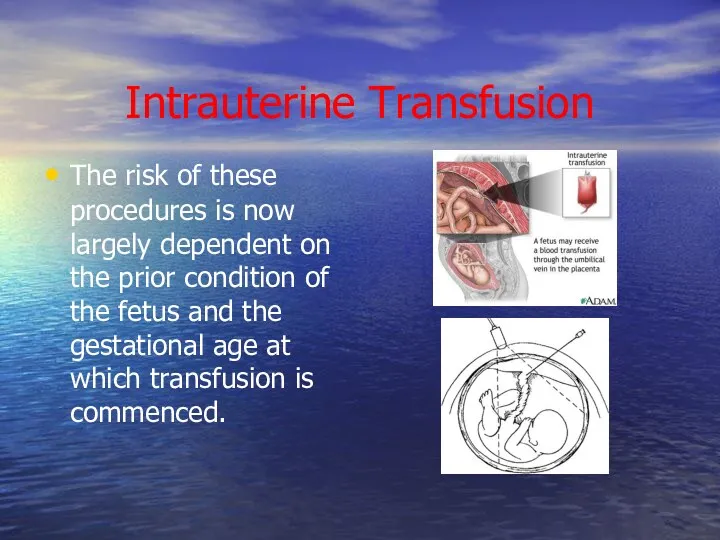
- 77. Treatment of Mild HDN Phototherapy is the treatment of choice. Phototherapy process slowly decomposes/converts bilirubin into
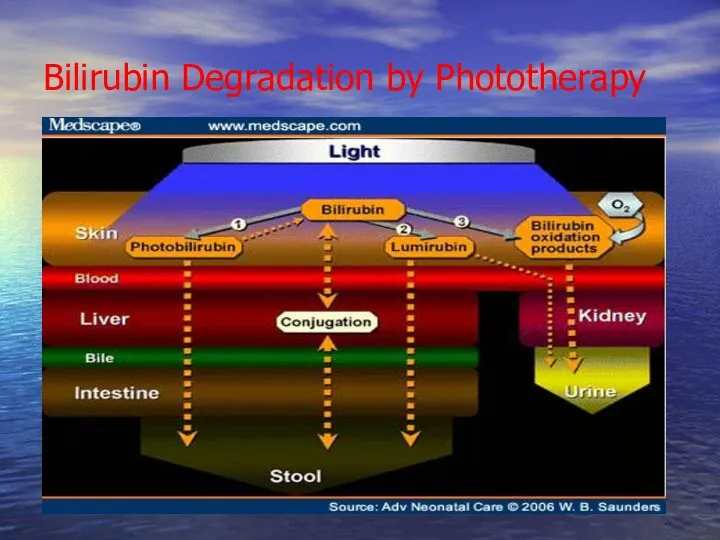
- 78. Bilirubin Degradation by Phototherapy
- 79. Phototherapy The therapy uses a blue light (420-470 nm) that converts bilirubin so that it can
- 80. Exchange Transfusion Full-term infants rarely require an exchange transfusion if intense phototherapy is initiated in a
- 81. Goals of Exchange Transfusion Remove sensitized cells. Reduce level of maternal antibody. Removes about 60 percent
- 83. Скачать презентацию













 Гипертензивные расстройства во время беременности, в родах и послеродовом периоде. Часть 2
Гипертензивные расстройства во время беременности, в родах и послеродовом периоде. Часть 2 Операции в области живота. Абдоминальная хирургия
Операции в области живота. Абдоминальная хирургия влияние комплексных физических упражнений на коррекцию нарушений осанки у детей школьного возраста
влияние комплексных физических упражнений на коррекцию нарушений осанки у детей школьного возраста Острое воспаление. Морфология экссудативного воспаления. (Занятие 7)
Острое воспаление. Морфология экссудативного воспаления. (Занятие 7) Гемофилия. Виды гемофилии
Гемофилия. Виды гемофилии Постстрептококковый гломерулонефрит. Острый гломерулонефрит. Этиология и патогенез. Клинические варианты. Клиника и диагностика
Постстрептококковый гломерулонефрит. Острый гломерулонефрит. Этиология и патогенез. Клинические варианты. Клиника и диагностика Пищевая аллергия у детей
Пищевая аллергия у детей Качество медпомощи в организациях ПМСП
Качество медпомощи в организациях ПМСП Наследственные заболевания лёгких и пороки развития
Наследственные заболевания лёгких и пороки развития Формирование воздушной струи в процессе преодоления нарушений звукопроизношения
Формирование воздушной струи в процессе преодоления нарушений звукопроизношения ВИЧ - инфекция
ВИЧ - инфекция Ядерная медицина
Ядерная медицина Миокардиты: классификация, клиника
Миокардиты: классификация, клиника Анестезиологическое обеспечение обширных ортопедических вмешательств
Анестезиологическое обеспечение обширных ортопедических вмешательств Физиология микроорганизмов. Антибиотики и ХТП
Физиология микроорганизмов. Антибиотики и ХТП !! 378512
!! 378512 Альцгеймер ауруы
Альцгеймер ауруы Кроветворение (гемопоэз)
Кроветворение (гемопоэз) Организмнің сыртқы ортаға бейімделудегі талдағыштар рөлі
Организмнің сыртқы ортаға бейімделудегі талдағыштар рөлі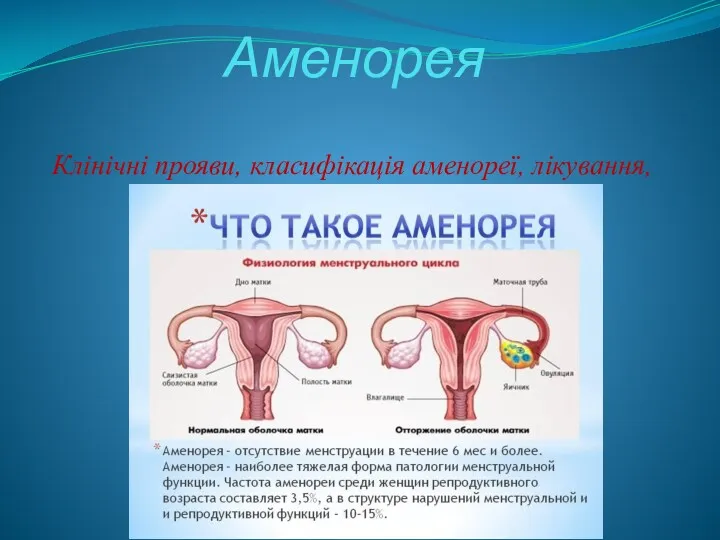 Аменорея. Клінічні прояви
Аменорея. Клінічні прояви Дифференциальный диагноз при аритмиях. Клиническая и ЭКГ-диагностика. Принципы лечения и неотложная помощь
Дифференциальный диагноз при аритмиях. Клиническая и ЭКГ-диагностика. Принципы лечения и неотложная помощь Диссеминированный туберкулез легких
Диссеминированный туберкулез легких Спа-маникюр
Спа-маникюр Защита от клеща. Медицинское страхование Росгосстрах
Защита от клеща. Медицинское страхование Росгосстрах Реографиялық құралдар, жұмыс істеу принциптері
Реографиялық құралдар, жұмыс істеу принциптері r1553706493
r1553706493 Болезнь Альцгеймера (сенильная деменция альцгеймеровского типа)
Болезнь Альцгеймера (сенильная деменция альцгеймеровского типа) Аминогликозиды. Характеристика. Спектр действия
Аминогликозиды. Характеристика. Спектр действия