Содержание
- 2. ETIOLOGY: The infectious agent – leptospira ( F. Spirochaetacea K. Leptospira) also is subdivided on pathogenic
- 5. Optimal conditions of the growth on the medium with addition 5 - 10 % serum of
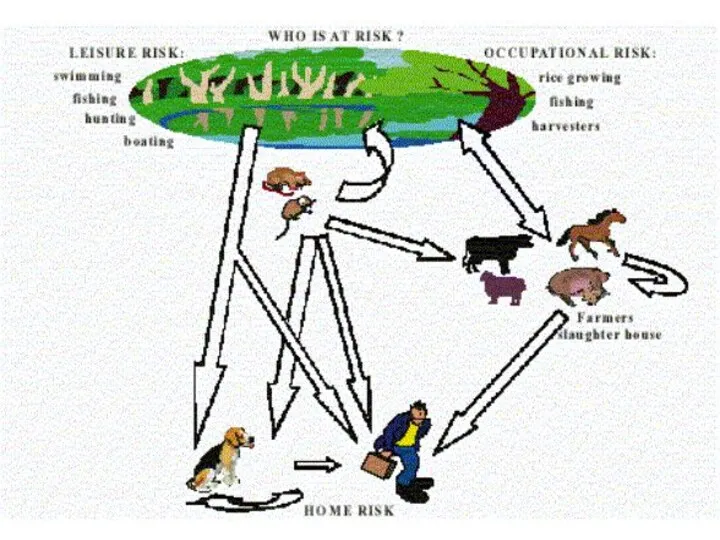
- 6. L. have 2 antigenes: - genuspecific (deep) - and typespecific (surface). During illness will be derivated
- 8. DWELLING-PLACE OF wild small rodents mice, rats hedgehogs ect.)
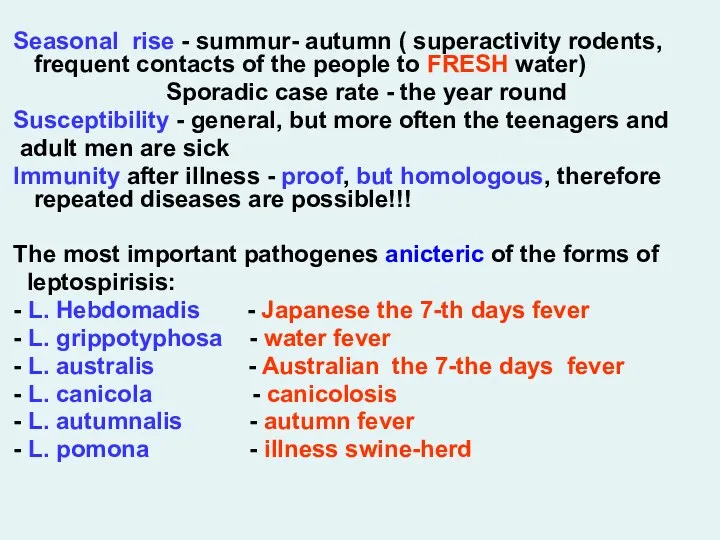
- 10. Seasonal rise - summur- autumn ( superactivity rodents, frequent contacts of the people to FRESH water)
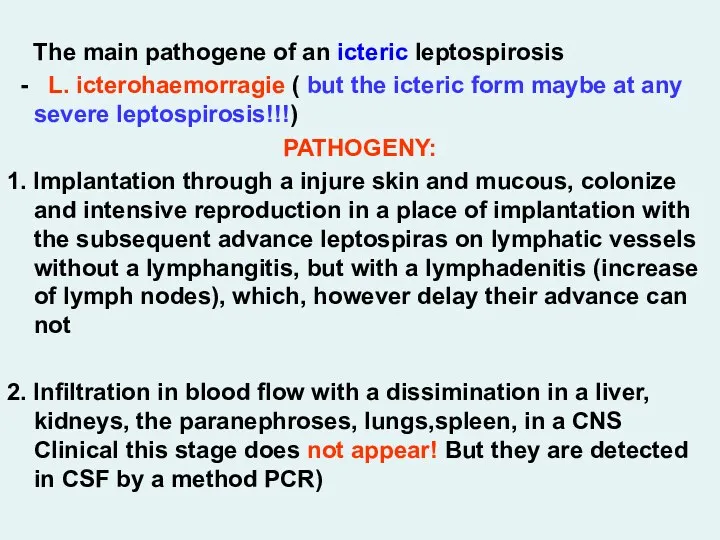
- 11. The main pathogene of an icteric leptospirosis - L. icterohaemorragie ( but the icteric form maybe
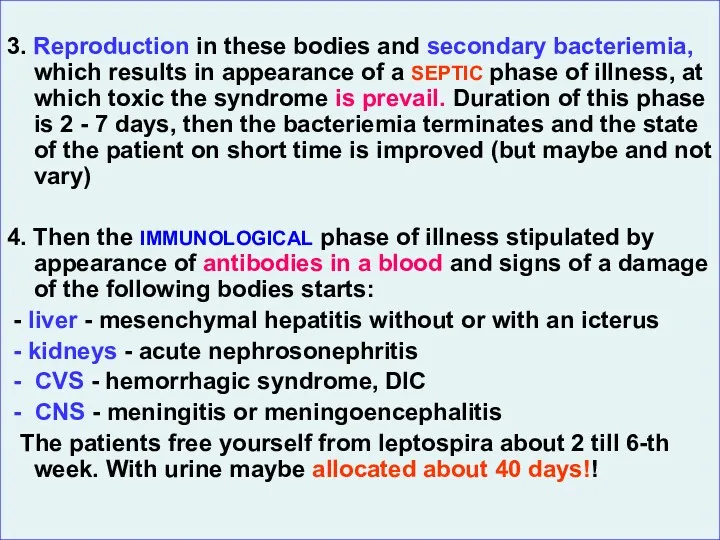
- 12. 3. Reproduction in these bodies and secondary bacteriemia, which results in appearance of a SEPTIC phase
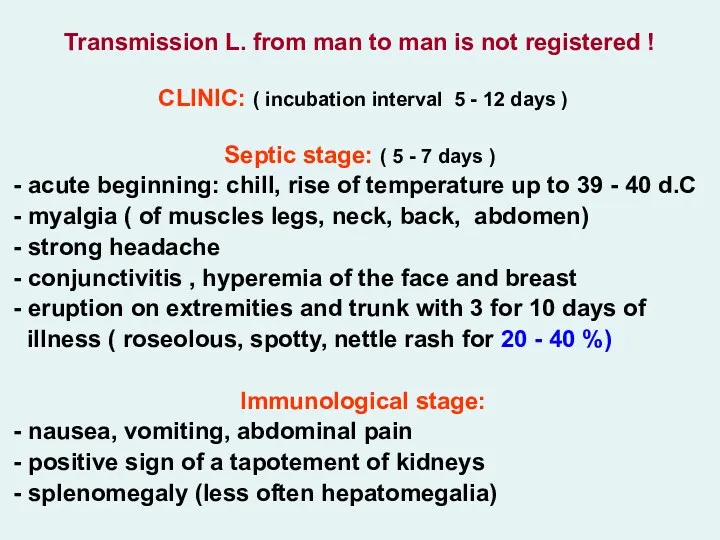
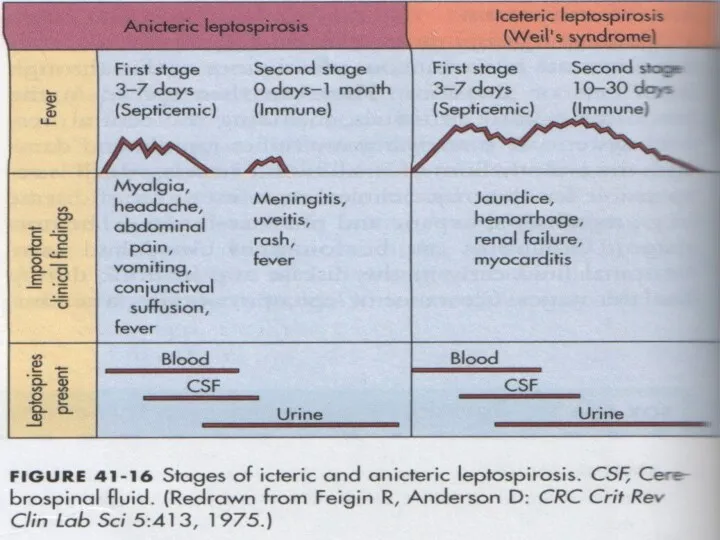
- 14. Transmission L. from man to man is not registered ! CLINIC: ( incubation interval 5 -
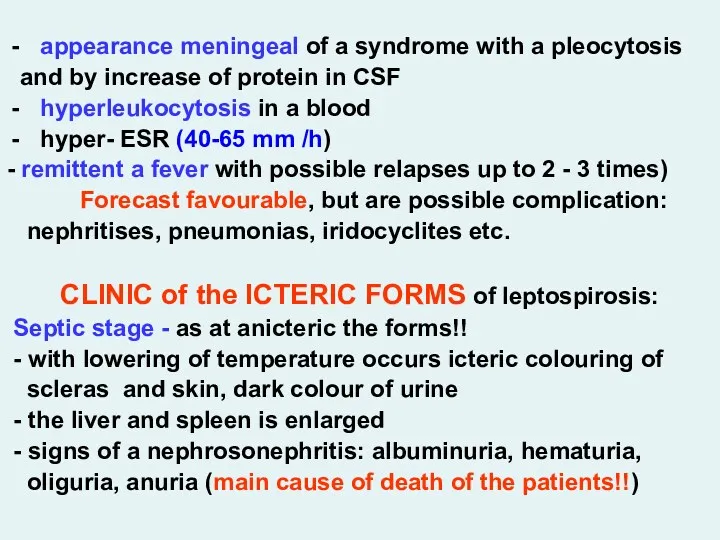
- 21. appearance meningeal of a syndrome with a pleocytosis and by increase of protein in CSF hyperleukocytosis
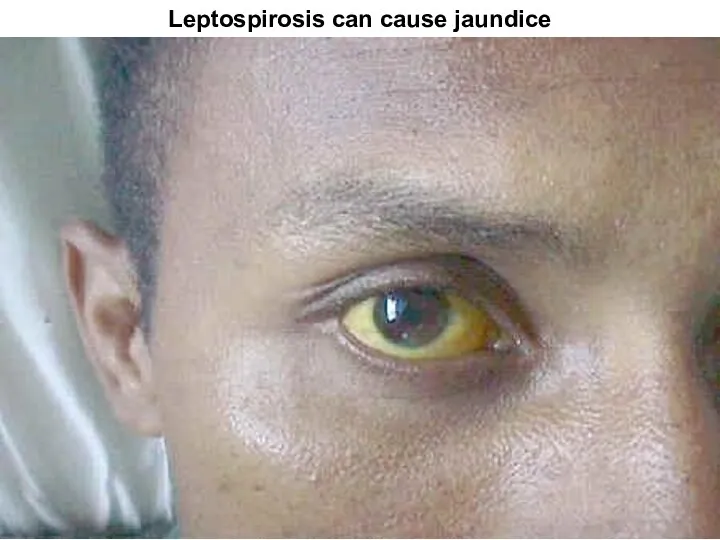
- 24. Leptospirosis can cause jaundice
- 27. - increase conjugated (direct) bilirubin at moderate rise АLТ (are not higher 2 - 4 norms)
- 28. LABORATORY DIAGNOSIS: - microscopy of a blood in a dark field (positive to 10 %) microscopy
- 29. - the icteric form: virus hepatitises, yellow fever, malaria, visceral leishmaniasis, yersiniosis, pseudotuberculosis, hemorrhagic fevers etc.
- 30. - at acute renal unsufficiency – diuretics (at once osmotic, at anuria - saluretics, but if
- 31. ANTHRAX – A. The acute infectious zoonotic disease described by development for the man of a
- 32. ETIOLOGY: Bacillus anthracis - large rod with equal edges 3-8 microns of length and 1-1.5 microns
- 36. Thermostable somatic polysaccharide the antigene is durably saved in corpses (is discovered by response of a
- 37. - eating corpses perished animals (predators) - through stings of insects (gadflies, horseflies, flies) Auxiliary source
- 38. Cases of man-to man transmission is not registered ! More often are sick cattle-breeder. The case
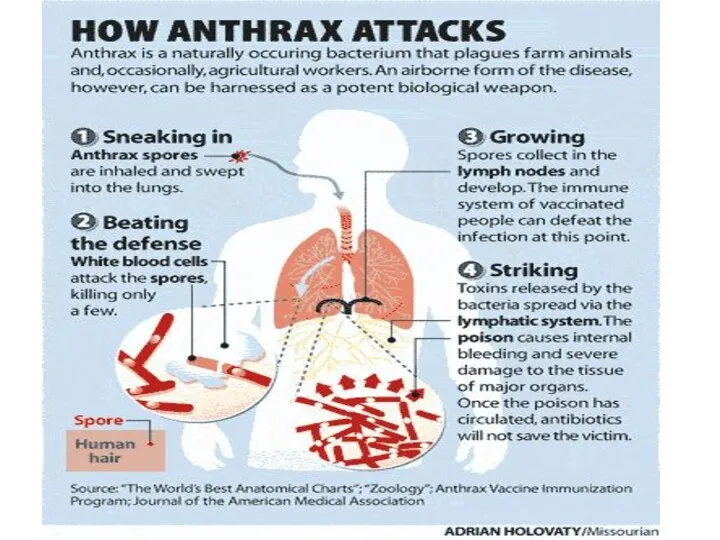
- 39. 3. The primary anthracic pneumonia does not develop! At aerogenic way of infection of spores will
- 40. CLINIC: (incubation interval from 2 about 14 days) The localized form of disease: in a place
- 52. Simultaneously around of a ulcer the edema considerably exceeding size of a ulcer is shaped. At
- 55. The generalized form А. - The incubation interval can be reduced about 1 day Acute beginning
- 56. Hemorrhagic meningitis resulting from inhalation anthrax.
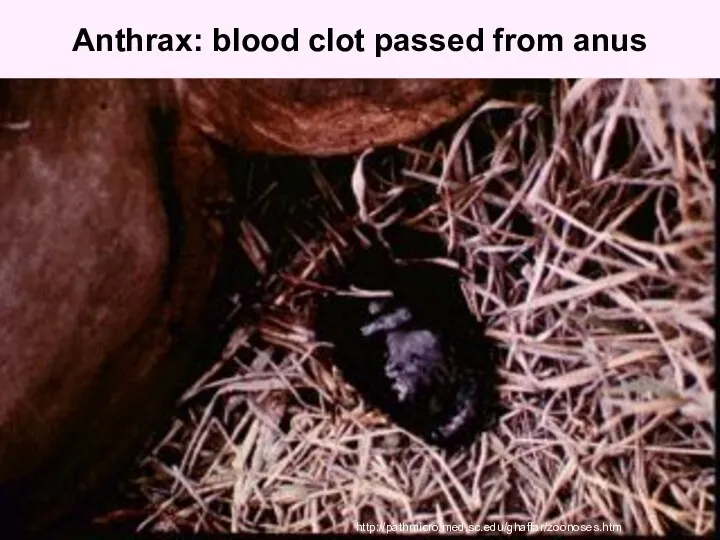
- 57. Anthrax: blood clot passed from anus http://pathmicro.med.sc.edu/ghaffar/zoonoses.htm
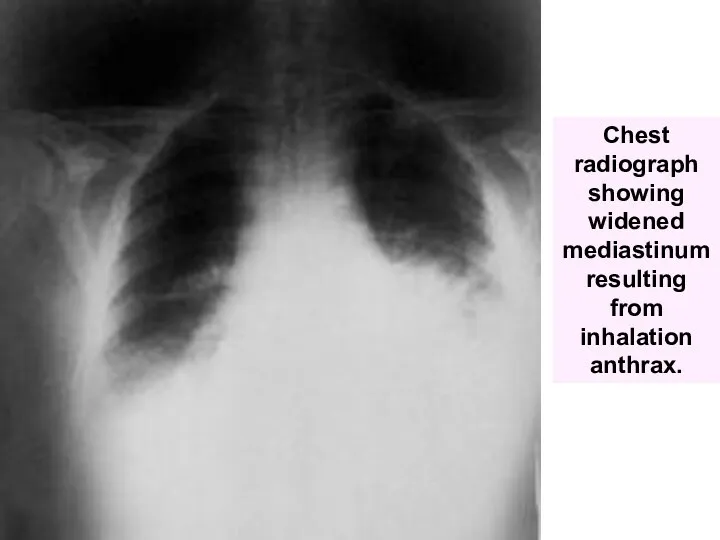
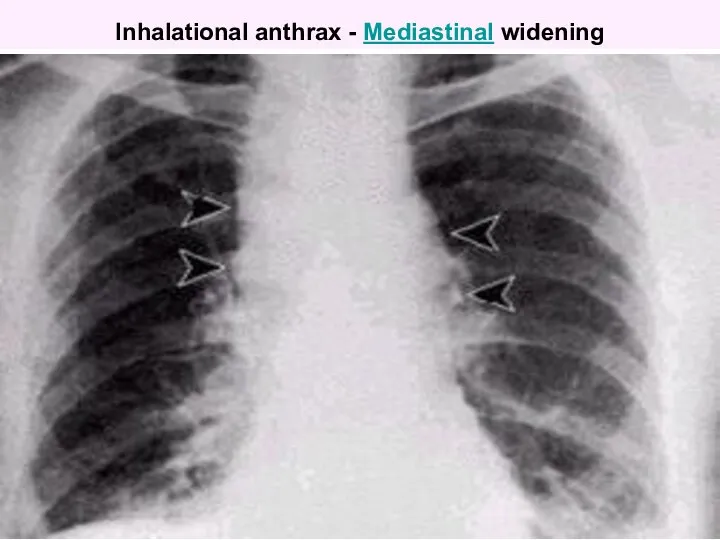
- 58. Chest radiograph showing widened mediastinum resulting from inhalation anthrax.
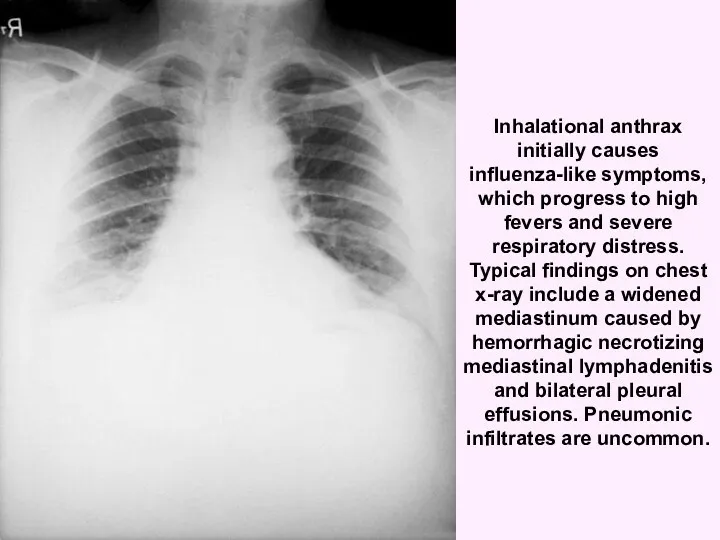
- 59. Inhalational anthrax initially causes influenza-like symptoms, which progress to high fevers and severe respiratory distress. Typical
- 60. Inhalational anthrax - Mediastinal widening
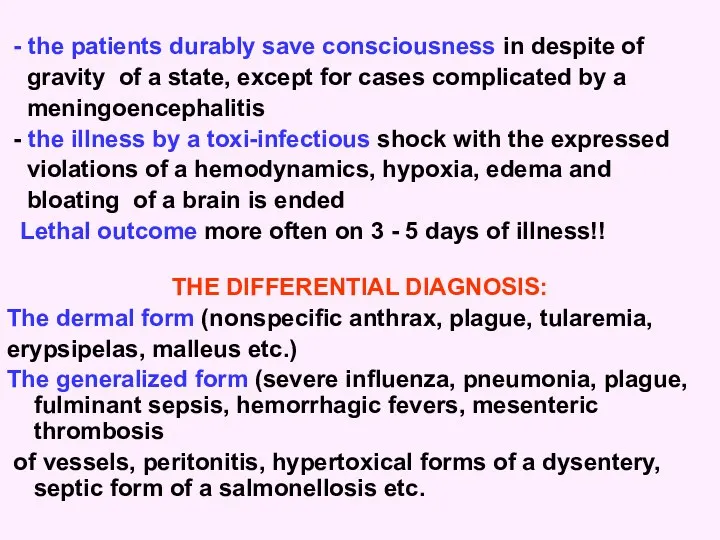
- 61. - the patients durably save consciousness in despite of gravity of a state, except for cases
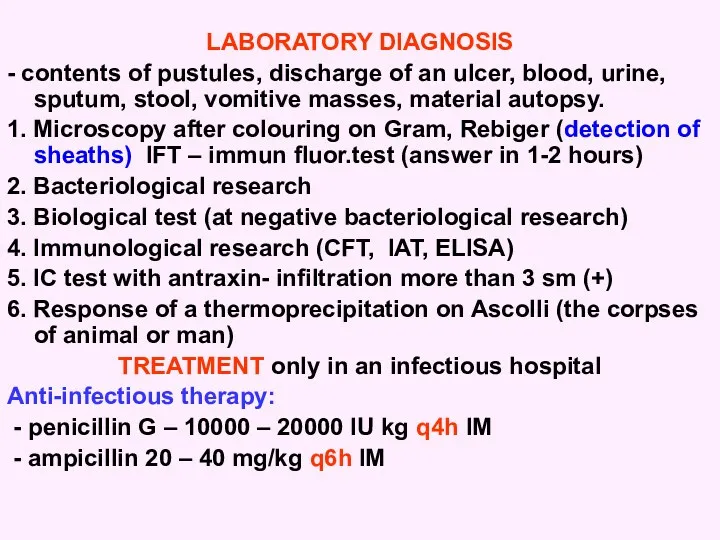
- 62. LABORATORY DIAGNOSIS - contents of pustules, discharge of an ulcer, blood, urine, sputum, stool, vomitive masses,
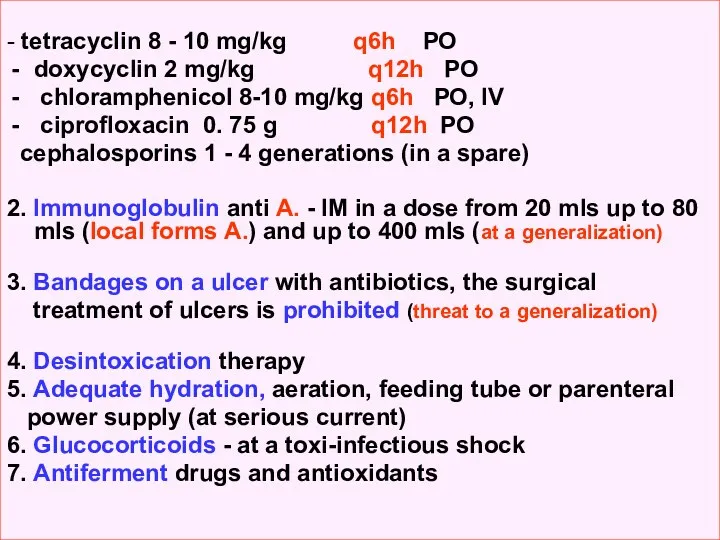
- 63. - tetracyclin 8 - 10 mg/kg q6h РО doxycyclin 2 mg/kg q12h РО chloramphenicol 8-10 mg/kg
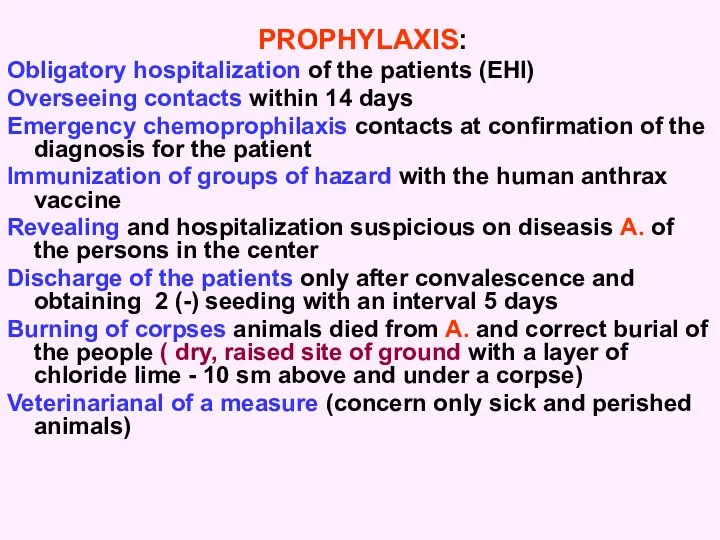
- 64. PROPHYLAXIS: Obligatory hospitalization of the patients (EHI) Overseeing contacts within 14 days Emergency chemoprophilaxis contacts at
- 69. Скачать презентацию
































 Алкогольные и неалкогольные стеатогепатиты
Алкогольные и неалкогольные стеатогепатиты Диабеттік нефропатия диагнозын анықтау, емдеу қантты диабеттің кеш асқынулары
Диабеттік нефропатия диагнозын анықтау, емдеу қантты диабеттің кеш асқынулары Симптоматология ревматоидного артрита, остеоартроза, диффузных болезней соединительной ткани. (Тема 33)
Симптоматология ревматоидного артрита, остеоартроза, диффузных болезней соединительной ткани. (Тема 33) Современная стоматологическая клиника социальной направленности (на примере р.п. Кантемировка)
Современная стоматологическая клиника социальной направленности (на примере р.п. Кантемировка) Внутричерепная гипертензия
Внутричерепная гипертензия Медленные инфекции. Механизм патогенеза
Медленные инфекции. Механизм патогенеза Геморрагическая лихорадка с почечным синдромом
Геморрагическая лихорадка с почечным синдромом Лапароскопия
Лапароскопия Клинические случаи в практике врача стоматолога
Клинические случаи в практике врача стоматолога История анестезиологии
История анестезиологии Развитие сестринского дела в России
Развитие сестринского дела в России Дифференциальная диагностика заболеваний с респираторным синдромом
Дифференциальная диагностика заболеваний с респираторным синдромом Иммунотропные средства
Иммунотропные средства Аллергия: диагностика, профилактика, лечение
Аллергия: диагностика, профилактика, лечение Балалар мекемелеріндегі санитарлық-техникалық жабдықтарға қойылатын гигиеналық талаптар. (Дәріс 19)
Балалар мекемелеріндегі санитарлық-техникалық жабдықтарға қойылатын гигиеналық талаптар. (Дәріс 19) 12 жұп бас ми нервтері
12 жұп бас ми нервтері Болезни конъюнктивы
Болезни конъюнктивы Фармакоэкономика. Оценка экономической эффективности лекарственных средств
Фармакоэкономика. Оценка экономической эффективности лекарственных средств Вырусные поражения половых органов
Вырусные поражения половых органов Microscopic colitis
Microscopic colitis Жасөспірім шақтағы ерте жүктіліктің алдын-алу
Жасөспірім шақтағы ерте жүктіліктің алдын-алу Лицевой нерв
Лицевой нерв Синдром длительного сдавления
Синдром длительного сдавления Қызметтік жүйелер туралы Анохиннің ілімі
Қызметтік жүйелер туралы Анохиннің ілімі Бет аймағының ақауларын протездеу. Эктопротездер
Бет аймағының ақауларын протездеу. Эктопротездер Расстройства воли и влечений, двигательные нарушения
Расстройства воли и влечений, двигательные нарушения Методы исследования ВНД. Электроэнцефалография. Лекция 2
Методы исследования ВНД. Электроэнцефалография. Лекция 2 Роль труда, спорта, социальных и биологических факторов на строение костей
Роль труда, спорта, социальных и биологических факторов на строение костей