Содержание
- 2. Neural basis of consciousness Consciousness cannot be readily defined in terms of anything else A state
- 3. Mental Status = Arousal + Content
- 4. Anatomy of Mental Status Ascending reticular activating system (ARAS) Activating systems of upper brainstem, hypothalamus, thalamus
- 5. Sum of patient’s intellectual (cognitive) functions and emotions (affect) Sensations, emotions, memories, images, ideas (SEMII) Depends
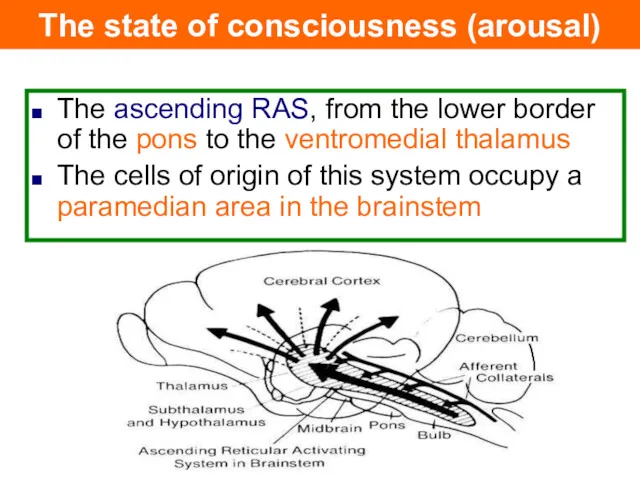
- 6. The ascending RAS, from the lower border of the pons to the ventromedial thalamus The cells
- 7. Abnormal change in level of arousal or altered content of a patient's thought processes Change in
- 8. Definitions of levels of arousal (conciousness) Alert (Conscious) - Appearance of wakefulness, awareness of the self
- 9. Semicoma was defined as complete loss of consciousness with a response only at the reflex level
- 10. Psychogenic unresponsiveness The patient, although apparently unconscious, usually shows some response to external stimuli An attempt
- 11. Patients who survive coma do not remain in this state for > 2–3 weeks, but develop
- 12. Locked in syndrome Patient is awake and alert, but unable to move or speak. Pontine lesions
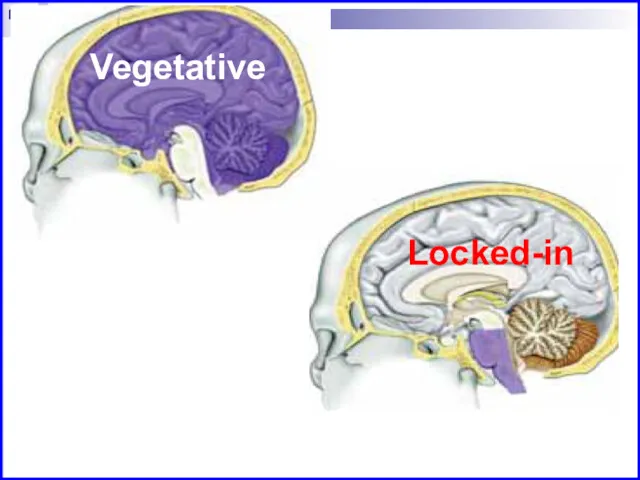
- 13. Vegetative Locked-in
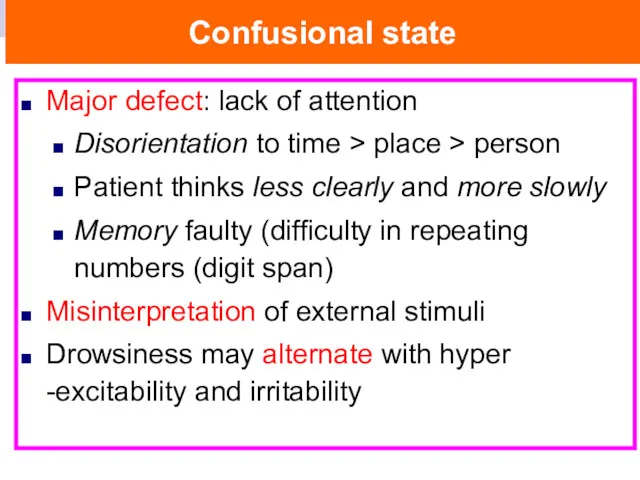
- 14. Confusional state Major defect: lack of attention Disorientation to time > place > person Patient thinks
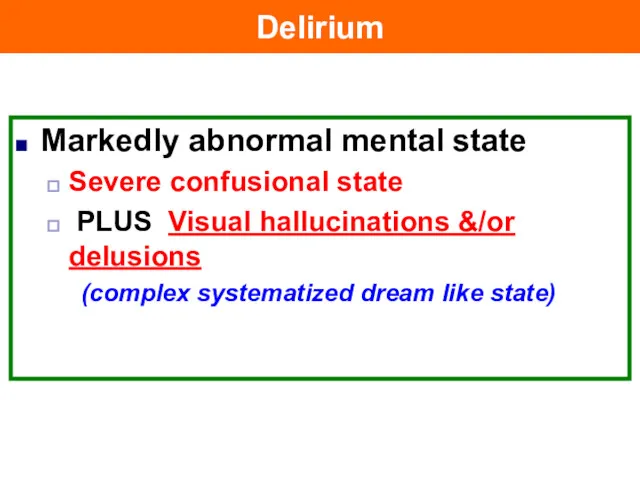
- 15. Delirium Markedly abnormal mental state Severe confusional state PLUS Visual hallucinations &/or delusions (complex systematized dream
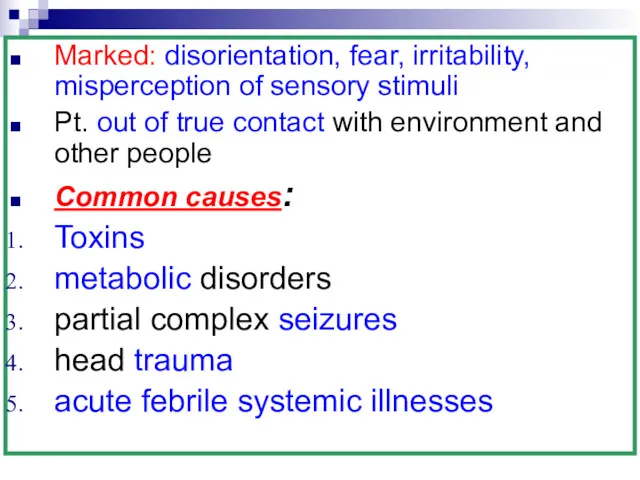
- 16. Marked: disorientation, fear, irritability, misperception of sensory stimuli Pt. out of true contact with environment and
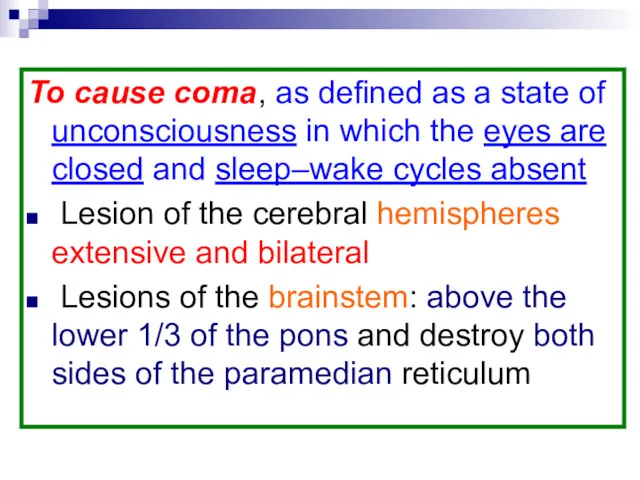
- 17. To cause coma, as defined as a state of unconsciousness in which the eyes are closed
- 18. The use of terms other than coma and stupor to indicate the degree of impairment of
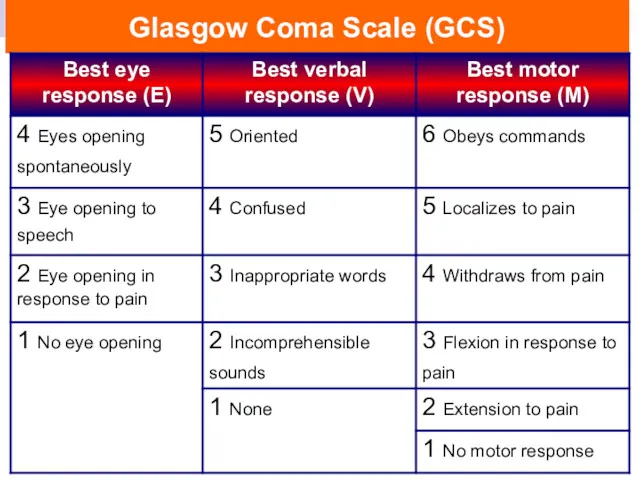
- 19. Glasgow Coma Scale (GCS)
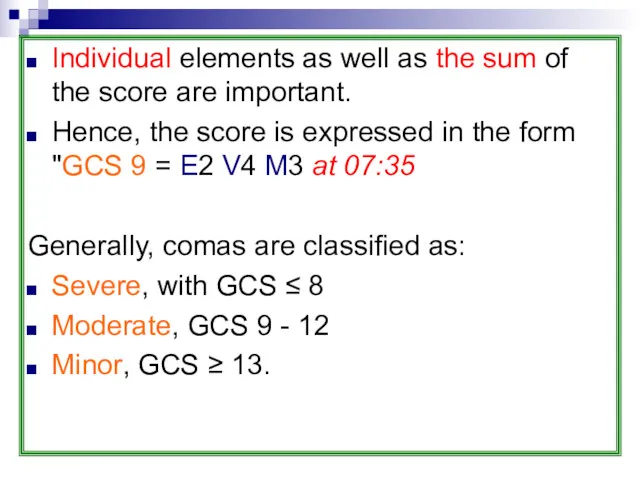
- 20. Individual elements as well as the sum of the score are important. Hence, the score is
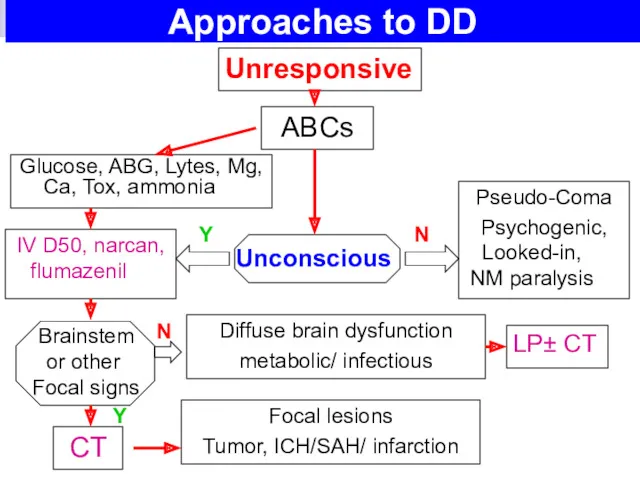
- 21. Approaches to DD Glucose, ABG, Lytes, Mg, Ca, Tox, ammonia Unresponsive ABCs IV D50, narcan, flumazenil
- 22. Approaches to DD General examination: On arrival to ER immediate attention to: Airway Circulation establishing IV
- 23. Attention is then directed towards: Assessment of the patient Severity of the coma Diagnostic evaluation All
- 24. Previous medical history: Epilepsy DM, Drug history Clues obtained from the patient's Clothing or Handbag Careful
- 25. If head trauma is suspected, the examination must await adequate stabilization of the neck. Glasgow Coma
- 26. Temperature Hypothermia Hypopituitarism, Hypothyroidism Chlorpromazine Exposure to low temperature environments, cold-water immersion Risk of hypothermia in
- 27. C/P: generalized rigidity and muscle fasciculation but true shivering may be absent. (a low-reading rectal thermometer
- 28. Hyperthermia (febrile Coma) Infective: encephalitis, meningitis Vascular: pontine, subarachnoid hge Metabolic: thyrotoxic, Addisonian crisis Toxic: belladonna,
- 29. Hyperthermia or heat stroke Loss of thermoregulation dt. prolonged exertion in a hot environment Initial ↑
- 30. This may be exacerbated by certain drugs, ‘Ecstasy’ abuse—involving a loss of the thirst reaction in
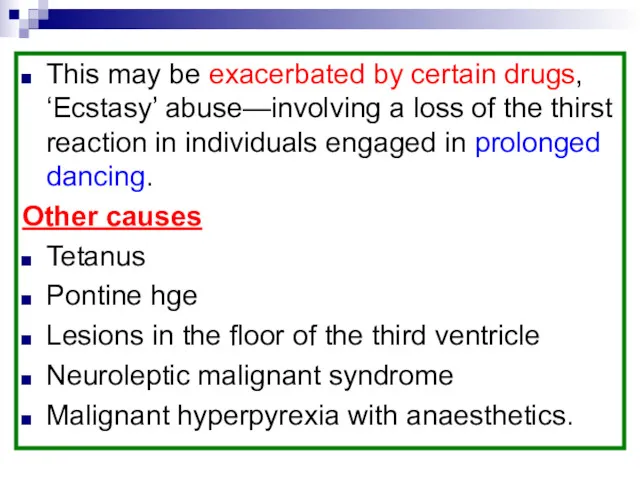
- 31. Heat stroke neurological sequelae Paraparesis. Cerebellar ataxia. Dementia (rare)
- 32. Pulse Bradycardia: brain tumors, opiates, myxedema. Tachycardia: hyperthyroidism, uremia Blood Pressure High: hypertensive encephalopathy Low: Addisonian
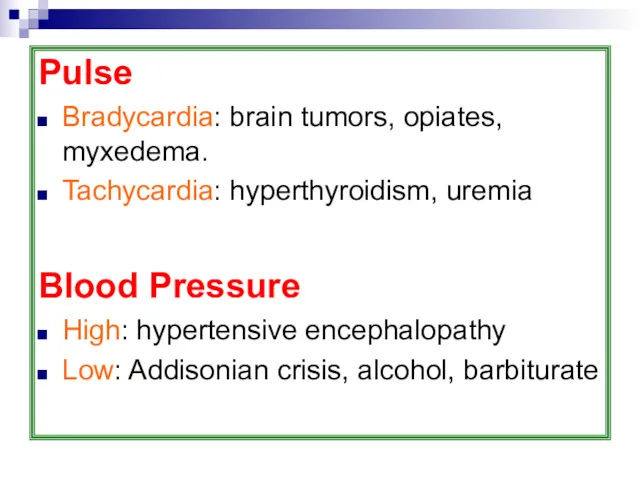
- 33. Skin Injuries, Bruises: traumatic causes Dry Skin: DKA, Atropine Moist skin: Hypoglycemic coma Cherry-red: CO poisoning
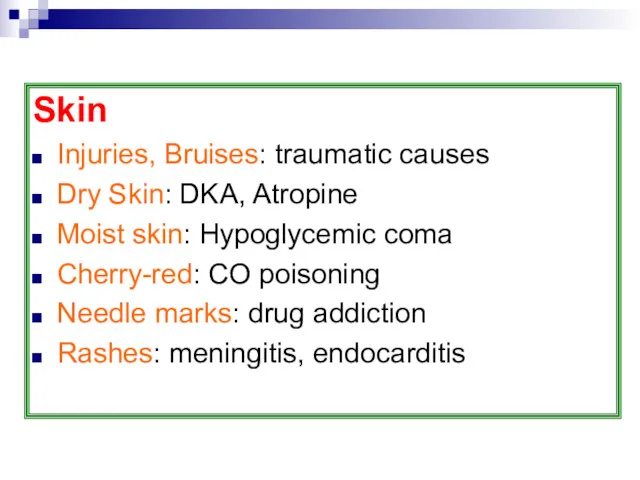
- 34. Pupils Size, inequality, reaction to a bright light. An important general rule: most metabolic encephalopathies give
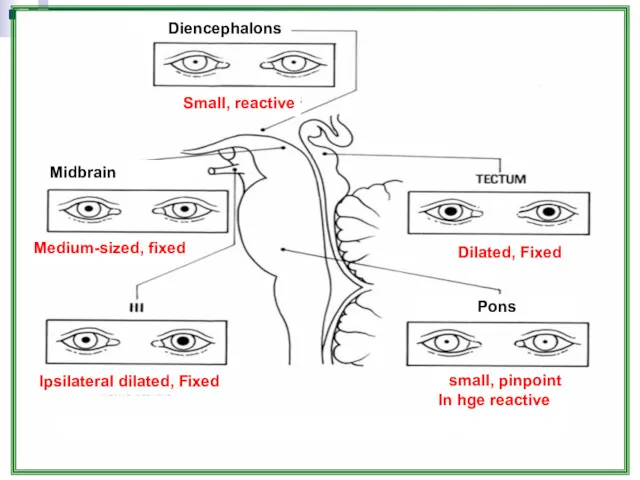
- 35. Structural lesions are more commonly associated with pupillary asymmetry and with loss of light reflex. Midbrain
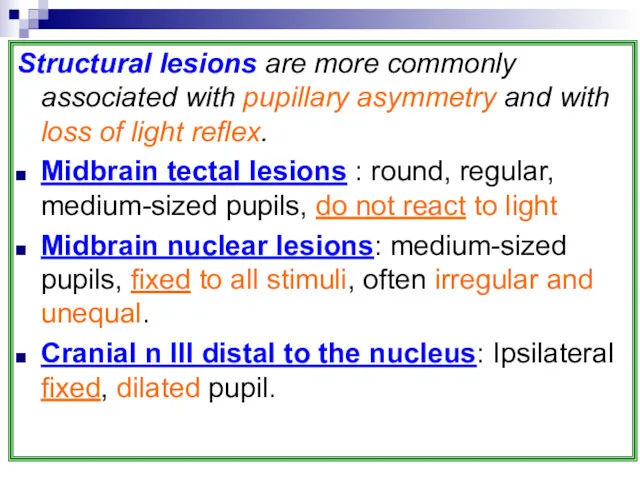
- 36. Pons (Tegmental lesions) : bilaterally small pupils, {in pontine hge, may be pinpoint, although reactive} assess
- 37. Small, reactive Diencephalons Dilated, Fixed small, pinpoint In hge reactive Pons Midbrain Ipsilateral dilated, Fixed Medium-sized,
- 38. Ocular movements The position of the eyes at rest Presence of spontaneous eye movement The reflex
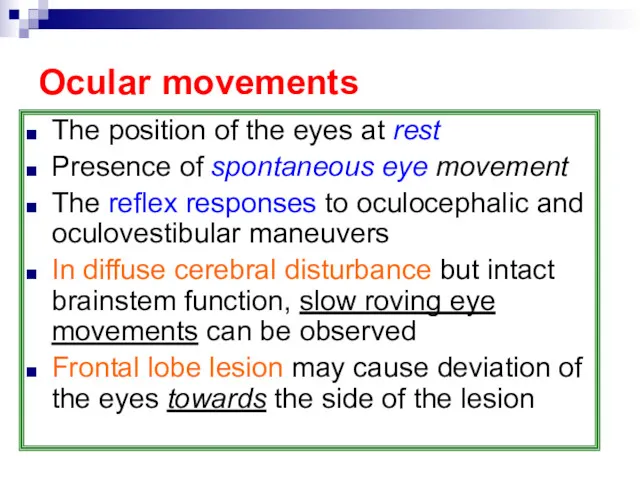
- 39. Lateral pontine lesion can cause conjugate deviation to the opposite side Midbrain lesion Conjugate deviation downwards
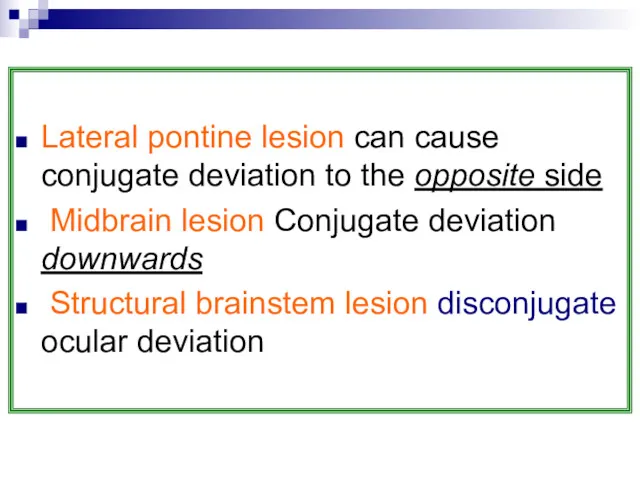
- 40. The oculocephalic (doll's head) response rotating the head from side to side and observing the position
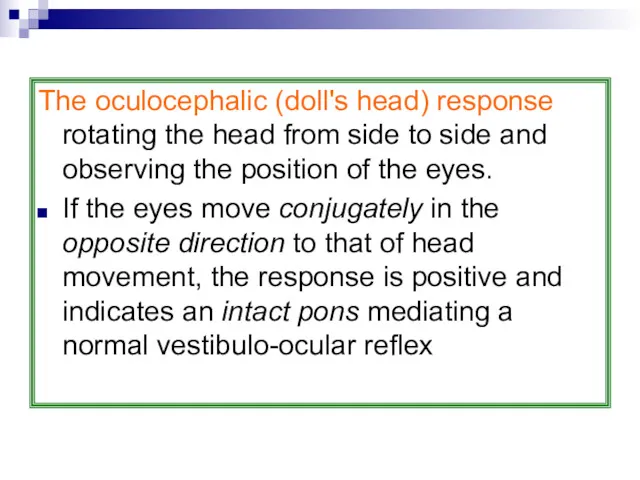
- 41. Caloric oculovestibular responses These are tested by the installation of ice-cold water into the external auditory
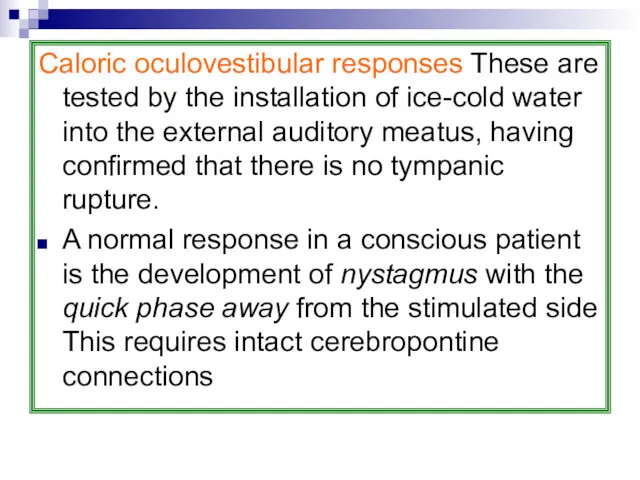
- 42. Odour of breath Acetone: DKA Fetor Hepaticus: in hepatic coma Urineferous odour: in uremic coma Alcohol
- 43. Respiration Cheyne–Stokes respiration: (hyperpnoea alternates with apneas) is commonly found in comatose patients, often with cerebral
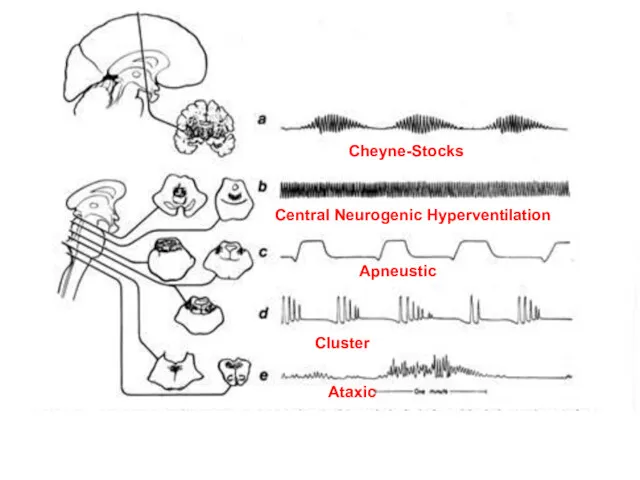
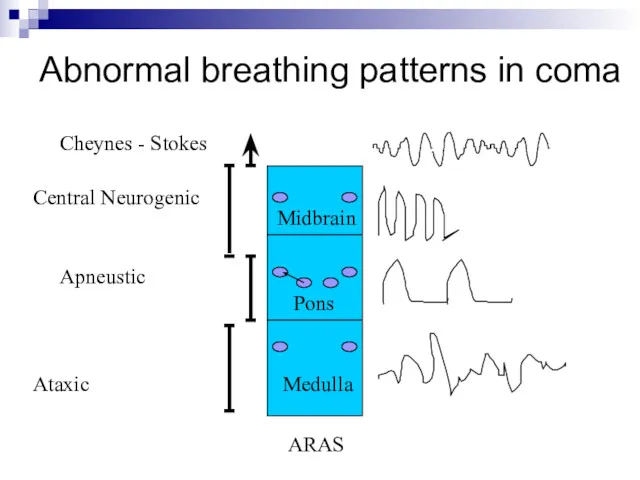
- 44. Central neurogenic hyperventilation Brainstem tegmentum (mostly tumors): ↑ PO2, ↓ PCO2, and Respiratory alkalosis in the
- 45. Apneustic breathing Brainstem lesions Pons may also give with a pause at full inspiration Ataxic: Medullary
- 47. Abnormal breathing patterns in coma Midbrain Pons Medulla ARAS Cheynes - Stokes Ataxic Apneustic Central Neurogenic
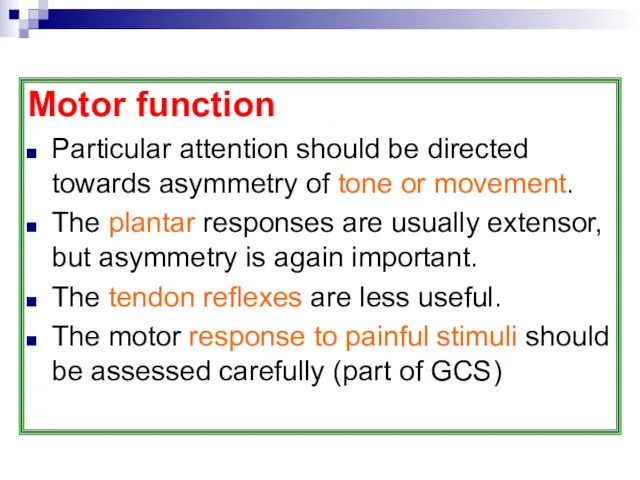
- 48. Motor function Particular attention should be directed towards asymmetry of tone or movement. The plantar responses
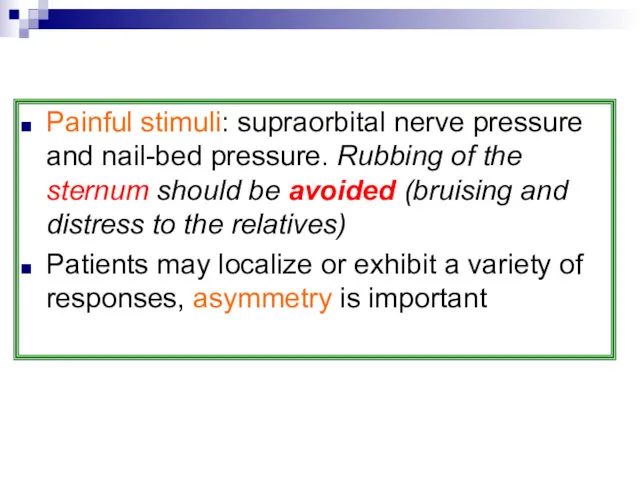
- 49. Painful stimuli: supraorbital nerve pressure and nail-bed pressure. Rubbing of the sternum should be avoided (bruising
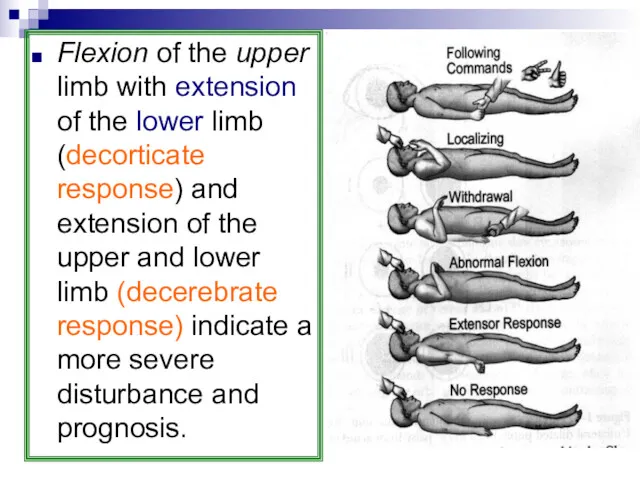
- 50. Flexion of the upper limb with extension of the lower limb (decorticate response) and extension of
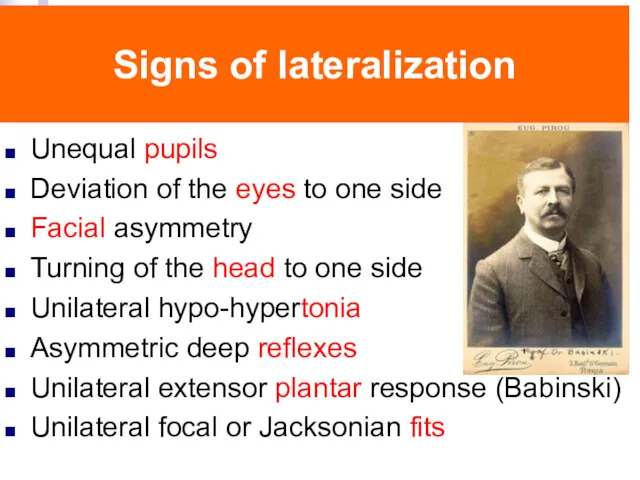
- 51. Signs of lateralization Unequal pupils Deviation of the eyes to one side Facial asymmetry Turning of
- 52. Head and neck The head Evidence of injury Skull should be palpated for depressed fractures. The
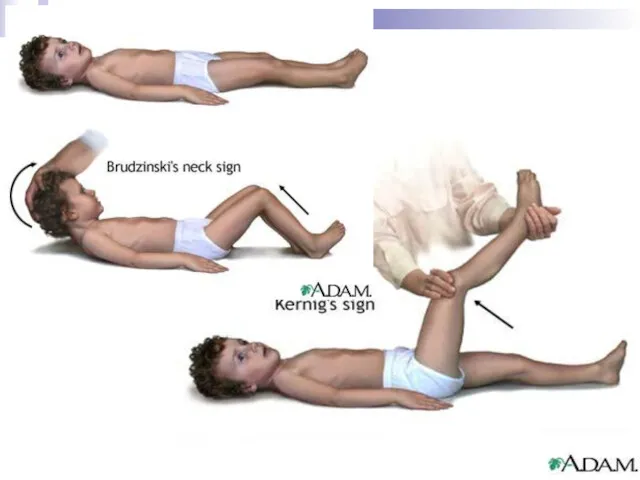
- 53. Neck: In the presence of trauma to the head, associated trauma to the neck should be
- 55. Causes of COMA
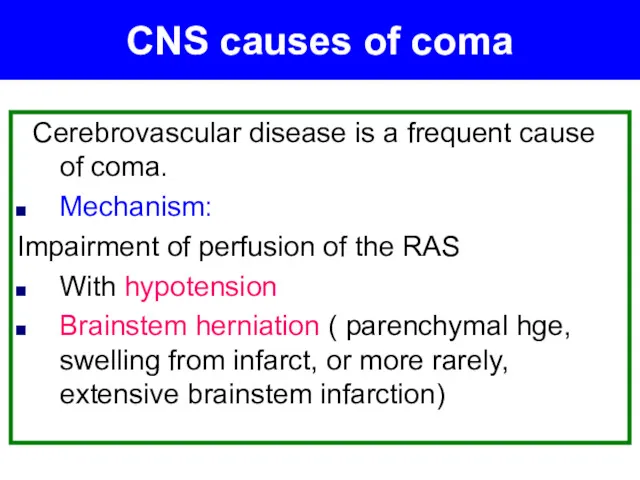
- 56. Cerebrovascular disease is a frequent cause of coma. Mechanism: Impairment of perfusion of the RAS With
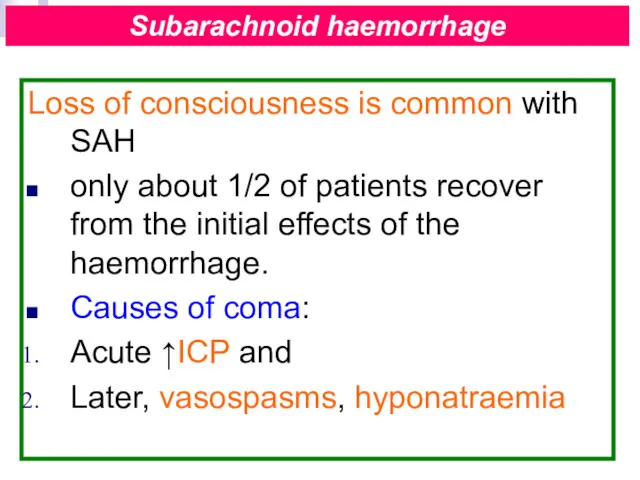
- 57. Loss of consciousness is common with SAH only about 1/2 of patients recover from the initial
- 58. May cause a rapid decline in consciousness, from Rupture into the ventricles or subsequent herniation and
- 59. The critical blood flow in humans required to maintain effective cerebral activity is about 20 ml/100
- 60. Now rare with better control of blood pressure. C/P: impaired consciousness, grossly raised blood pressure, papilloedema.
- 61. Mass effects: tumours, abscesses, haemorrhage, subdural, extradural haematoma, brainstem herniation→ distortion of the RAS. C/P: depends
- 62. Herniation and loss of consciousness Lesions located deeply, laterally, or in the temporal lobes > located
- 63. Central herniation involves downward displacement of the upper brainstem Uncal herniation in which the medial temporal
- 64. Central herniation: small pupils are followed by midpoint pupils, and irregular respiration gives way to hyperventilation
- 65. The leading cause of death below the age of 45, head injury accounts for 1/2 of
- 66. Alcohol on the breath provides a direct clue to a cause of coma, evidence of head
- 67. Damage can be diffuse or focal. Rotational forces of the brain cause surface cortical contusions and
- 68. Diffuse axonal injury is now seen as the major consequence of head injury and associated coma.
- 69. Secondary damage can occur from parenchymal haemorrhage, brain oedema, and vascular dilatation, all of which will
- 70. Systemic infections may result in coma as an event secondary to metabolic and vascular disturbance or
- 71. Diagnosis is confirmed by identifying the changes in the CSF, from which it may be possible
- 72. Parasitic infections Cerebral malaria 25 % mortality rate. Associated with 2–10 % of cases of infection
- 73. Hypoglycaemia and lactic acidosis, which may contribute to the coma. Treatment: intravenous quinine. Steroids, which were
- 74. Septic patients Commonly develop an encephalopathy. In some patients this can be severe, with a prolonged
- 75. Although there is a high mortality, there is the potential for complete reversibility Presence of coma
- 76. Metabolic causes of coma The patient is known to be suffering from liver failure May occur
- 77. Precipitation: GIT hge, infection, certain diuretics, sedatives, analgesics, general anaesthesia, high-protein food or ammonium compounds Subacute
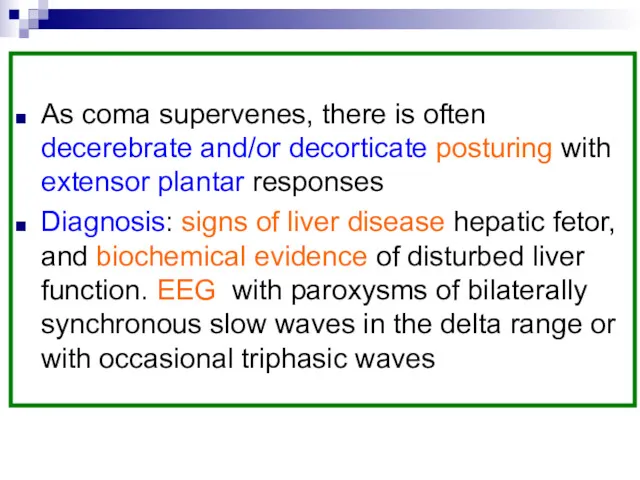
- 79. As coma supervenes, there is often decerebrate and/or decorticate posturing with extensor plantar responses Diagnosis: signs
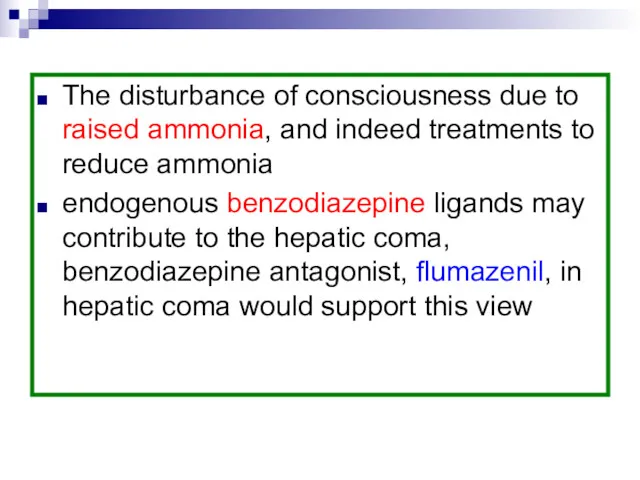
- 80. The disturbance of consciousness due to raised ammonia, and indeed treatments to reduce ammonia endogenous benzodiazepine
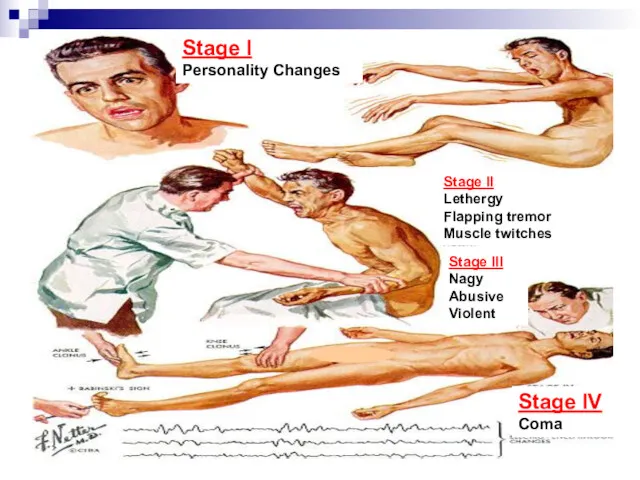
- 81. Stage I Personality Changes Stage II Lethergy Flapping tremor Muscle twitches Stage III Nagy Abusive Violent
- 82. May occur in acute or chronic renal failure Raised blood urea alone cannot be responsible for
- 83. Early symptoms Headache, vomiting, dyspnoea, mental confusion, drowsiness or restlessness, and insomnia Later muscular twitchings, asterixis,
- 84. Dialysis may develop iatrogenic causes of impaired consciousness. Dialysis disequilibrium syndrome Is a temporary, self-limiting disorder,
- 85. accompanied by headache, nausea, vomiting, and restlessness before drowsiness and marked somnolence. It can occur during
- 86. EEG: paroxysmal bursts of irregular, generalized spike and wave activity. has been attributed to the neurotoxic
- 87. Subacute onset with late development of coma. Marked ketoacidosis, usually above 40 mmol/l, together with ketonuria.
- 88. More commonly seen in the elderly. Coma is more common than with ketoacidosis. Profound cellular dehydration,
- 89. Much more rapid onset. Symptoms appear with blood sugars of less than 2.5 mmol/l Initially autonomic:
- 90. Diagnosis of Hypoglycemic Coma: The patient is known to be taking insulin. Spontaneous hypoglycaemia with insulinomas
- 91. Treatment: Glucose, together with thiamine Unless treated promptly, hypoglycaemia results in irreversible brain damage. Cerebellar Purkinje
- 92. Rare cause of coma and is the result of hypoglycaemia, hypotension, hypothermia, and impaired adrenocortical function
- 93. Pituitary apoplexy Acute onset of hypopituitarism occurs with haemorrhagic infarction in pre-existing tumours, patients present with
- 94. Mental symptoms are common, with headaches, poor concentration, and apathy; this is frequently diagnosed as depression.
- 95. Myxoedemic coma has a high mortality and is associated with hypoglycaemia and hyponatraemia. low-reading thermometer to
- 96. Mild mental symptoms: anxiety, restlessness,reduced attention. ‘Thyroid storm’ with agitated delirium, which can progress to coma,
- 97. Mental changes are common in Addison's disease and secondary hypoadrenalism. Undiagnosed Addison's disease is frequently associated
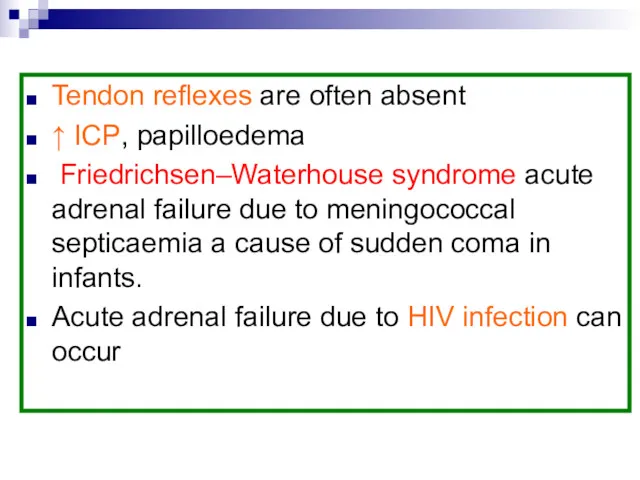
- 98. Tendon reflexes are often absent ↑ ICP, papilloedema Friedrichsen–Waterhouse syndrome acute adrenal failure due to meningococcal
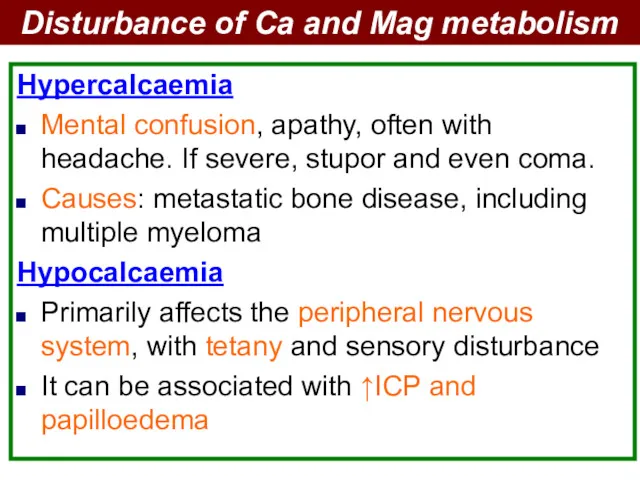
- 99. Hypercalcaemia Mental confusion, apathy, often with headache. If severe, stupor and even coma. Causes: metastatic bone
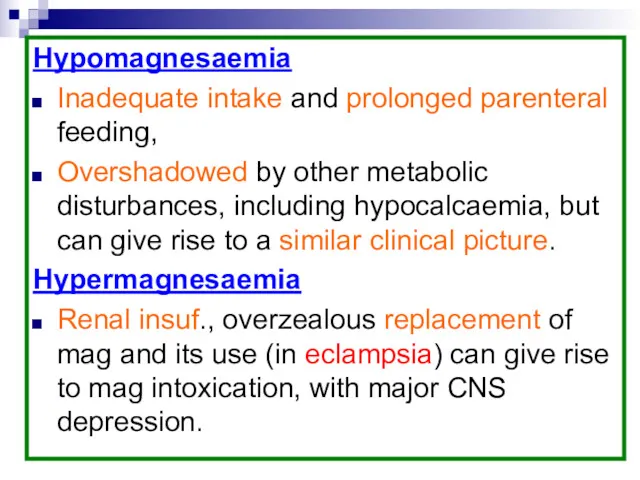
- 100. Hypomagnesaemia Inadequate intake and prolonged parenteral feeding, Overshadowed by other metabolic disturbances, including hypocalcaemia, but can
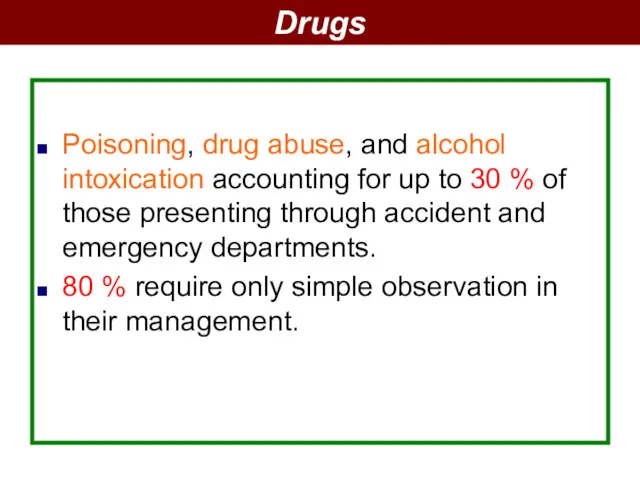
- 101. Poisoning, drug abuse, and alcohol intoxication accounting for up to 30 % of those presenting through
- 102. The most commonly drugs in suicide attempts are : Benzodiazepines Paracetamol antidepressants. Narcotic overdoses (heroin) Pinpoint
- 103. Solvent abuse and glue sniffing should be considered in the undiagnosed patient with coma. Drugs may
- 104. Alcohol intoxication Apparent from the history, flushed face, rapid pulse, and low blood pressure. The smell
- 106. Miscellaneous causes of coma
- 107. Common cause of coma, with a period of unconsciousness following a single generalized seizure commonly lasting
- 108. PMLE severe end-stage multiple sclerosis. Prion disease may lead to coma over a short period of
- 109. In the second half of pregnancy and represents a failure of autoregulation, with raised blood pressure.
- 110. CP: seizures, cortical blindness, and coma. Management: control of convulsions and raised blood pressure. Parental magnesium
- 111. Investigation of coma At presentation blood will be taken for determination of glucose, electrolytes, liver function,
- 112. Following the clinical examination, a broad distinction between a metabolic cause, with preserved pupillary responses, or
- 113. In the absence of focal signs, but with evidence of meningitis, a lumbar puncture may need
- 114. All patients will require chest radiography and ECG, detailed investigations of systemic disease will be directed
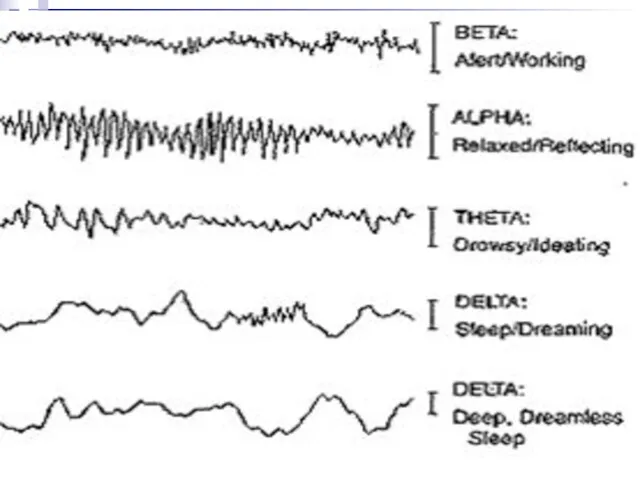
- 115. Fast activity is commonly found with drug overdose and slow wave abnormalities with metabolic and anoxic
- 117. Management of the unconscious patient Treatment of the underlying cause Maintenance of normal physiology: respiration, circulation,
- 118. Intubation, if coma is prolonged, tracheostomy Retention or incontinence of urine will require catheterization Intravenous fluid
- 119. Prognosis in coma In general, coma carries a serious prognosis. This is dependent to a large
- 120. Length of coma and increasing age are of poor prognostic significance. Brainstem reflexes early in the
- 121. The chronic vegetative state usually carries a uniformly poor prognosis, although a partial return of cognition,
- 123. Скачать презентацию
 Физико-химические и технологические свойства порошкообразных лекарственных субстанций
Физико-химические и технологические свойства порошкообразных лекарственных субстанций Этические проблемы клинических областей медицины. (Тема 7)
Этические проблемы клинических областей медицины. (Тема 7) Биожүйелердің электрөткізгіштігі
Биожүйелердің электрөткізгіштігі Гельминтоздардың жалпы эпидемиологиялық сипаттамасы және контагиозды гельминтоздардың эпидемиологиялық процестің сипаттамасы
Гельминтоздардың жалпы эпидемиологиялық сипаттамасы және контагиозды гельминтоздардың эпидемиологиялық процестің сипаттамасы Гастро -эзофагальды рефлюкс ауруларының фармакотерапиясы
Гастро -эзофагальды рефлюкс ауруларының фармакотерапиясы Предотвращение распространения гриппа, острых респираторных вирусных инфекций и коронавирусной инфекции
Предотвращение распространения гриппа, острых респираторных вирусных инфекций и коронавирусной инфекции Миниинвазивные вмешательства в кардио- и ангиохирургии
Миниинвазивные вмешательства в кардио- и ангиохирургии Клінічна фармація в пульмонології
Клінічна фармація в пульмонології Алгоритм диагностики и оказания скорой помощи при гипертензивных кризах
Алгоритм диагностики и оказания скорой помощи при гипертензивных кризах Противомикробные средства. Антисептики и дезинфицирующие средства
Противомикробные средства. Антисептики и дезинфицирующие средства Роль и задачи участкового терапевта по наблюдению за здоровьем подростков
Роль и задачи участкового терапевта по наблюдению за здоровьем подростков Ischemic Colitis
Ischemic Colitis Ўзбекистон Республикасида вирусли гепатитларнинг ташхисоти, давоси ва профилактикаси бўйича чора
Ўзбекистон Республикасида вирусли гепатитларнинг ташхисоти, давоси ва профилактикаси бўйича чора Ломброзо и криминальная антропология
Ломброзо и криминальная антропология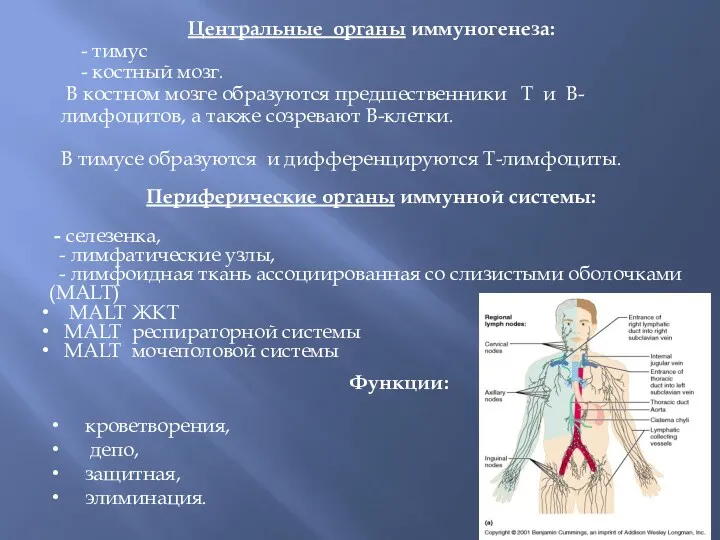 Центральные органы иммуногенеза
Центральные органы иммуногенеза Дорсопатия - дегенеративно-дистрофические заболевания позвоночника и околопозвоночных тканей
Дорсопатия - дегенеративно-дистрофические заболевания позвоночника и околопозвоночных тканей Перша медична допомога
Перша медична допомога Рак кожи
Рак кожи Ауыз қуысы шырышты қабатының анатомо-гистологиялық құрылым ерекшеліктері.терминология, АҚШҚ ауруларының жүйесі
Ауыз қуысы шырышты қабатының анатомо-гистологиялық құрылым ерекшеліктері.терминология, АҚШҚ ауруларының жүйесі Асқазан-ішек диспепсиясын емдеудің негізгі бағыттары
Асқазан-ішек диспепсиясын емдеудің негізгі бағыттары Применение измененной или особой воздушной среды в стоматологии
Применение измененной или особой воздушной среды в стоматологии Risk for a health and ecological risk
Risk for a health and ecological risk Анатомо-фізіологічні особливості розвитку та будови тканин і органів щелепно-лицевої ділянки
Анатомо-фізіологічні особливості розвитку та будови тканин і органів щелепно-лицевої ділянки Лучевая диагностика заболеваний плевры
Лучевая диагностика заболеваний плевры Особенности течения и лечение бронхиальной астмы у беременных
Особенности течения и лечение бронхиальной астмы у беременных Комплексные методы лечения зубочелюстных аномалий. Виды хирургических вмешательств в возрастном аспекте
Комплексные методы лечения зубочелюстных аномалий. Виды хирургических вмешательств в возрастном аспекте Другие синтетические противомикробные средства
Другие синтетические противомикробные средства СД Комарова С.А. 2022
СД Комарова С.А. 2022