Слайд 2
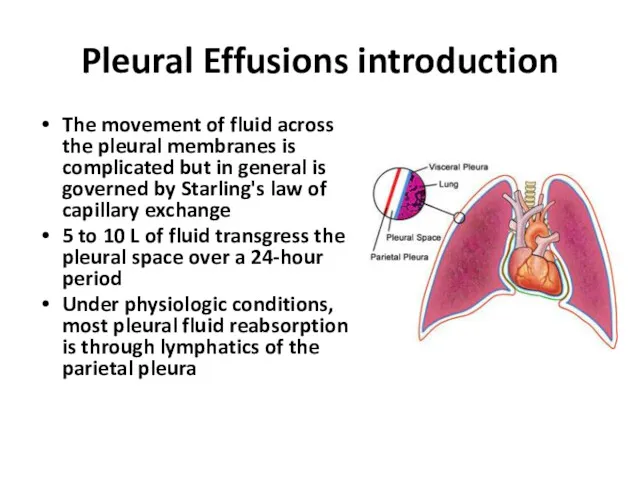
Pleural Effusions introduction
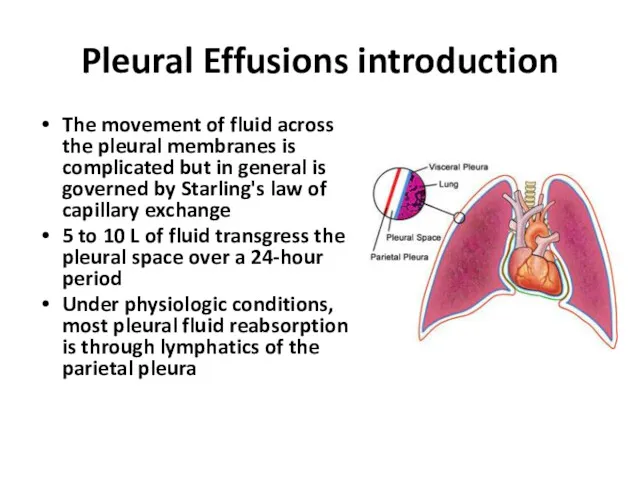
The movement of fluid across the pleural membranes is
complicated but in general is governed by Starling's law of capillary exchange
5 to 10 L of fluid transgress the pleural space over a 24-hour period
Under physiologic conditions, most pleural fluid reabsorption is through lymphatics of the parietal pleura
Слайд 3
Pleural Effusions introduction
imbalance of accumulation and absorption of pleural fluid will
lead to the development of a pleural effusion:
1. Increased hydrostatic pressure
2. Increased negative intrapleural pressure
3. Increased capillary permeability
4. Decreased plasma oncotic pressure
5. Decreased or interrupted lymphatic drainage
Слайд 4
Pleural Effusions introduction
About 300 mL of fluid is required for the
development of costophrenic angle blunting seen on an upright chest radiograph.
At least 500 mL of effusion is necessary for detection on clinical examination.
Слайд 5
Transudative Vs. Exudative Effusions
Criteria:
1. Pleural fluid protein/serum protein greater
than 0.5
2. Pleural fluid LDH/serum LDH greater than 0.6
3. Pleural fluid LDH 1.67 times normal serum
These criteria misidentify ~25% of transudates as exudates
A transudative pleural effusion occurs when systemic factors that influence the formation and absorption of pleural fluid are altered.
An exudative pleural effusion occurs when local factors that influence the formation and absorption of pleural fluid are altered
Слайд 6
Diagnostic Approach
The leading causes of transudative pleural effusions in the United
States are left-ventricular failure and cirrhosis
The leading causes of exudative pleural effusions are bacterial pneumonia, malignancy, viral infection, and pulmonary embolism.
Слайд 7
Pleural fluid analysis
Gross appearance (pus- Empyema, black- Aspergillus, green- Biliothorax, white- Chylothorax)
Very
high LDH- empyema, rheumatoid pleurisy, malignancy
High triglyceride- Chylothorax
Low glucose- Rheumatoid pleurisy, parapneumonic effusion or empyema, Malignant effusion, Tuberculous pleurisy, Lupus pleuritis, Esophageal rupture
Low pH- parapneumonic effusion or empyema, Malignant effusion
High amylase- Acute pancreatitis, Chronic pancreatic pleural effusion, Esophageal rupture, Malignancy
adenosine deaminase (ADA), interferon gamma - Tuberculous pleurisy
Lymphocytosis- tuberculous pleurisy, lymphoma, sarcoidosis, chronic rheumatoid pleurisy
Слайд 8

Слайд 9
Effusion Due to Heart Failure
A diagnostic thoracentesis should be performed
if the effusions are not bilateral and comparable in size, if the patient is febrile, if the patient has pleuritic chest pain or if the effusion persists despite therapy
A pleural fluid N-terminal pro-brain natriuretic peptide (NT-proBNP) >1500 pg/mL is virtually diagnostic of an effusion secondary to congestive heart failure
Слайд 10
Hepatic Hydrothorax
Pleural effusions occur in ~5% of patients with cirrhosis and
ascites
effusion is usually right-sided
Слайд 11
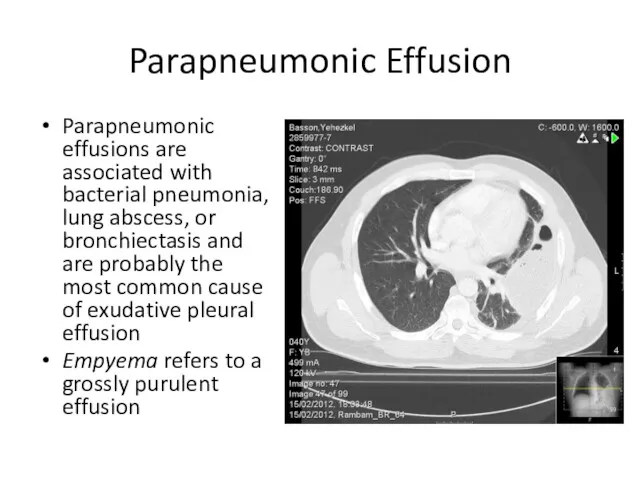
Parapneumonic Effusion
Parapneumonic effusions are associated with bacterial pneumonia, lung abscess, or
bronchiectasis and are probably the most common cause of exudative pleural effusion
Empyema refers to a grossly purulent effusion
Слайд 12
Parapneumonic Effusion
Patients with aerobic bacterial pneumonia and pleural effusion present with
an acute febrile illness consisting of chest pain, sputum production, and leukocytosis
Patients with anaerobic infections present with a subacute illness
If the free fluid separates the lung from the chest wall by >10 mm, a therapeutic thoracentesis should be performed
Слайд 13
Uncomplicated Vs. Complicated parapneumonic effusion
An uncomplicated parapneumonic effusion has "exudative"
chemistries, normal pH and glucose, and negative cultures
A complicated parapneumonic effusion typically has "exudative" chemistries, a low pleural pH (pH <7.20), a low glucose, and is often loculated
Слайд 14
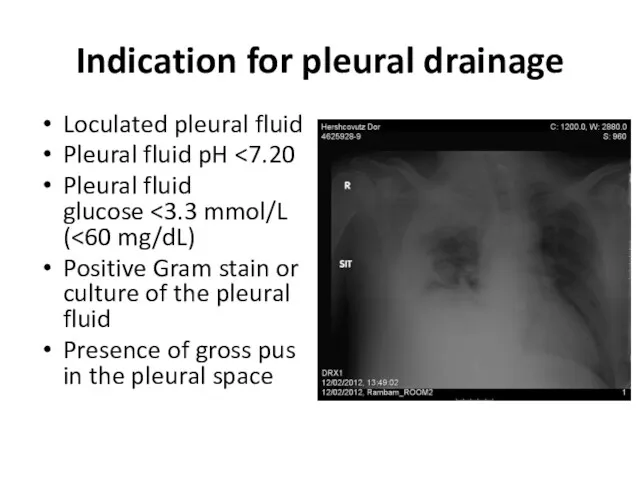
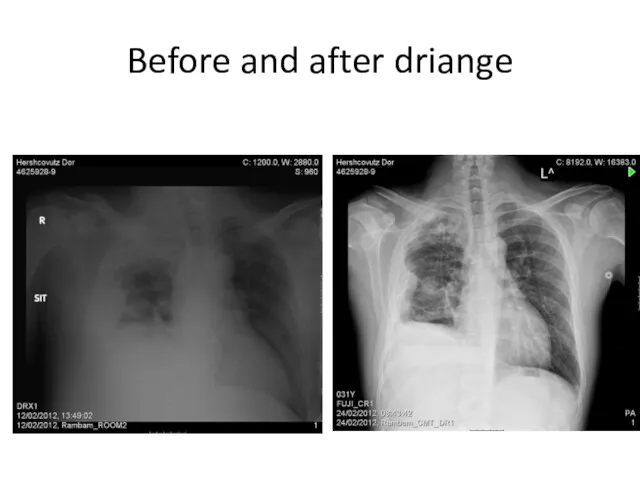
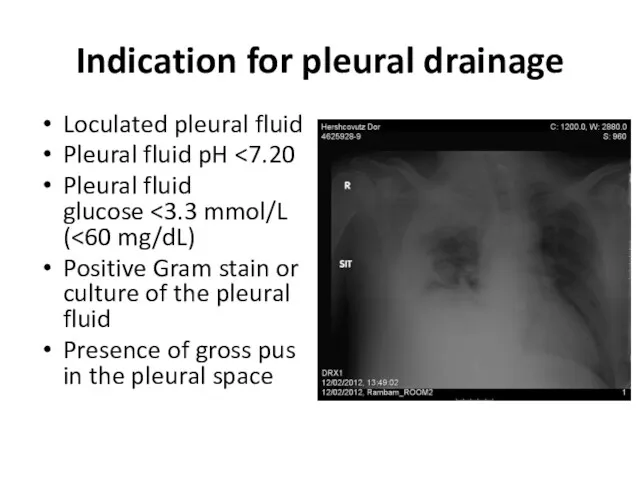
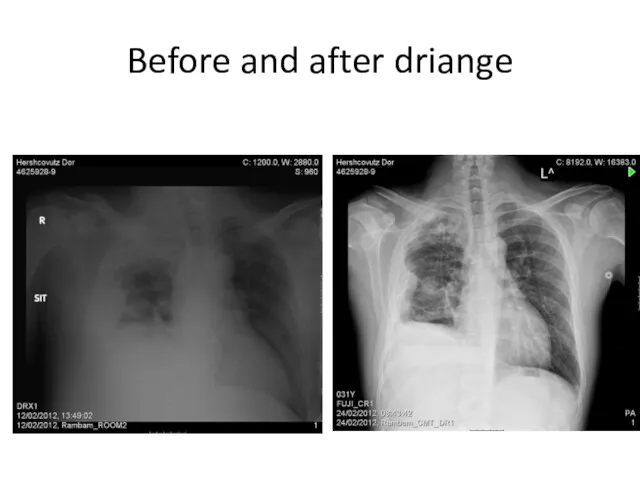
Indication for pleural drainage
Loculated pleural fluid
Pleural fluid pH <7.20
Pleural fluid glucose <3.3
mmol/L (<60 mg/dL)
Positive Gram stain or culture of the pleural fluid
Presence of gross pus in the pleural space
Слайд 15
Слайд 16
Treatment of parapneumonic effusion
An empiric, broad spectrum antibiotic that includes
coverage for anaerobic organisms
In patients with an uncomplicated parapneumonic effusion that is small to moderate in size, free flowing, and has a pH of 7.20 or greater there is no indication for drainage
In patients with a large, loculated, or complicated parapneumonic effusion there is indication for prompt drainage of any remaining pleural fluid by chest tube.
Слайд 17

Effusion Secondary to Malignancy
Malignant pleural effusions secondary to metastatic disease are
the second most common type of exudative pleural effusion
The three tumors that cause ~75% of all malignant pleural effusions are lung carcinoma, breast carcinoma, and lymphoma
Слайд 18

Effusion Secondary to Malignancy
The diagnosis usually is made via cytology of
the pleural fluid
If the initial cytologic examination is negative, thoracoscopy is the best next procedure if malignancy is strongly suspected
Слайд 19
Treatment of Malignant pleural effusion
If the patient's lifestyle is compromised
by dyspnea and if the dyspnea is relieved with a therapeutic thoracentesis, one of the following procedures should be considered:
therapeutic thoracentesis
insertion of a small indwelling catheter
pleurodesis
Слайд 20
Pneumothorax introduction
Pneumothorax is the accumulation of air within the pleural space
Pneumothorax
can be spontaneous or occur secondary to a traumatic, surgical, therapeutic, or disease-related event
pneumothorax compresses lung tissue and reduces pulmonary compliance, ventilatory volumes, and diffusing capacity
If air enters the pleural space repeatedly and is unable to escape, positive pressure will develop in the pleural space. This situation is called a tension pneumothorax
Слайд 21
Pneumothorax introduction
Patients with pneumothorax most commonly present with chest pain (sharp
and pleuritic) and dyspnea
Characteristic physical findings include:
Hyperresonance on percussion
Breath sounds are diminished to absent.
Subcutaneous emphysema may be palpated
Слайд 22
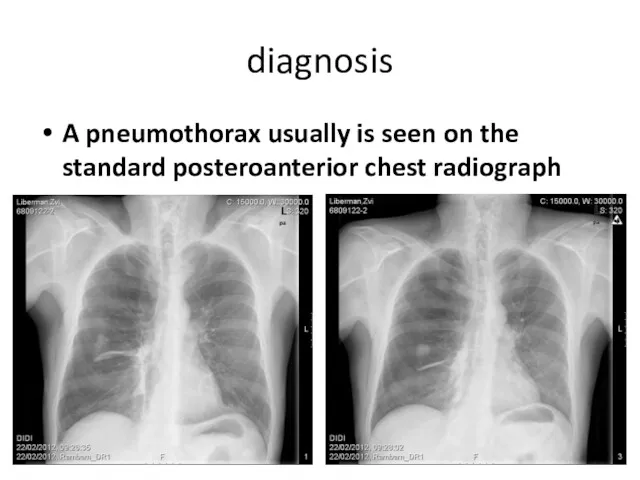
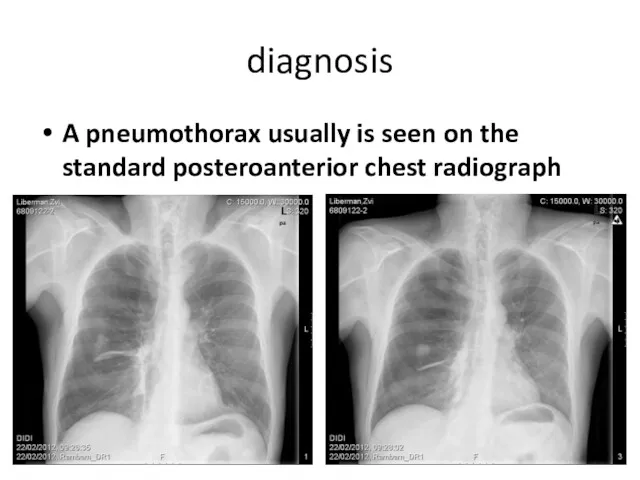
diagnosis
A pneumothorax usually is seen on the standard posteroanterior chest radiograph
Слайд 23
Слайд 24
Classifications of Pneumothorax
Spontaneous
Primary
Secondary
Traumatic
Iatrogenic
Esophageal perforation
Слайд 25
primary spontaneous pneumothorax
A primary spontaneous pneumothorax occurs in the absence
of underlying lung disease
Patients are often tall, thin and smoker men from 25 to 40 years of age (rare after age 40)
Risk factor include: smoking, family history, Marfan syndrome, homocystinuria, and thoracic endometriosis
Primary spontaneous pneumothoraxes are usually due to rupture of apical pleural blebs (>85%)
25-50% of patients with a first time spontaneous pneumothorax will have a recurrence (most recurrences occurring within the first year )
Слайд 26
Treatment of primary spontaneous pneumothorax
Small pneumothoraces (<20%, ≤2 to 3
cm between the lung and chest wall on a chest radiograph) that are stable may be monitored if the patient has few symptoms. An uncomplicated pneumothorax reabsorbs at a rate of about 1% per day.
Indications for intervention include progressive pneumothorax, delayed pulmonary expansion, or development of symptoms.
Слайд 27
Treatment of primary spontaneous pneumothorax
Moderate (20%-40%) and large (>40%) pneumothoraces
nearly always are associated with persistent symptoms that cause physical limitations and require intervention
Simple needle aspiration of a pneumothorax may relieve symptoms and can promote quicker lung re-expansion
Tube thoracostomy (chest tube insertion) and underwater seal drainage are the mainstays of treatment for spontaneous pneumothorax.
The classic location for chest tube insertion is through the fourth, fifth, or sixth intercostal space in the mid to anterior axillary line.
Слайд 28
Treatment of primary spontaneous pneumothorax
Complications of chest tube insertion for
pneumothorax are infrequent but include laceration of an intercostal vessel, laceration of the lung, intrapulmonary or extrathoracic placement of the chest tube, and infection.
When an air leak persist for more than 72 hours or the lung not completely re-expand, surgical intervention is warranted
Слайд 29
Indication for Surgical intervention in spontaneous pneumothorax
Air leak that persist
for more than 72 hours or when the lung not completely re-expand
Bilateral simultaneous pneumothoraces
Complete (100%) pneumothorax
Pneumothorax associated with tension or borderline cardiopulmonary reserve
Pneumothorax in patients in high-risk professions or activities
A recurrence pneumothorax
Слайд 30
Surgical intervention for spontaneous pneumothorax
Apical blebs are resected. The parietal
pleura over the apex of the hemithorax can be removed (pleurectomy), abraded (mechanical pleurodesis), or treated with talc or tetracycline-like agents (chemical pleurodesis or poudrage).
The recurrence rate of these procedures, performed open or closed, is less than 5%
Слайд 31
Secondary spontaneous pneumothorax
Most secondary pneumothoraxes are due to chronic obstructive
pulmonary disease
Pneumothorax in patients with lung disease is more life-threatening than it is in normal individuals because of the lack of pulmonary reserve in these patients.
Treatment of secondary pneumothorax is very similar to PSP but most of the patients with secondary pneumothorax should be treated with tube thoracostomy.
Слайд 32
Preventing recurrence
smoking cessation
VATS pleurodesis- The rate of recurrent pneumothorax is less
than 5 percent after VATS with bleb/bullae resection and pleurodesis
Chemical pleurodesis- decreases the recurrence rate for pneumothorax to 15-25%
Слайд 33

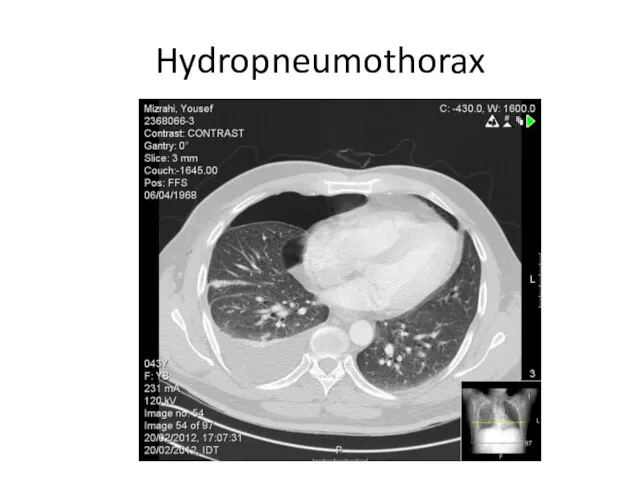
Traumatic pneumothoraxes
Traumatic pneumothoraxes can result from both penetrating and blunt
chest trauma
Some times when a hemopneumothorax is present, one chest tube should be placed in the superior part of the hemithorax to evacuate the air and another should be placed in the inferior part of the hemithorax to remove the blood.
Слайд 34

Слайд 35
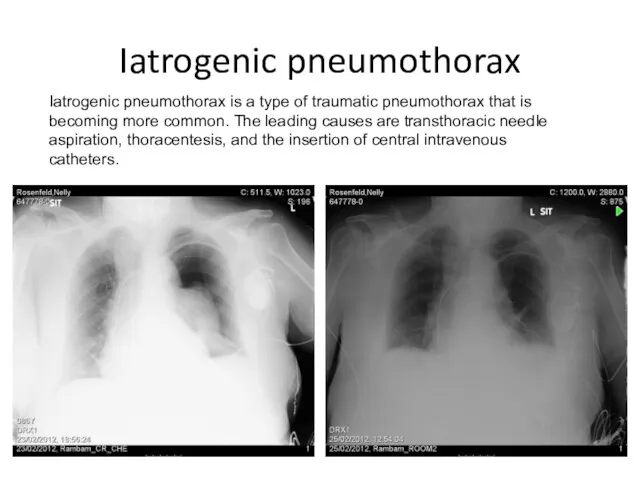
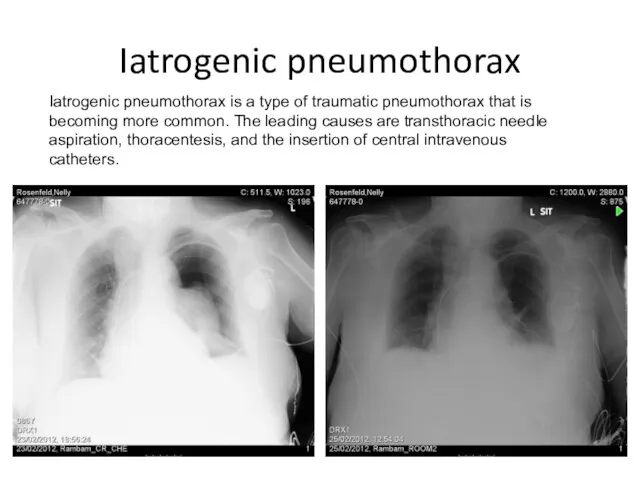
Iatrogenic pneumothorax
Iatrogenic pneumothorax is a type of traumatic pneumothorax that is
becoming more common. The leading causes are transthoracic needle aspiration, thoracentesis, and the insertion of central intravenous catheters.
Слайд 36
tension pneumothorax
hemodynamic collapse (decreased venous return to the heart and reduced
cardiac output)
severe respiratory compromise
compression or collapse of the entire lung
shifting of the mediastinum and heart away from the pneumothorax
Слайд 37
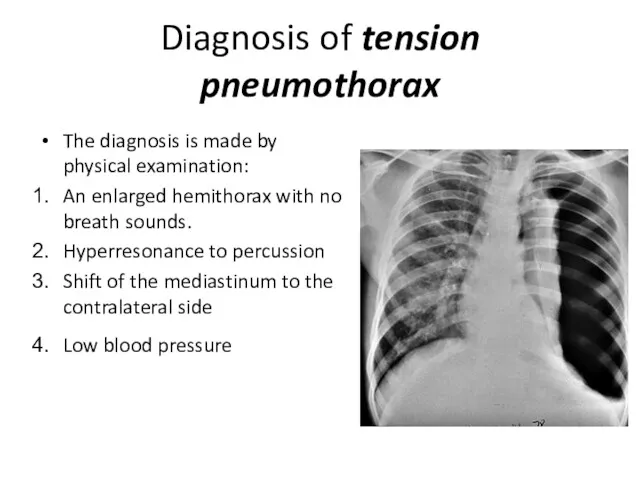
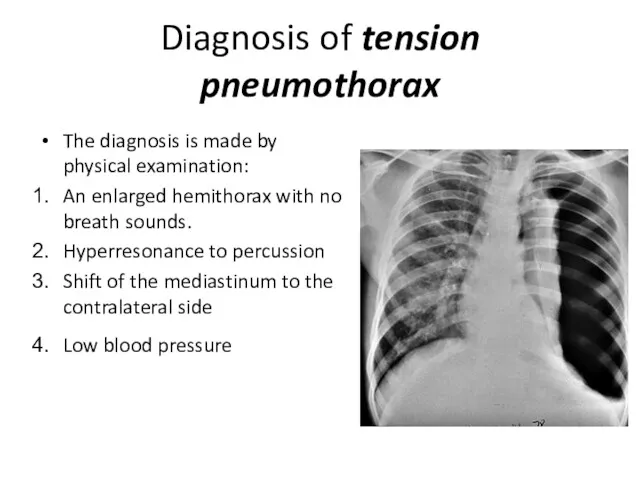
Diagnosis of tension pneumothorax
The diagnosis is made by physical examination:
An enlarged
hemithorax with no breath sounds.
Hyperresonance to percussion
Shift of the mediastinum to the contralateral side
Low blood pressure





 Электрофизиологические основы ЭКГ. Электрическая ось сердца. ЭКГ-характеристика гипертрофий
Электрофизиологические основы ЭКГ. Электрическая ось сердца. ЭКГ-характеристика гипертрофий Предлежание плаценты
Предлежание плаценты Эвтаназия, как важнейшая проблема современной биоэтики. Хоспис, как альтернатива активной эвтаназии
Эвтаназия, как важнейшая проблема современной биоэтики. Хоспис, как альтернатива активной эвтаназии Организация работы органов, осуществляющих медицинскую помощь гражданам. Тема 8
Организация работы органов, осуществляющих медицинскую помощь гражданам. Тема 8 Атеросклероз. Клиникалық қөріністері. Емдеу жолдары. Қорытынды
Атеросклероз. Клиникалық қөріністері. Емдеу жолдары. Қорытынды Организация работы детской городской поликлиники и больницы
Организация работы детской городской поликлиники и больницы Воспаление висцеральной и париетальной брюшины малого таза - пельвиоперитонит
Воспаление висцеральной и париетальной брюшины малого таза - пельвиоперитонит Современное состояние и перспективы развития антимикробной химиотерапии
Современное состояние и перспективы развития антимикробной химиотерапии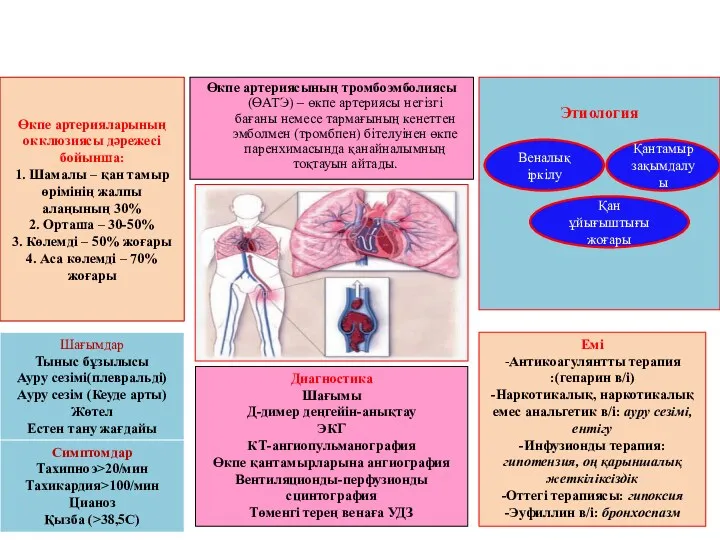 Өкпе артерияларының окклюзиясы дəрежесі бойынша: 1. Шамалы – қан тамыр өрімінің жалпы алаңының 30% 2. Орташа – 30-50% 3
Өкпе артерияларының окклюзиясы дəрежесі бойынша: 1. Шамалы – қан тамыр өрімінің жалпы алаңының 30% 2. Орташа – 30-50% 3 Синдром болей в левой половине грудной клетки. ИБС в практике терапевта поликлиники
Синдром болей в левой половине грудной клетки. ИБС в практике терапевта поликлиники Острая церебральная недостаточность
Острая церебральная недостаточность Клеточные факторы врождённого иммунитета. Фагоцитоз и его стадии
Клеточные факторы врождённого иммунитета. Фагоцитоз и его стадии Общие закономерности роста и развития детей и подростков
Общие закономерности роста и развития детей и подростков Қыз балалар гинекологиясының негіздері
Қыз балалар гинекологиясының негіздері Расстройства внимания
Расстройства внимания Острый респираторный дистресс-синдром
Острый респираторный дистресс-синдром Острый ларингит
Острый ларингит Физическое развитие и функциональное состояние организма. Медицинский контроль
Физическое развитие и функциональное состояние организма. Медицинский контроль Церебральные инсульты у взрослых
Церебральные инсульты у взрослых Специфические заболевания ЛОР-органов
Специфические заболевания ЛОР-органов Диагностика в терапии. Заболевания сердечно-сосудистой системы
Диагностика в терапии. Заболевания сердечно-сосудистой системы Ишемическая болезнь сердца. Стабильная стенокардия напряжения. Ведение на современном этапе
Ишемическая болезнь сердца. Стабильная стенокардия напряжения. Ведение на современном этапе Энтероколит. Колиттер. Гельминтоздар
Энтероколит. Колиттер. Гельминтоздар Пищевая аллергия и пищевая непереносимость
Пищевая аллергия и пищевая непереносимость Стоматологические материалы на основе полимеров (базисные и для искусственных зубов)
Стоматологические материалы на основе полимеров (базисные и для искусственных зубов) Tпринципы терапии дыхательных расстройств
Tпринципы терапии дыхательных расстройств Этика и деонтология для работников регистратур медицинских организаций
Этика и деонтология для работников регистратур медицинских организаций Лучевые синдромы поражения легких
Лучевые синдромы поражения легких