Содержание
- 2. Topic: Hypertensive Crisis A hypertensive crisis (HC) is a severe increase in blood pressure that can
- 3. Signs and symptoms of HC may include: Elevated blood pressure Severe headache Severe anxiety SHORTNESS OF
- 4. Life–threatening signs and symptoms of HC: Fluid in lungs (pulmonary edema) Brain swelling or bleeding A
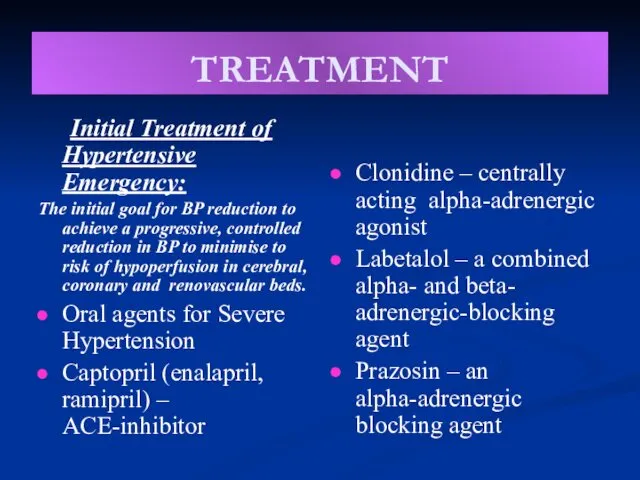
- 5. TREATMENT Initial Treatment of Hypertensive Emergency: The initial goal for BP reduction to achieve a progressive,
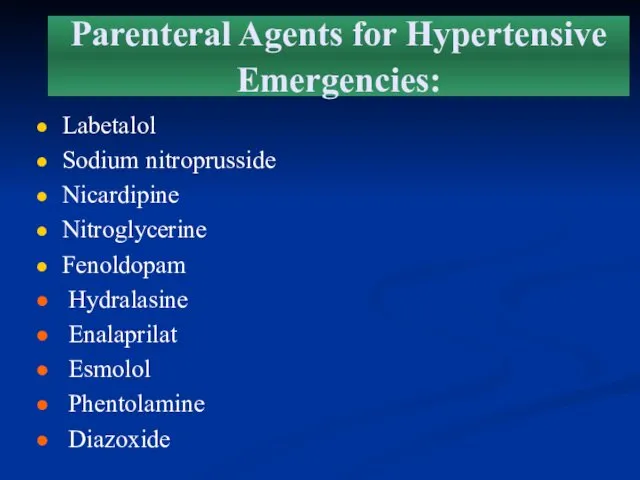
- 6. Parenteral Agents for Hypertensive Emergencies: Labetalol Sodium nitroprusside Nicardipine Nitroglycerine Fenoldopam Hydralasine Enalaprilat Esmolol Phentolamine Diazoxide
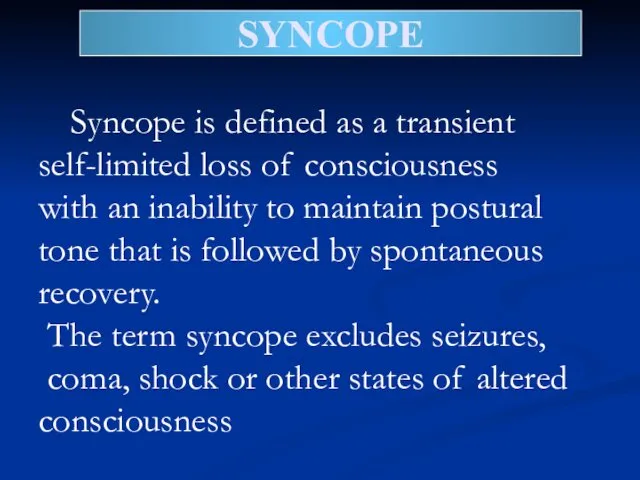
- 7. SYNCOPE Syncope is defined as a transient self-limited loss of consciousness with an inability to maintain
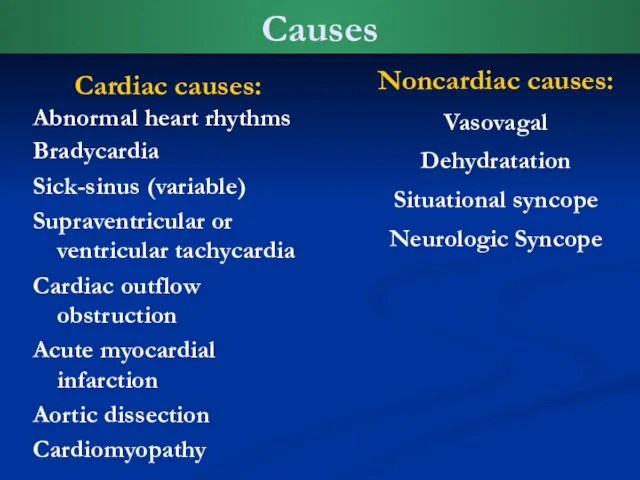
- 8. Causes Cardiac causes: Abnormal heart rhythms Bradycardia Sick-sinus (variable) Supraventricular or ventricular tachycardia Cardiac outflow obstruction
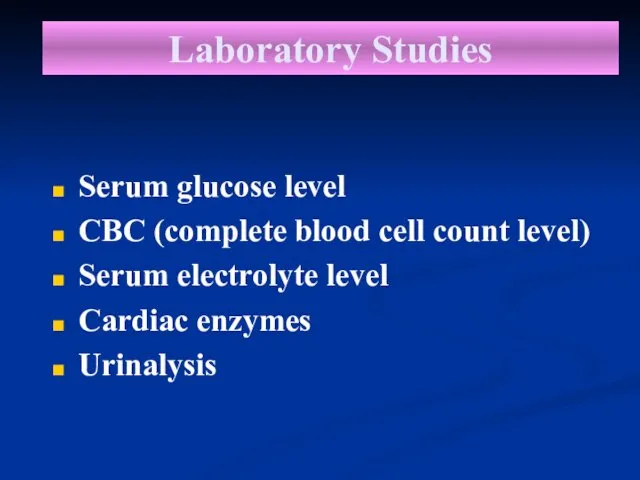
- 9. Laboratory Studies Serum glucose level CBC (complete blood cell count level) Serum electrolyte level Cardiac enzymes
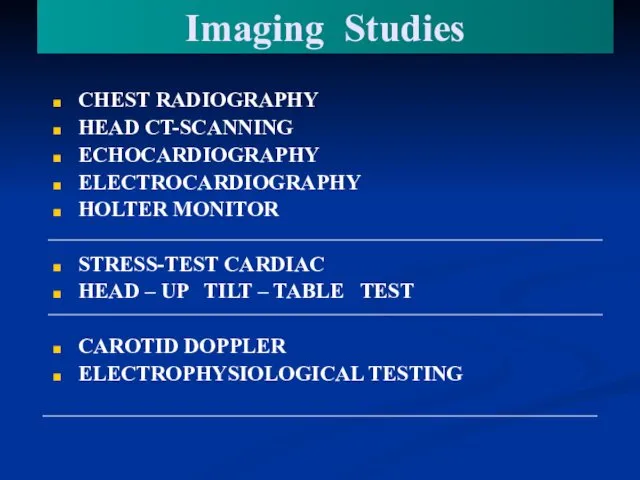
- 10. Imaging Studies CHEST RADIOGRAPHY HEAD CT-SCANNING ECHOCARDIOGRAPHY ELECTROCARDIOGRAPHY HOLTER MONITOR STRESS-TEST CARDIAC HEAD – UP TILT
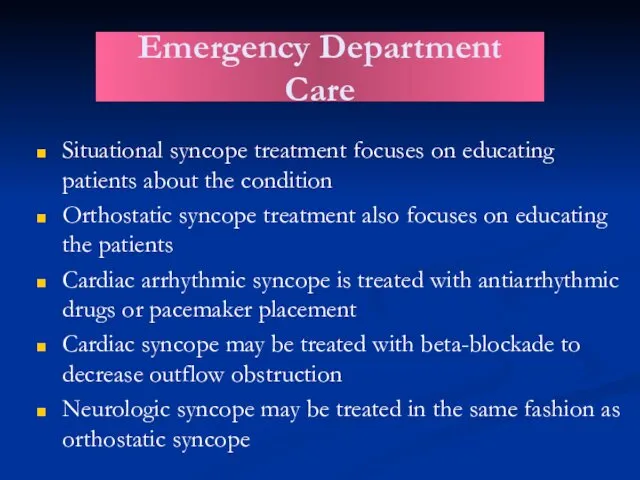
- 11. Situational syncope treatment focuses on educating patients about the condition Orthostatic syncope treatment also focuses on
- 12. Cardiac arrhythmia Cardiac arrhythmia is a term for any of a large and heterogeneous group of
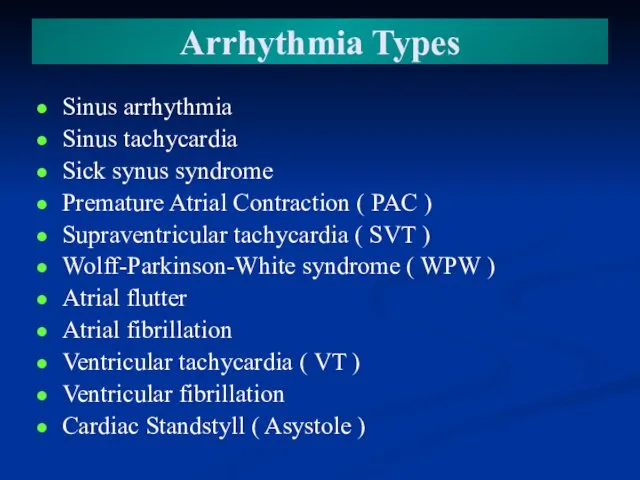
- 13. Arrhythmia Types Sinus arrhythmia Sinus tachycardia Sick synus syndrome Premature Atrial Contraction ( PAC ) Supraventricular
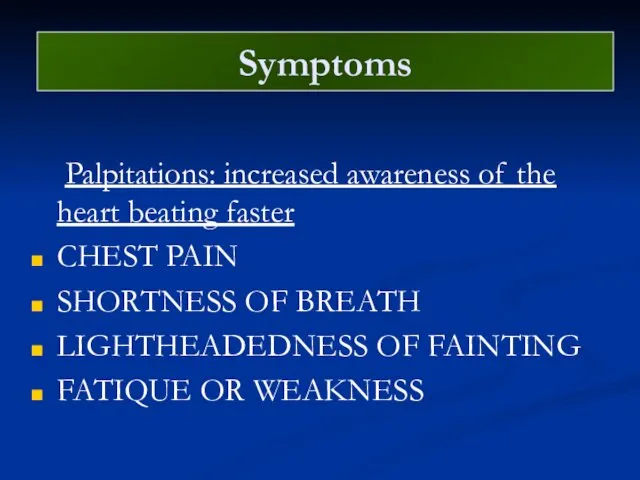
- 14. Symptoms Palpitations: increased awareness of the heart beating faster CHEST PAIN SHORTNESS OF BREATH LIGHTHEADEDNESS OF
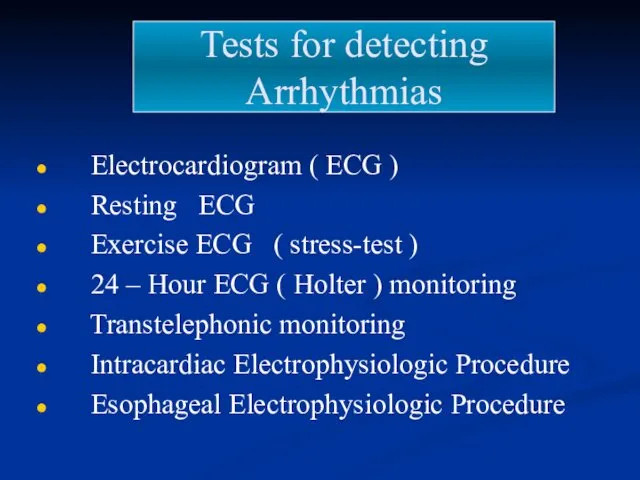
- 15. Tests for detecting Arrhythmias Electrocardiogram ( ECG ) Resting ECG Exercise ECG ( stress-test ) 24
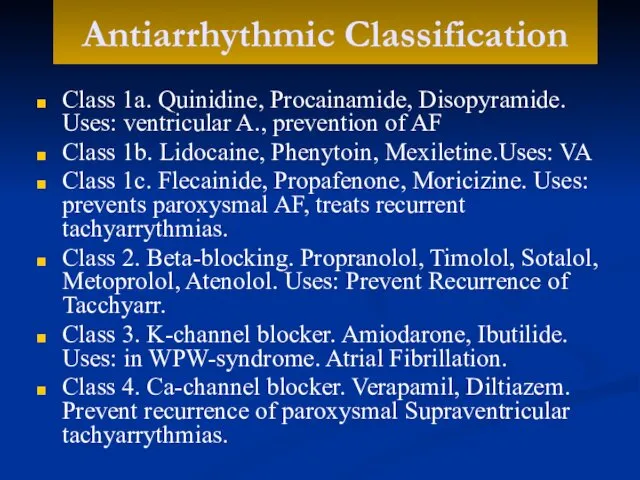
- 16. Antiarrhythmic Classification Class 1a. Quinidine, Procainamide, Disopyramide. Uses: ventricular A., prevention of AF Class 1b. Lidocaine,
- 18. Скачать презентацию
 Таинственные острова математики
Таинственные острова математики Портфолио учителя начальных классов Дудиной Е. А.
Портфолио учителя начальных классов Дудиной Е. А. Приемы и техники массажа. Движение
Приемы и техники массажа. Движение ГСНТИ как информационная система
ГСНТИ как информационная система Характеристика детей, имеющих общее недоразвитие речи.
Характеристика детей, имеющих общее недоразвитие речи. Наша школьная жизнь
Наша школьная жизнь Презентация к дистанционному уроку Типы химических реакций на примере свойств воды. 8 класс
Презентация к дистанционному уроку Типы химических реакций на примере свойств воды. 8 класс Одночлен. 7 класс
Одночлен. 7 класс Презентация Методы и приемы обучения по речевому направлению в ДОУ
Презентация Методы и приемы обучения по речевому направлению в ДОУ Семейный кодекс РФ
Семейный кодекс РФ Artificial Intelligence
Artificial Intelligence Хлебобулочные изделия
Хлебобулочные изделия Токарный станок по дереву. Технология точения конических, фасонных и внутренних поверхностей
Токарный станок по дереву. Технология точения конических, фасонных и внутренних поверхностей Прямоугольный параллелепипед
Прямоугольный параллелепипед Климактерический период в жизни женщины
Климактерический период в жизни женщины Дидактическая игра Волшебный экран
Дидактическая игра Волшебный экран Элементы налогообложения
Элементы налогообложения Структура газообразных, жидких и твердых тел. 5 класс
Структура газообразных, жидких и твердых тел. 5 класс Зонирование территории: типы и рыночный эффект. Лекция 4
Зонирование территории: типы и рыночный эффект. Лекция 4 Архангельская губерния в XIX веке. Освоение Арктики
Архангельская губерния в XIX веке. Освоение Арктики Исход евреев из Египта
Исход евреев из Египта Вирусы и бактериофаги. Неклеточные формы жизни
Вирусы и бактериофаги. Неклеточные формы жизни Визитная карточка МБДОУ № 23 г. Коврова Муниципальное дошкольное образовательное учреждение детский сад № 23 Радуга г. Коврова
Визитная карточка МБДОУ № 23 г. Коврова Муниципальное дошкольное образовательное учреждение детский сад № 23 Радуга г. Коврова Воскресная школа сегодня и завтра
Воскресная школа сегодня и завтра Инвестиция
Инвестиция Социальное государство
Социальное государство Архангельск в годы Великой отечественной войны
Архангельск в годы Великой отечественной войны Буква, строка, текст. Искусство шрифта. (8 класс)
Буква, строка, текст. Искусство шрифта. (8 класс)