Содержание
- 2. Anti-anxiety drugs Prof. Anatoly Kreinin MD, PhD Director of Psychiatric Department, Maale Carmel Mental Health Center,
- 3. תרופות נוגדות חרדה.. Benzodiazepines (BZDs) Buspirone Antihistamines Antidepressants Anti-epileptic drugs (AEDs) Atypical antipsychotics
- 4. תרופות שלא משומשות יותר לחרדה Typical antipsychotics (e.g., thioridazineמלריל -) Barbiturates
- 5. Benzodiazepines (BZDs) The Problem About 2 per cent of the adult population of the US (around
- 6. History of benzodiazepines 1912 phenobarbital 1961 chlordiazepoxide (Librium): 1st BDZ 1963 diazepam 1970 highest level of
- 7. BZD Alprazolam (Xanax) Clonazepam (clonex) Diazepam (Valium,Assival) Lorazepam (Lorivan) Oxazepam (Vaben) Clorazepate (Tranxal) Chlordiazepoxide (Librium)
- 8. History The first benzodiazepine (benzo) was synthesized by an Austrian scientist - Dr. Leo Sternbach in
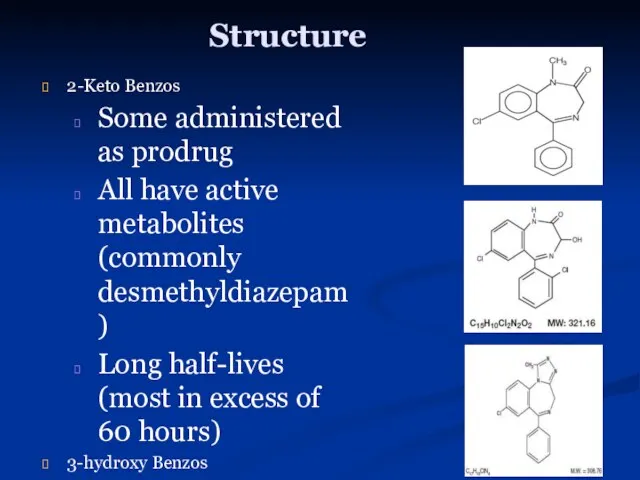
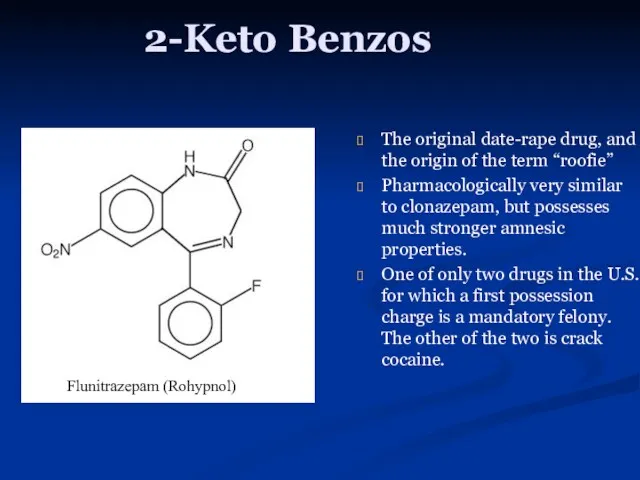
- 9. Structure 2-Keto Benzos Some administered as prodrug All have active metabolites (commonly desmethyldiazepam) Long half-lives (most
- 10. 2-Keto Benzos First isolated benzo Oxidized to desmethyldiazepam in the liver Indicated for treatment of anxiety
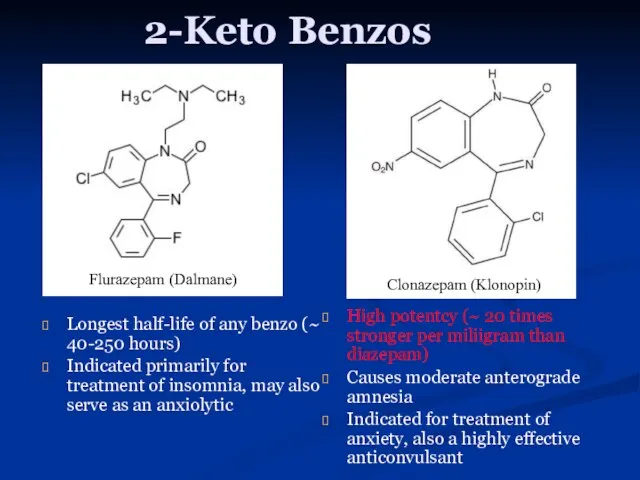
- 11. 2-Keto Benzos Longest half-life of any benzo (~ 40-250 hours) Indicated primarily for treatment of insomnia,
- 12. 2-Keto Benzos The original date-rape drug, and the origin of the term “roofie” Pharmacologically very similar
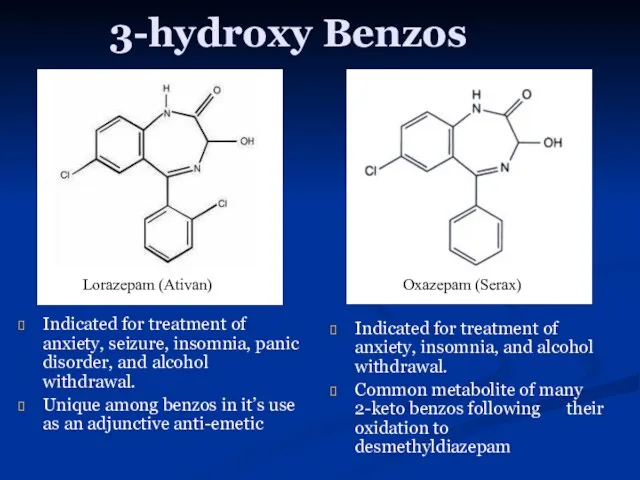
- 13. 3-hydroxy Benzos Indicated for treatment of anxiety, seizure, insomnia, panic disorder, and alcohol withdrawal. Unique among
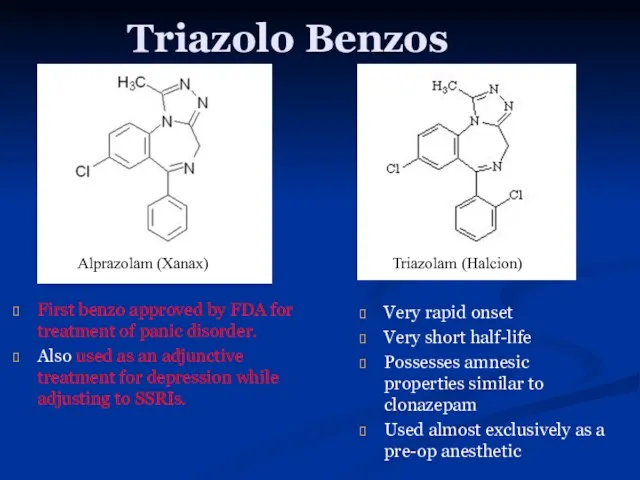
- 14. Triazolo Benzos First benzo approved by FDA for treatment of panic disorder. Also used as an
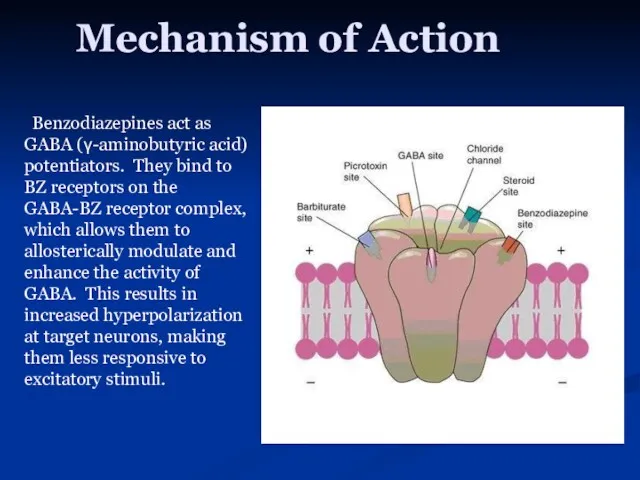
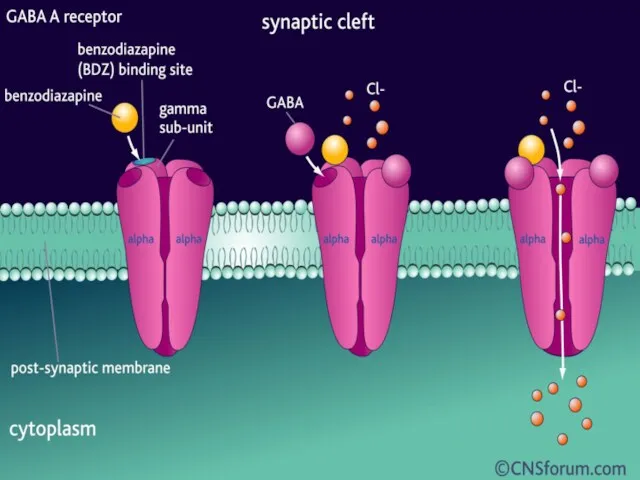
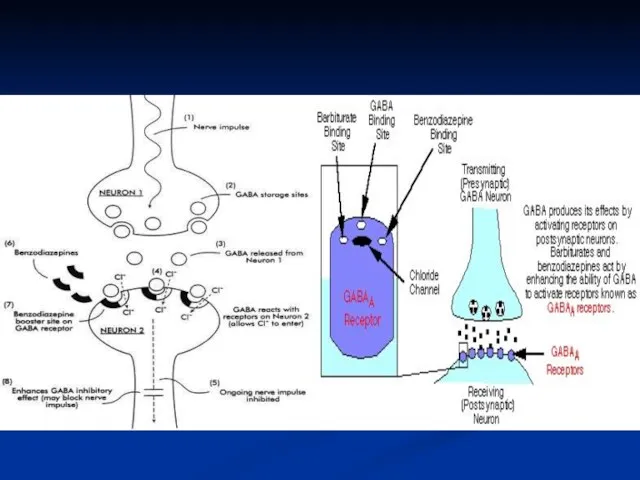
- 15. Mechanism of Action Benzodiazepines act as GABA (γ-aminobutyric acid) potentiators. They bind to BZ receptors on
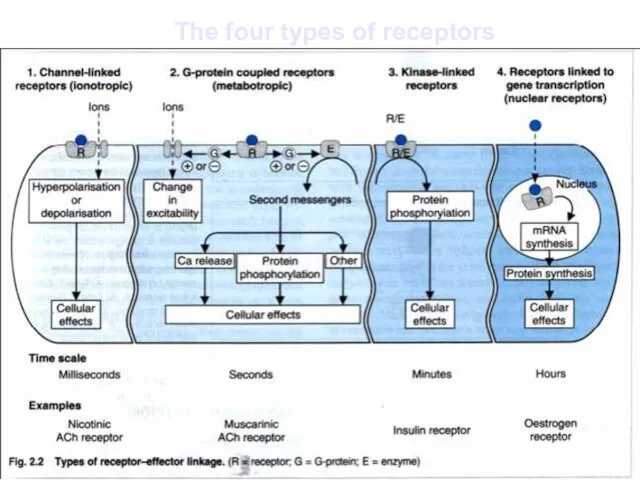
- 18. The four types of receptors
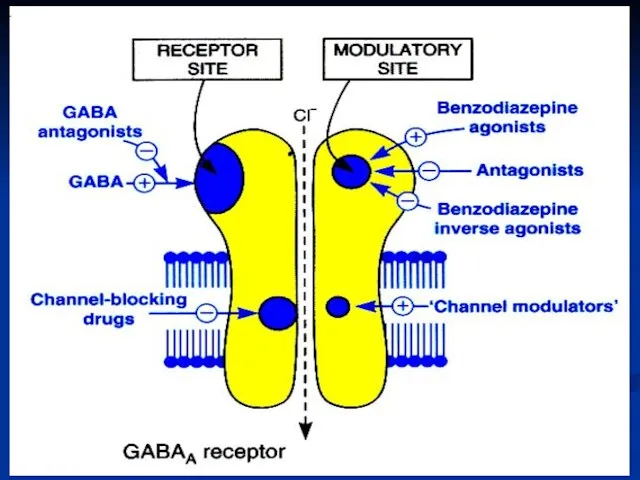
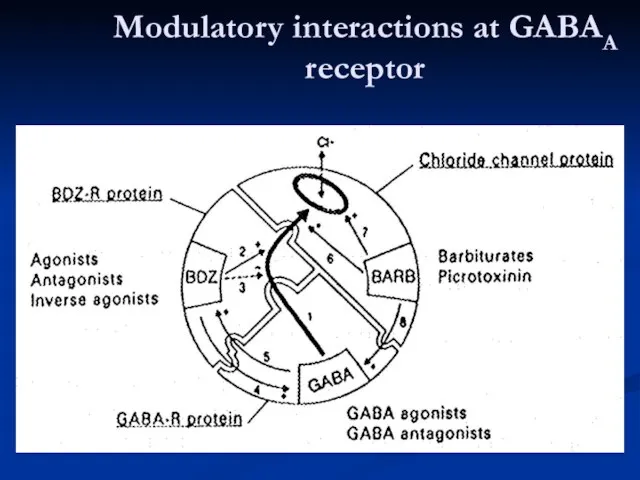
- 20. Modulatory interactions at GABAA receptor
- 21. Benzodiazepines Mechanism of action Increase GABA-mediated inhibition: - spinal cord - cuneate nucleus - cerebellum -
- 22. Clinical Applications Anxiolytic GAD, PTSD, OCD, etc. Panic Disorder Specific Phobias Anticonvulsant Status epilepticus Myoclonic epilepsy
- 23. Benzodiazepines CNS - Antianxiety, sedative - Hypnotic - Amnesic - Anticonvulsant - Muscle relaxant
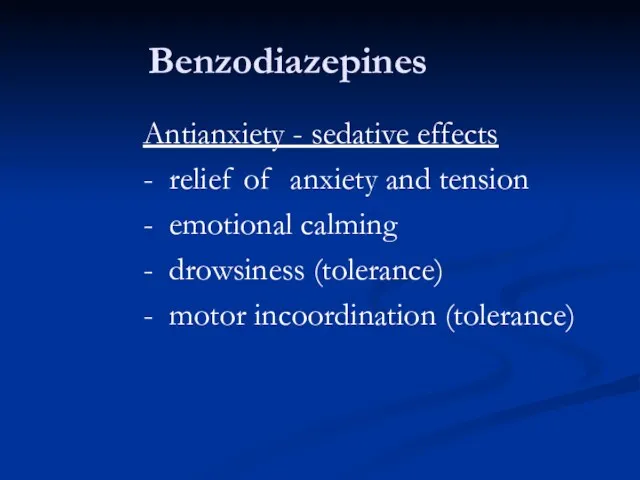
- 24. Benzodiazepines Antianxiety - sedative effects - relief of anxiety and tension - emotional calming - drowsiness
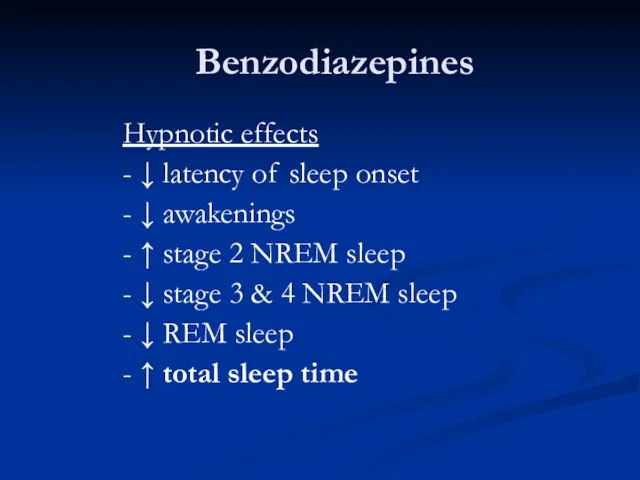
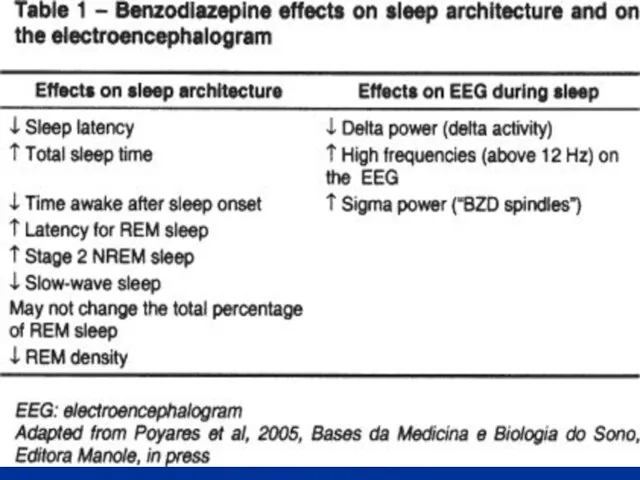
- 25. Benzodiazepines Hypnotic effects - ↓ latency of sleep onset - ↓ awakenings - ↑ stage 2
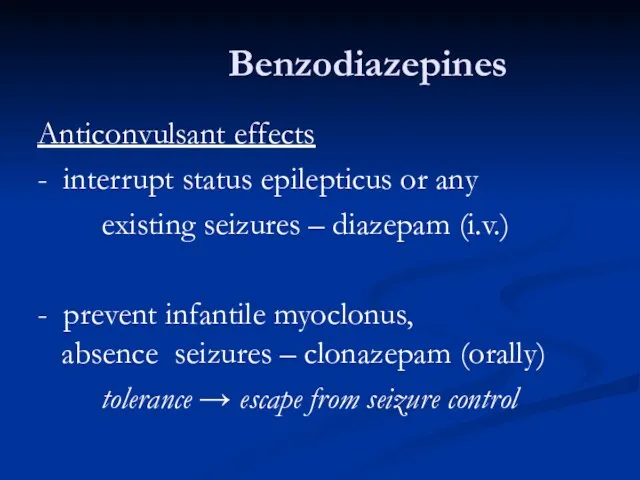
- 27. Benzodiazepines Anticonvulsant effects - interrupt status epilepticus or any existing seizures – diazepam (i.v.) - prevent
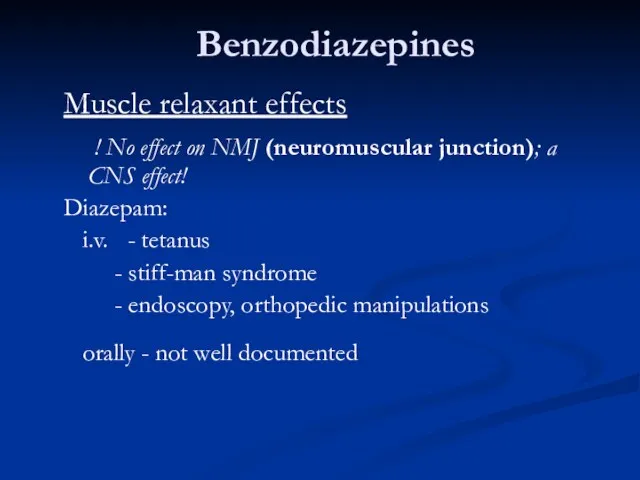
- 28. Benzodiazepines Muscle relaxant effects ! No effect on NMJ (neuromuscular junction); a CNS effect! Diazepam: i.v.
- 29. Benzodiazepines Effects on respiration and cardiovascular system -usually insignificant Preexisting respiratory failure can be aggravated by
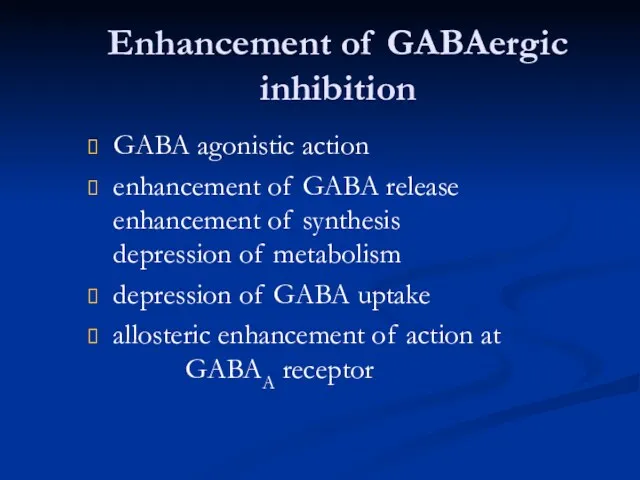
- 30. Enhancement of GABAergic inhibition GABA agonistic action enhancement of GABA release enhancement of synthesis depression of
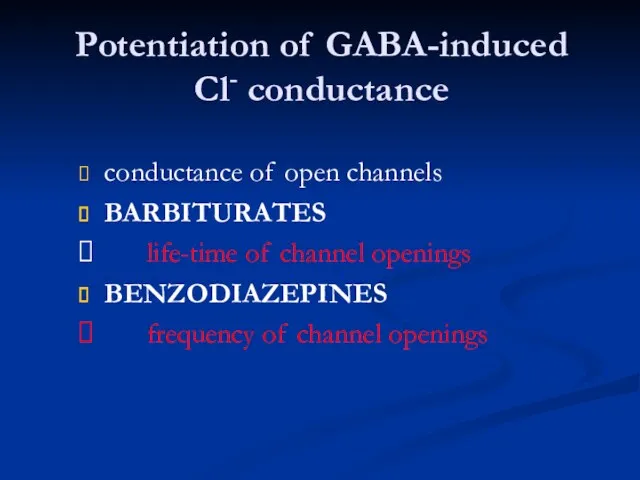
- 31. Potentiation of GABA-induced Cl- conductance conductance of open channels BARBITURATES life-time of channel openings BENZODIAZEPINES frequency
- 32. Benzodiazepines Binding sites - 3H-diazepam binding: saturable, reversible, specific - sites unevenly distributed; parallel to GABAA
- 33. Benzodiazepine binding site ligands Agonists (positive modulators) benzodiazepines Antagonists (null modulators) flumazenil for BZD overdose -
- 34. Future therapeutic trends of benzodiazepine binding site (BDZ R) ligands Drugs for a given binding site
- 35. Benzodiazepine pharmacokinetics Absorption rapid: diazepam, triazolam, flurazepam intermediate: lorazepam slow: oxazepam Plasma protein binding high Distribution
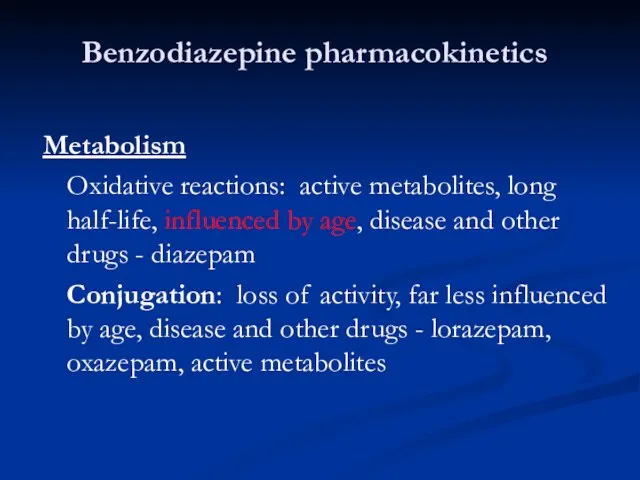
- 36. Benzodiazepine pharmacokinetics Metabolism Oxidative reactions: active metabolites, long half-life, influenced by age, disease and other drugs
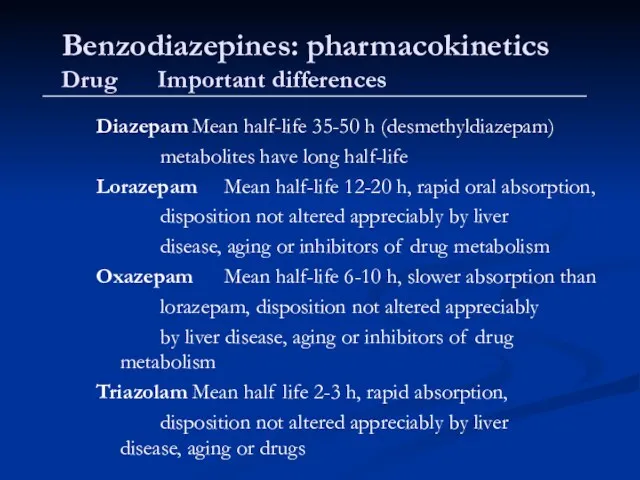
- 37. Benzodiazepines: pharmacokinetics Drug Important differences Diazepam Mean half-life 35-50 h (desmethyldiazepam) metabolites have long half-life Lorazepam
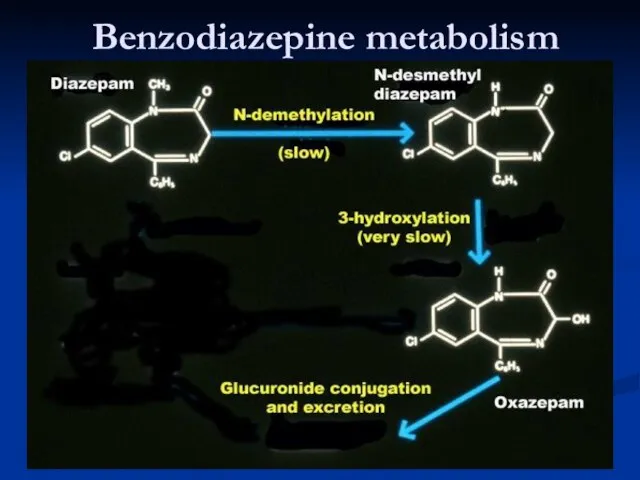
- 38. Benzodiazepine metabolism
- 40. Скачать презентацию


 Нефть и ее роль в мировой экономике
Нефть и ее роль в мировой экономике Химиядан сұрақтар
Химиядан сұрақтар Поверхностный мембранный потенциал. Равновесие Доннана
Поверхностный мембранный потенциал. Равновесие Доннана Свойства НЦ
Свойства НЦ Изомерия в органической химии. Изомеры
Изомерия в органической химии. Изомеры Характеристика спиртов
Характеристика спиртов Неметаллы – простые вещества
Неметаллы – простые вещества Газообразные вещества
Газообразные вещества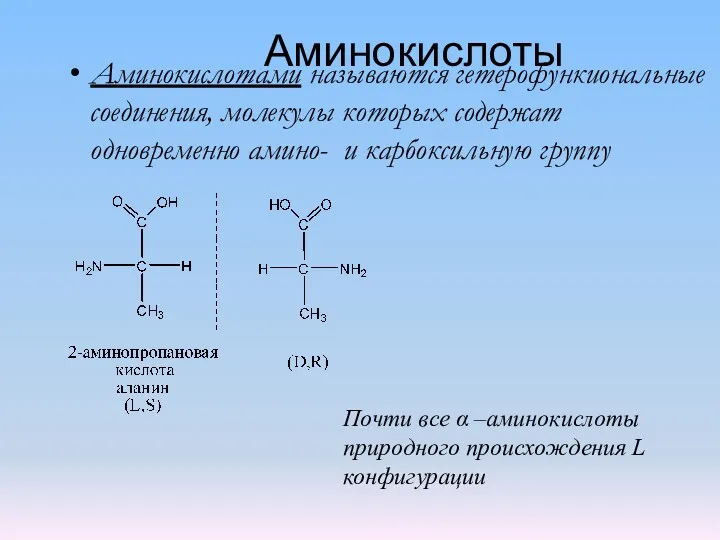 Аминокислоты 1
Аминокислоты 1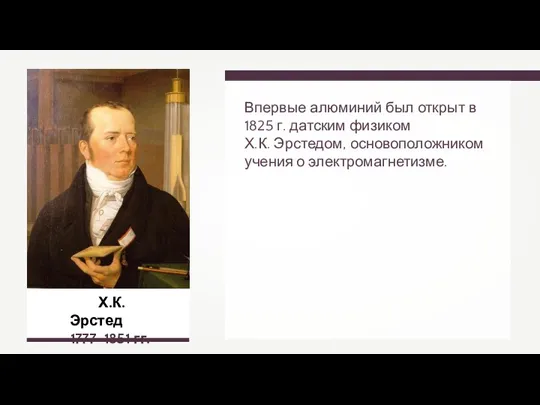 Алюминий
Алюминий Неметаллы. Общая характеристика
Неметаллы. Общая характеристика Реакция горения. Класс 7
Реакция горения. Класс 7 Липиды, биологическая роль, классификация
Липиды, биологическая роль, классификация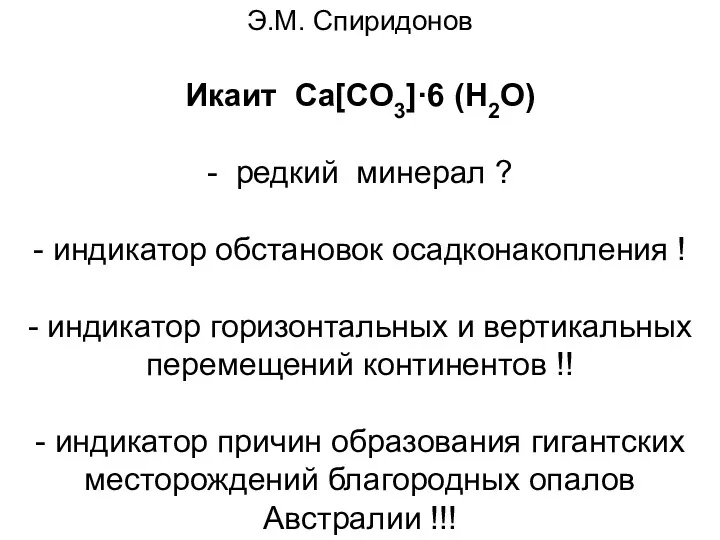 Икаит Ca[CO3]·6 (H2O)
Икаит Ca[CO3]·6 (H2O) 20230219_prezentatsiya_k_uroku_neft
20230219_prezentatsiya_k_uroku_neft Электроизоляционные пластмассы
Электроизоляционные пластмассы V и III группы периодической системы элементов Д.И. Менделеева
V и III группы периодической системы элементов Д.И. Менделеева Мыло. Синтетические моющие средства
Мыло. Синтетические моющие средства Природные источники углеводородов
Природные источники углеводородов Создание пилотной производства 500 тонн в год рафинированного металлургического кремния Si 99,99% для нужд солнечной энергетики
Создание пилотной производства 500 тонн в год рафинированного металлургического кремния Si 99,99% для нужд солнечной энергетики Проведення полімеразної ланцюгової реакції з використанням діагностичних тест-систем
Проведення полімеразної ланцюгової реакції з використанням діагностичних тест-систем Введение в органическую химию
Введение в органическую химию Термодинамика растворов неэлектролитов
Термодинамика растворов неэлектролитов Фракционная перегонка нефти
Фракционная перегонка нефти Термопластические полимеры
Термопластические полимеры Коррозия металлов
Коррозия металлов Подгруппа меди. Элементы 11 группы (Cu,Ag,Au)
Подгруппа меди. Элементы 11 группы (Cu,Ag,Au) Элементы группы галогенов
Элементы группы галогенов